Tisagenlecleucel
Pronunciation: TIS-a-JEN-lek-LOO-sel
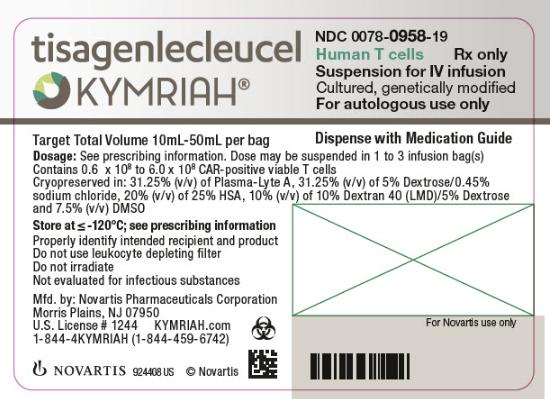
Generic name: tisagenlecleucel
Brand name: Kymriah
Dosage form: suspension for intravenous infusion
Drug class: Miscellaneous antineoplastics
What is tisagenlecleucel?
Tisagenlecleucel is a CAR T-cell treatment sold under the brand name Kymriah, used to treat B-cell precursor acute lymphoblastic leukemia (ALL) aged up to 25 years, or relapsed or refractory large B-cell lymphoma (LBCL) or follicular lymphoma (FL) in adults. It is made from a patient's white blood cells that are collected, modified, and then infused back into the patient.
Tisagenlecleucel is an infusion of T-cells that have been genetically modified in a laboratory to recognize and attach to a specific protein on cancer cells called CD19. Tisagenlecleucel belongs to the drug class called CD19-directed genetically modified autologous T-cell immunotherapy, also known as CAR T-cell therapy (CAR stands for chimeric antigen receptor). It is an individualized, targeted immunotherapy treatment; it is not chemotherapy.
Tisagenlecleucel gained FDA approval on August 30, 2017, under the brand Kymriah. There is no generic or biosimilar.
FDA approvals and indications
Tisagenlecleucel is approved to treat:
- B-cell precursor acute lymphoblastic leukemia (ALL) in children and young adults aged up to 25 years that is refractory or in second or later relapse
- Relapsed or refractory large B-cell lymphoma (LBCL) in adults, after two or more lines of systemic therapy. Includes diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma
- Relapsed or refractory follicular lymphoma (FL) in adults, after two or more lines of systemic therapy.
- This approval is under the accelerated approval designation, and continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s).
Side effects
The most common side effects of tisagenlecleucel are:
- difficulty breathing
- fever (100.4°F/38°C or higher)
- chills and shakes
- confusion
- severe nausea, vomiting, or diarrhea
- muscle or joint pain
- very low blood pressure
- dizziness/lightheadedness
- headache.
Serious side effects and warnings
Tisagenlecleucel carries a Boxed Warning for cytokine release syndrome, neurological toxicities, and secondary hematological cancers.
Cytokine release syndrome (CRS) is a serious side effect of tisagenlecleucel. Tell your caregivers right away if you have any signs or symptoms of this condition, such as a fever, chills, trouble breathing, body aches, vomiting, diarrhea, or feeling light-headed. Your cancer specialist should provide your caregivers with medication to quickly treat CRS if it occurs.
Neurological toxicities. Life-threatening nerve problems can happen with tisagenlecleucel. Tell your caregivers or seek emergency medical attention if you have problems with speech, problems with thinking or memory, confusion, or a seizure.
Secondary hematological cancers. Tisagenlecleucel may increase your risk of getting cancers, including certain types of blood cancers. Your healthcare provider should monitor you for this.
Tisagenlecleucel may also cause the following other serious side effects:
- Serious infections. Tisagenlecleucel can increase the risk of life-threatening infections that may lead to death. Tell your healthcare provider right away if you develop fever, chills, or any signs or symptoms of an infection.
- Low blood cells. Tisagenlecleucel can lower one or more types of blood cells (red blood cells, white blood cells, or platelets). After treatment, your healthcare provider will test your blood to check for this. Tell your healthcare provider right away if you get a fever, are feeling tired, weak, or short of breath, or have bruising or bleeding.
- False-positive HIV test results. Having tisagenlecleucel in your blood may cause a false positive HIV test result in some commercial tests.
- Hypersensitivity (allergic) reactions. These may occur during or following a tisagenlecleucel infusion. Get emergency medical help if you have signs of an allergic reaction, such as hives, difficulty breathing, or swelling of your face, lips, tongue, or throat.
Tell all your healthcare providers that you have received tisagenlecleucel. Your healthcare providers may give you other medicines to treat your side effects.
Tisagenlecleucel is only available through a restricted program called the Kymriah Risk Evaluation and Mitigation Strategy (REMS). Your healthcare provider will order it through a qualified Kymriah Treatment Center.
This is not a complete list of side effects, and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Rituxan
Rituxan infusion is used to treat certain leukemias and lymphomas and some non-cancer conditions ...
Truxima
Truxima is used to treat non-Hodgkin's lymphoma, chronic lymphocytic leukemia, rheumatoid ...
Monjuvi
Monjuvi is used for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) or follicular ...
Breyanzi
Breyanzi is a CAR T cell therapy for large B-cell lymphoma, CLL/SLL, follicular lymphoma, mantle ...
Kymriah
Kymriah is used to treat acute lymphoblastic leukemia (ALL) that is relapsing or refractory in ...
Polivy
Polivy (polatuzumab vedotin-piiq) is a targeted treatment that may be used to treat diffuse large ...
Yescarta
Yescarta is a CAR T-cell treatment used to treat relapsed or refractory large B-cell lymphoma ...
Xpovio
Xpovio is used to treat multiple myeloma (MM) or relapsed/refractory diffuse large B-cell lymphoma ...
Zynlonta
Zynlonta (loncastuximab tesirine) is used to treat relapsed or refractory diffuse large B-cell ...
Before taking
To make sure tisagenlecleucel is safe for you, tell your healthcare providers about all your medical conditions, including if you:
- have hepatitis B or C
- have HIV (human immunodeficiency virus)
- have received a vaccine in the past 2 weeks
- are pregnant or intending to become pregnant
- are breastfeeding.
Pregnancy
Females who can get pregnant may need pregnancy testing before receiving this medicine. You should also take birth control to prevent pregnancy during and shortly after treatment with tisagenlecleucel and chemotherapy.
If you receive tisagenlecleucel during pregnancy, your baby's blood may need to be tested after it is born. This is to evaluate any effects the medicine may have had on the baby.
Breastfeeding
It may not be safe to breastfeed while using tisagenlecleucel. Ask your doctor about any risks.
How is tisagenlecleucel administered?
Tisagenlecleucel is made from your white blood cells, using a process called leukapheresis.
- Your healthcare provider will take some of your blood via an intravenous catheter over about 3 to 6 hours. This process may need to be repeated.
- Your blood cells are frozen and sent to the manufacturing site to make tisagenlecleucel.
It takes about 3-4 weeks from the time your cells are received at the manufacturing site and shipped back to your healthcare provider, but the time may vary.
- While waiting for tisagenlecleucel to be made, your healthcare provider may give you therapy to stabilize your cancer.
- A few days before you are due to receive tisagenlecleucel, your healthcare provider may give you chemotherapy for a few days to prepare your body.
On the day of your infusion, your doctor may give you premedication with acetaminophen and diphenhydramine or another H1-antihistamine approximately 30 to 60 minutes before infusion. Avoid using corticosteroids at any time except in the case of a life-threatening emergency.
- When your body is ready, tisagenlecleucel will be infused through a tube (intravenous catheter) into your vein. This usually takes less than one hour.
You should plan to stay within 2 hours of the location where you received your treatment for at least 4 weeks after getting tisagenlecleucel. Your healthcare provider will check to see if your treatment is working and help you with any side effects that occur.
- Serious and sometimes fatal infections may develop after the injection. Call your doctor right away if you have a fever, chills, easy bruising, unusual bleeding, or other signs of infection.
Dosing information
Dose of Tisagenlecleucel for B-cell precursor ALL (up to 25 years of age)
- 50kg or less: 0.2 to 5.0 x 106 CAR-positive viable T-cells per kg body weight.
- Above 50kg: 0.1 to 2.5 x 108 CAR-positive viable T-cells.
- Suspended in one to three patient-specific infusion bags for intravenous infusion.
Dose of Tisagenlecleucel for relapsed/refractory B-cell lymphoma or follicular lymphoma (Adults)
- 0.6 to 6.0 x 108 CAR-positive viable T-cells.
- Suspended in one to three patient-specific infusion bags for intravenous infusion.
What happens if I miss a dose?
Call your doctor for instructions if you miss any of your chemotherapy treatment, or if you miss a dose of your premedications to prevent side effects of tisagenlecleucel.
What happens if I overdose?
Since this medicine is given by a healthcare professional in a medical setting, an overdose is unlikely to occur.
What should I avoid after receiving tisagenlecleucel?
Do not drive, operate machinery, or partake in hazardous tasks for at least 8 weeks after receiving tisagenlecleucel.
Do not donate blood, an organ, or any tissues or cells from your own body.
Do not receive a "live" vaccine while using tisagenlecleucel, or you could develop a serious infection. Live vaccines include measles, mumps, rubella (MMR), polio, rotavirus, typhoid, yellow fever, varicella (chickenpox), zoster (shingles), and the nasal flu (influenza) vaccine.
What other drugs will affect tisagenlecleucel?
Other drugs may interact with tisagenlecleucel, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all your current medicines and any medicine you start or stop using.
Manufacturer
Novartis Pharmaceuticals Corporation makes tisagenlecleucel under the brand name Kymriah at several specialized facilities around the world, including Morris Plains, New Jersey, USA.
Tisagenlecleucel Biosimilars
Biosimilar and interchangeable products are biological products that are highly similar to and have no clinically meaningful differences from the reference product.
Reference products
These are biological products that have already been approved by the FDA, against which biosimilar products are compared. There is 1 for tisagenlecleucel.
Kymriah (tisagenlecleucel) - Novartis Pharmaceuticals Corporation
| Formulation type | Strength |
|---|---|
| Bag | 0.6 to 6.0 x 10^8 CAR-POSITIVE VIABLE T CELLS |
View Kymriah information in detail.
Popular FAQ
What type of drug is Kymriah (tisagenlecleucel)?
Kymriah (tisagenlecleucel) is a chimeric antigen receptor T cell (CAR-T) therapy. In CAR-T cell therapy, a patient's cells are genetically modified to include a new protein that directs that specific white blood cell (known as T-cell) to target and kill leukemia cells. Continue reading
References
More about tisagenlecleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.