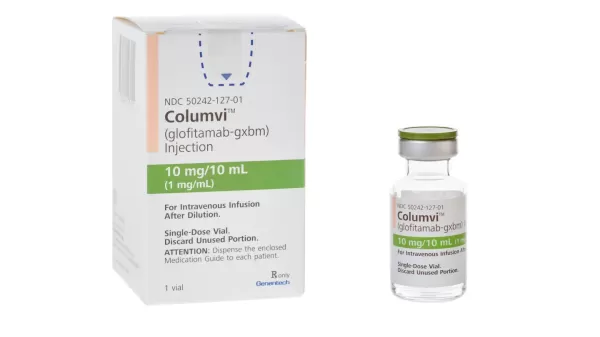
Columvi
Pronunciation: ko-loom-vee
Generic name: glofitamab-gxbm
Dosage form: injection for intravenous infusion
Drug class: Bispecific T-cell engagers (BiTE)
What is Columvi?
Columvi is used to treat certain types of diffuse large B-cell lymphoma (DLBCL) or large B-cell lymphoma (LBCL) in adults. It is administered via an IV infusion (an infusion into a vein).
Clinical trials have reported Columvi (glofitamab) is effective for B-cell lymphomas with an overall response rate of 56% and a complete response rate of 43%. A response rate of 9 months or longer was reported by 68.5% of patients (median duration of response, 18.4 months).
Uses and FDA approvals
Columvi is a prescription medicine FDA-approved for adults with:
- relapsed or refractory diffuse large B-cell lymphoma, not otherwise specified (DLBCL, NOS)
- large B-cell lymphoma (LBCL) arising from follicular lymphoma, after 2 or more lines of systemic therapy.
It is not known if this medicine is safe and effective in children.
Columvi gained FDA approval on June 15, 2023, under the accelerated approval designation. There is no generic.
- Continued approval may be dependent upon a continued benefit being shown in clinical trials.
How does Columvi work?
Columvi has a bispecific mechanism of action and binds to 2 different immune system targets: the CD20 protein on B cells and the CD3 protein on T cells. This brings T cells into proximity to B cells, making them more effective at killing cancerous B cells.
Columvi belongs to the drug class called Bispecific T-cell engagers (BiTE).
Columvi side effects
The most common side effects of Columvi are:
- Cytokine release syndrome (CRS, see below)
- Muscle and bone pain
- A rash
- Fatigue or tiredness
- Laboratory abnormalities (such as decreased white cells, lower phosphate levels, increased uric acid levels, and decreased fibrinogen).
Serious side effects and warnings
Columvi carries a Boxed Warning for cytokine release syndrome.
Cytokine Release Syndrome (CRS). Columvi can cause CRS, a serious side effect that is common during treatment and can also be serious and lead to death. Call your healthcare provider or get emergency medical help right away if you develop any signs or symptoms of CRS, including:
- fever of 100.4°F (38°C) or higher
- chills or shaking
- fast or irregular heartbeat
- dizziness or light-headedness
- trouble breathing
- shortness of breath.
Due to the risk of CRS, you will receive Columvi on a “step-up dosing schedule”.
- A single dose of a medicine called obinutuzumab (Gazyva) will be given to you on the first day of your first treatment cycle (Day 1 of Cycle 1).
- You will start the Columvi step-up dosing schedule a week after the obinutuzumab dose. The step-up dosing schedule is when you receive smaller “step-up” doses of Columvi on Day 8 and Day 15 of Cycle 1.
- This is to help reduce your risk of CRS. You should be hospitalized during your infusion and for 24 hours after receiving the first step-up dose on Day 8.
- You should be hospitalized during your infusion and for 24 hours after receiving the second step-up dose on Day 15 if you experienced CRS during the first step-up dose.
You will receive your first full dose of Columvi a week after the second step-up dose (this will be Day 1 of Cycle 2).
- If your dose of Columvi is delayed for any reason, you may need to repeat the “step-up dosing schedule”.
- If you had more than mild CRS with your previous dose of Columvi, you should be hospitalized during and for 24 hours after receiving your next dose of Columvi.
Before each dose of Columvi, you will receive medicines to help reduce your risk of CRS and infusion-related reactions.
- Your healthcare provider will monitor you for CRS during treatment with Columvi and may treat you in a hospital if you develop signs and symptoms of CRS. Your healthcare provider may temporarily stop or completely stop your treatment with Columvi if you have severe side effects.
Carry the Columvi Patient Wallet Card with you at all times and show it to all of your healthcare providers.
- The Columvi Patient Wallet Card lists the signs and symptoms of CRS you should get emergency medical help for right away.
Neurologic problems. Columvi can cause serious neurologic problems that may lead to death. Your healthcare provider will monitor you for neurologic problems during treatment with Columvi. Your healthcare provider may also refer you to a healthcare provider who specializes in neurologic problems. Tell your healthcare provider right away if you develop any signs or symptoms of neurologic problems, including:
- headache
- confusion and disorientation
- difficulty paying attention or understanding things
- trouble speaking
- sleepiness
- memory problems
- numbness, tingling, or weakness of the hands or feet
- dizziness
- shaking (tremors).
Serious infections. Columvi can cause serious infections that may lead to death. Your healthcare provider will monitor you for signs and symptoms of infection and treat you as needed. Tell your healthcare provider right away if you develop any signs of infection, including fever, chills, weakness, cough, shortness of breath, or sore throat.
Growth in your tumor or worsening of tumor-related problems (tumor flare). Tell your healthcare provider if you get any of these signs or symptoms of tumor flare:
- tender or swollen lymph nodes
- pain or swelling at the site of the tumor
- chest pain
- cough
- trouble breathing.
Your healthcare provider may temporarily stop or completely stop treatment with Columvi if you develop certain side effects.
These are not all the possible side effects of Columvi. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Before taking
Before receiving Columvi, tell your healthcare provider about all of your medical conditions, including if you:
- have an infection
- have kidney problems
- are pregnant or plan to become pregnant
- are breastfeeding or plan to breastfeed.
Pregnancy
Columvi may harm your unborn baby. Females who can become pregnant:
- Your healthcare provider should do a pregnancy test before you start treatment with Columvi.
- You should use effective birth control (contraception) during treatment and for 1 month after your last dose of Columvi. Talk to your healthcare provider about what birth control method is right for you during this time.
Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with Columvi.
Breastfeeding
It is not known if Columvi passes into your breastmilk. Do not breastfeed during treatment and for 1 month after your last dose of Columvi.
How will I receive Columvi?
Columvi will be given to you by your healthcare provider by infusion through a needle placed in your vein (intravenous infusion).
- You should be well-hydrated before receiving treatment.
Your Columvi treatment schedule is divided into cycles that are 21 days (3 weeks) long.
- On Day 1 of Cycle 1, your healthcare provider will give you a single dose of a medicine called obinutuzumab by intravenous infusion.
- You will then receive Columvi on Day 8 and Day 15 of Cycle 1.
- Starting with Cycle 2, you will receive Columvi 1 time every three weeks.
- Your healthcare provider will decide how many treatment cycles you will receive of Columvi
Before each dose of Columvi, you will be given premedication to reduce the risk of CRS.
After your infusion, you will be monitored for nerve damage, infection, and tumor flare reactions.
What should I avoid while receiving Columvi?
Do not drive, operate heavy machinery, or do other dangerous activities if you develop dizziness, confusion, shaking (tremors), sleepiness, or any other symptoms that impair consciousness until your signs and symptoms go away. These may be signs and symptoms of neurologic problems.
What other drugs will affect Columvi?
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
- Columvi causes the release of cytokines that may suppress the activity of CYP enzymes, resulting in higher concentrations of the many other medications that are broken down by these enzymes.
- This is most likely to happen after the first dose of Columvi on Cycle 1 and up to 14 days after the first 30 mg dose on Cycle 2. It can also happen during and after CRS.
Columvi injection ingredients
Active ingredient: glofitamab-gxbm
Inactive ingredients: histidine, histidine hydrochloride monohydrate, methionine, polysorbate 20, sucrose, and Water for injection.
Available in two strengths:
- Columvi 2.5 mg/2.5 mL (1 mg/mL) in a single-dose vial
- Columvi 10 mg/10 mL (1 mg/mL) in a single-dose vial.
The injection is preservative-free and should be colorless and clear.
Manufacturer
Columvi injection is manufactured by Genentech Inc., a member of the Roche group. Roche's global headquarters are located in Basel, Switzerland. Some other notable medicines manufactured by Roche include:
- Ocrevus (ocrelizumab) for multiple sclerosis
- Tecentriq (atezolizumab) for various types of cancer
- Actemra (tocilizumab) for rheumatoid arthritis and other inflammatory conditions
- Herceptin (trastuzumab) for HER2-positive breast cancer
- Avastin (bevacizumab) for various cancers.
Columvi Biosimilars
Biosimilar and interchangeable products are biological products that are highly similar to and have no clinically meaningful differences from the reference product.
Reference products
These are biological products that have already been approved by the FDA, against which biosimilar products are compared. There is 1 for Columvi.
Columvi (glofitamab-gxbm) - Genentech, Inc.
| Formulation type | Strength |
|---|---|
| Single-Dose Vial | 10 mg/10 mL (1 mg/mL) |
| Single-Dose Vial | 2.5 mg/2.5 mL (1 mg/mL) |
Popular FAQ
What are Monoclonal Antibodies and how do they work?
Monoclonal antibodies (mAbs) are man-made proteins that mimic the natural antibodies produced by our immune systems. Monoclonal antibodies can be formulated into medicines to treat various types of illnesses, such as cancer, rheumatoid arthritis or psoriasis.
Continue readingWhat is glofitamab?
Glofitamab-gxbm is an immunotherapy treatment that may be used to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified or large B-cell lymphoma arising from follicular lymphoma, after at least 2 lines of systemic therapy. It is approved under the name Columvi. Continue reading
References
More about Columvi (glofitamab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: bispecific T-cell engagers (BiTE)
- Breastfeeding
- En español
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.