Tisagenlecleucel Dosage
Medically reviewed by Drugs.com. Last updated on Mar 5, 2025.
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Acute Lymphoblastic Leukemia
Prior to infusing this drug:
Lymphodepleting chemotherapy: Fludarabine (30 mg/m2 IV daily for 4 days) and cyclophosphamide (500 mg/m2 IV daily for 2 days starting with the first dose of fludarabine); infuse tisagenlecleucel 2 to 14 days after completion of the lymphodepleting chemotherapy.
Tisagenlecleucel:
Up to 25 years:
Body weight 50 kg or less: 0.2 to 5 x 10(6) chimeric antigen receptor (CAR)-positive viable T cells per kg of body weight
Body weight above 50 kg: 0.1 to 2.5 x 10(8) CAR-positive viable T cells
Comments:
- Base the dosage on the patient's weight at the time of leukapheresis.
- Administer this drug via IV infusion within 30 minutes of thawing at 10 to 20 mL per minute (adjusted as appropriate for smaller children and smaller volumes); the infusion bag volume ranges from 10 to 50 mL.
- Pre-medicate patients with acetaminophen and diphenhydramine or another H1-antihistamine approximately 30 to 60 minutes prior to infusion of this drug; avoid using corticosteroids at any time except in the case of a life-threatening emergency.
Use: For patients up to 25 years with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
Usual Adult Dose for Lymphoma
Prior to infusing this drug:
- Lymphodepleting chemotherapy: Fludarabine (25 mg/m2 IV daily for 3 days) and cyclophosphamide (250 mg/m2 IV daily for 3 days starting with the first dose of fludarabine)
- Alternate lymphodepleting chemotherapy: Bendamustine 90 mg/m2 IV daily for 2 days if a patient experienced a previous Grade 4 hemorrhagic cystitis with cyclophosphamide or demonstrates resistance to a previous cyclophosphamide containing regimen; infuse tisagenlecleucel 2 to 11 days after completion of the lymphodepleting chemotherapy.
- Lymphodepleting chemotherapy may be omitted if a patient's white blood cell (WBC) count is less than or equal to 1 x 10(9)/L within 1 week prior to tisagenlecleucel infusion.
Dose: 0.6 to 6 x 10(8) CAR-positive viable T cells
Use: For adult patients with relapsed or refractory (r/r) large B-cell lymphoma after 2 or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma (NOTE: This drug not indicated for treatment of patients with primary central nervous system lymphoma).
Usual Pediatric Dose for Acute Lymphoblastic Leukemia
Prior to infusing this drug:
Lymphodepleting chemotherapy: Fludarabine (30 mg/m2 IV daily for 4 days) and cyclophosphamide (500 mg/m2 IV daily for 2 days starting with the first dose of fludarabine); infuse tisagenlecleucel 2 to 14 days after completion of the lymphodepleting chemotherapy.
Up to 25 years:
- Body weight 50 kg or less: 0.2 to 5 x 10(6) chimeric antigen receptor (CAR)-positive viable T cells per kg of body weight
- Body weight above 50 kg: 0.1 to 2.5 x 10(8) CAR-positive viable T cells
Comments:
- Base the dosage on the patient's weight at the time of leukapheresis.
- Administer this drug via IV infusion within 30 minutes of thawing at 10 to 20 mL per minute (adjusted as appropriate for smaller children and smaller volumes); the infusion bag volume ranges from 10 to 50 mL.
- Pre-medicate patients with acetaminophen and diphenhydramine or another H1-antihistamine approximately 30 to 60 minutes prior to infusion of this drug; avoid using corticosteroids at any time except in the case of a life-threatening emergency.
Use: For patients up to 25 years with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse
Renal Dose Adjustments
Data not available
Liver Dose Adjustments
Data not available
Dose Adjustments
MANAGEMENT OF CYTOKINE RELEASE SYNDROME (CRS): Identify CRS based on clinical presentation; evaluate and treat other causes of fever, hypoxia, and hypotension.
If CRS is Suspected, Treat Based on CRS Severity:
- Prodromal Syndrome (low-grade fever, fatigue, anorexia): Observe in person; exclude infection; administer antibiotics per local guidelines if neutropenic; provide symptomatic support.
- Overt CRS (one or more of the following: high fever, hypoxia, mild hypotension): Administer antipyretics, oxygen, IV fluids, and/or low-dose vasopressors as needed.
Severe or Life-Threatening CRS (one or more of the following: hemodynamic instability despite IV fluids and vasopressor support; worsening respiratory distress including pulmonary infiltrates, increasing oxygen requirement including high-flow oxygen and/or need for mechanical ventilation; rapid clinical deterioration):
- Administer high dose or multiple vasopressors, oxygen, mechanical ventilation, and/or other supportive care as needed.
- Administer tocilizumab: 12 mg/kg IV over 1 hour (if patient weighs less than 30 kg) OR 8 mg/kg IV over 1 hour (maximum dose: 800 mg; if patient weighs 30 kg or greater).
Resistant CRS (no clinical improvement in 12 to 18 hours, or worsening at any time despite prior management):
- Administer multiple vasopressors, oxygen, mechanical ventilation, and/or other supportive care as needed.
- Administer methylprednisolone 2 mg/kg as an initial dose, then 2 mg/kg per day until vasopressors and high-flow oxygen are no longer needed, then taper quickly.
- If no response to steroids within 24 hours, repeat the administration of tocilizumab at 12 mg/kg IV over 1 hour (if patient weighs less than 30 kg) OR 8 mg/kg IV over 1 hour (maximum dose: 800 mg; if patient weighs 30 kg or greater).
- If no response to the second dose of tocilizumab within 24 hours, consider a third dose of tocilizumab or pursue alternative measures for CRS treatment.
Precautions
The US FDA requires a Risk Evaluation and Mitigation Strategy (REMS) for tisagenlecleucel. It includes elements to assure safe use. For additional information: www.accessdata.fda.gov/scripts/cder/rems/index.cfm.
US BOXED WARNINGS:
- CYTOKINE RELEASE SYNDROME (CRS): CRS reactions, including fatal reactions, occurred in patients receiving this drug.
- Do not administer this drug to patients with active infection or inflammatory disorders.
- Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids.
- NEUROLOGICAL TOXICITIES: Neurological toxicities, which may be life-threatening, can occur following therapy with this drug and may occur concurrently with CRS.
- Monitor for neurological events after treatment with this drug, and provide supportive care as needed.
CONTRAINDICATIONS:
- None
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration Advice:
- Delay the infusion of this drug if a patient has unresolved serious adverse reactions (e.g., pulmonary reactions, cardiac reactions, hypotension) from preceding chemotherapies, active uncontrolled infection, active graft versus host disease (GVHD), or worsening of leukemia burden following lymphodepleting chemotherapy.
- Do not wash, spin down, and/or re-suspend this drug in new media prior to infusion.
- Consult the manufacturer product information for additional administration instructions.
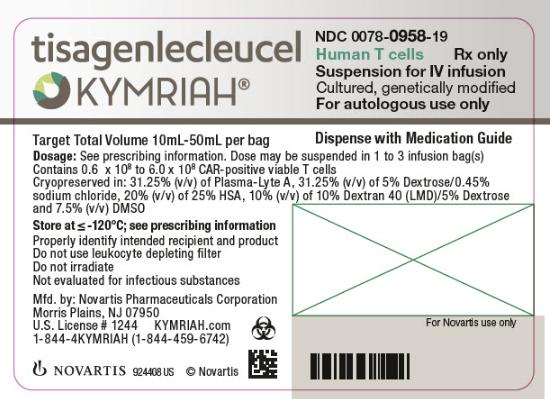
Storage Requirements:
- This drug is supplied as a frozen suspension in one infusion bag; store the bag in the vapor phase of liquid nitrogen (minus 120 degrees Celsius or less) in a temperature-monitored system.
- May store this drug at room temperature (20 to 25 degrees Celsius) for up to 30 minutes once it has been thawed.
Preparation/Handling Techniques:
- Refer to the manufacturer product information for thawing and drug infusion preparation instructions.
- Employ universal precautions to avoid potential transmission of infectious diseases when handling this drug.
General:
- Lymphodepleting chemotherapy consists of fludarabine (30 mg/m2 IV daily for 4 days) and cyclophosphamide (500 mg/m2 IV daily for 2 days starting with the first dose of fludarabine).
- This drug contains human cells genetically modified with a lentivirus, and is prepared from autologous blood collected by leukapheresis.
- This drug is for autologous and IV use only.
Monitoring:
- Hepatic: Screening for HBV, HCV, and HIV (before collection of cells for manufacturing)
- Immunologic: Signs/symptoms of cytokine release syndrome (at least 4 weeks after treatment); immunoglobulin levels (after treatment)
- Infections/infestations: Signs/symptoms of infection (after treatment)
- Nervous system: Neurological events (after treatment)
- Oncologic: Secondary malignancies (life-long)
Patient Advice:
- Avoid potentially dangerous activities such as driving and operating machinery until you know how this drug affects you.
Frequently asked questions
More about tisagenlecleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (3)
- Side effects
- During pregnancy
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.