Misoprostol (Monograph)
Brand name: Cytotec
Drug class: Prostaglandins
ATC class: A02BB01
VA class: GA309
Chemical name: 11α,13E)-(±)-11,16-Dihydroxy-16-methyl-9-oxo-prost-13-en-1-oic acid methyl ester
Molecular formula: C22H38O5
CAS number: 59122-46-2
Warning
-
May cause serious fetal harm (e.g., birth defects, abortion, premature birth, uterine rupture).1 5 70
-
Uterine rupture reported when misoprostol was administered in pregnant women to induce labor or to induce abortion; risk increases with advancing gestational age and with prior uterine surgery, including cesarean delivery.
-
Misoprostol should not be taken by pregnant women to reduce the risk of nonsteroidal anti-inflammatory agent (NSAIA)-induced ulcers.1
-
Misoprostol should not be used for reducing the risk of NSAIA-induced ulcers in women of childbearing potential unless the patient is at high risk of complications from gastric ulcers associated with use of the NSAIA, or is at high risk of developing gastric ulceration.1 In such women, pregnancy must be excluded before the start of treatment and prevented thereafter by use of reliable contraception.1 Misoprostol should only be initiated on the second or third day of the next normal menstrual period.1
-
Advise patients of the abortifacient property of misoprostol and warn them not to give the drug to others because of the danger to women of childbearing potential should the drug be taken by mistake.1
Introduction
Gastric antisecretory agent with protective effects on the gastroduodenal mucosa;1 2 3 13 15 16 25 26 27 31 35 37 47 57 60 72 76 77 78 79 80 84 85 86 87 88 89 91 94 95 127 a synthetic analog of prostaglandin E1 (alprostadil).1 5 10 11 13 20 25 26 27 31 55 76 78 85 95
Prevention of NSAIA-induced Ulcers
Treatment to reduce the risk of NSAIA-induced gastric ulcers in patients at high risk (e.g., concomitant debilitating disease, geriatric patients, history of upper GI ulcer) of developing complications (e.g., bleeding, perforation, death) from these ulcers.1 5 56 61 67 68 70 85 95 96 135 233
Contraindicated for this use in pregnant women.1
Not recommended for use in women of childbearing potential unless the woman is at high risk of developing gastric ulcers or of complications resulting from NSAIA-induced gastric ulcers.1
The American College of Gastroenterology (ACG) has published guidelines for the prevention of NSAIA-related ulcer complications.245 The guidelines state that misoprostol (administered in full doses of 800 mcg daily) is very effective in preventing ulcers and ulcer complications in patients taking NSAIDs, but use may be limited by adverse GI effects.245 There is evidence that lower doses (400–600 mcg daily) may also confer significant protection with a similar adverse effect profile to placebo.245
Termination of Pregnancy
Used in conjunction with misoprostol for termination of intrauterine pregnancy through 70 days of gestation, dated from first day of last menstrual period; duration of pregnancy may be determined by menstrual history or clinical examination, or with an ultrasonographic scan if duration of pregnancy is uncertain or ectopic pregnancy is suspected.241
The American College of Obstetricians and Gynecologists (ACOG) states that the medication abortion regimen supported by major medical organizations nationally and internationally includes mifepristone and misoprostol; if mifepristone is unavailable, then a misoprostol-only regimen is an acceptable alternative.244
Gastric Ulcer
Short-term treatment of active, benign, gastric ulcer† [off-label];2 55 58 72 76 85 87 however, not considered a drug of choice.140
Maintenance treatment following healing of active gastric ulcer to reduce ulcer recurrence† [off-label].72
Duodenal Ulcer
Short-term treatment of endoscopically or radiographically confirmed active duodenal ulcer† [off-label];2 23 55 78 79 80 83 84 85 86 89 91 92 93 94 however, not considered a drug of choice.140
Labor Induction
Treatment to improve cervical inducibility (cervical “ripening”) in appropriately selected pregnant women with unfavorable cervices with a medical or obstetric need for labor induction† [off-label].235 237 238 However, avoid such use in women with prior uterine surgery or cesarean section because of the risk of possible uterine rupture.235 237 238
Postpartum Hemorrhage
Prevention or treatment of serious postpartum hemorrhage† [off-label] in the presence of uterine atony.1 237
Misoprostol Dosage and Administration
Administration
Also has been administered intravaginally†, using tablets formulated for oral administration.1 235 237 238
Oral Administration
Prevention of NSAIA-induced ulcers: Administer in divided doses after meals and at bedtime.1 3 Avoid concomitant administration with a magnesium-containing or other laxative antacid to minimize the incidence of misoprostol-induced diarrhea.1
Termination of pregnancy: Administer misoprostol intrabuccally 24–48 hours following mifepristone administration.241 Place 2 misoprostol tablets in each side of the mouth between the cheek and gums for 30 minutes, then swallow any remnants with water or another liquid.241 Administer in an appropriate setting for the patient, taking into account that expulsion of uterine contents could begin within 2 hours following drug administration.241
Dosage
Adults
Prevention of NSAIA-Induced Ulcers
Oral
200 mcg 4 times daily.1 56 57 59 76 81 95 May reduce dosage to 100 mcg 4 times daily if higher dosage is not well tolerated;1 61 70 however, reduced dosage may be less effective.1 61 67 73 95 Alternatively, 200 mcg twice daily.1 60 Continue therapy for the duration of NSAIA therapy.1
Termination of Pregnancy
Oral
800 mcg intrabuccally (two 200-mcg tablets placed in each cheek pouch) 24–48 hours following mifepristone administration.241 Administration of misoprostol <24 or >48 hours following mifepristone administration may result in reduced efficacy of the combined regimen.241
Vaginal,†Sublingual†, or Buccal†
Alternatively, if mifepristone is unavailable, ACOG states misoprostol may be administered alone at a dose of 800 mcg vaginally, sublingually, or buccally.244 Repeat dose every 3 hours for up to 3 doses for the initial treatment regimen.244 The World Health Organization (WHO) does not specify a maximum number of misoprostol doses for this use.244
Gastric Ulcer†
Oral
100 or 200 mcg 4 times daily for 8 weeks.2 55 58 72 76 87
Duodenal Ulcer†
Oral
100 or 200 mcg 4 times daily or 400 mcg twice daily for 4–8 weeks.2 23 55 78 80 84 89 91 93
Induction of Labor†
Intravaginal†
Initially, 25 mcg (¼ of a 100-mcg oral tablet).235 237 238 Subsequently, 25-mcg every 3–6 hours.235 237 238
Prescribing Limits
Adults
Induction of Labor†
Intravaginal†
Maximum 25 mcg.235 237 238 Subsequently, maximum 25-mcg every 3–6 hours.235 237 238
Special Populations
Renal Impairment
Routine dosage reduction not required;1 5 however, dosage can be reduced if not tolerated.1 5
Geriatric Patients
Routine dosage reduction not required;1 5 however, dosage can be reduced if not tolerated.1 5
Cautions for Misoprostol
Contraindications
-
Pregnant women (when used to reduce the risk of NSAIA-induced gastric ulcers).1
Warnings/Precautions
Warnings
Fetal/Neonatal Morbidity and Mortality
Possible teratogenic and abortifacient effects; possible serious fetal harm when administered to pregnant women.1 5 70 (See Boxed Warning.)
Possible uterine contractions and uterine bleeding and expulsion of the products of conception.1 3 23 55
Uterine rupture reported when administered in pregnant women to induce labor or abortion.1
Possible congenital abnormalities (e.g., skull defects, cranial nerve palsies, facial malformations, and limb defects); sometimes associated with fetal death.1
Contraindicated in pregnant women for reducing the risk of NSAIA-induced gastric ulcers.1 Do not initiate therapy in women of childbearing potential until pregnancy is excluded and other necessary precautions (effective contraception) are ensured.1 5 13 64 70 85 Initiate therapy only after determining that patient is reliable and able to comply with effective contraceptive measures.1 Perform a reliable, blood pregnancy test within 2 weeks prior to beginning therapy.1 Initiate therapy on the second or third day of the next normal menstrual cycle, after a negative pregnancy test is reported.1
If inadvertently administered during pregnancy or if the patient becomes pregnant while receiving the drug, discontinue therapy and inform patient of the potential hazard to the fetus.1
Intravaginal† use may result in uterine hyperstimulation, uterine tetany, uterine rupture, amniotic fluid embolism, pelvic pain, retained placenta, severe genital bleeding, shock, fetal bradycardia, and fetal and maternal death, especially with dosages >25 mcg.1 237 Risk of uterine rupture increases with advancing gestational age, prior uterine surgery (including cesarean delivery), and grand multiparity.1 237 Intravaginal use is not recommended in patients with a previous cesarean delivery or prior major uterine surgery.237
General Precautions
GI Effects
Possible diarrhea; 1 3 5 15 22 23 55 56 57 58 59 61 64 76 78 79 80 81 84 85 86 89 91 92 93 121 151 usually apparent after about 2 weeks of therapy.1 Generally is self-limiting,1 58 61 78 80 85 89 resolving within about a week after onset.1 61 Possible increased risk of profound (e.g., voluminous, watery) and life-threatening diarrhea in patients with inflammatory bowel disease.1 151 Use with extreme caution in these patients; careful monitoring recommended.1 151 Careful monitoring recommended in patients prone to dehydration or in whom its consequences would be dangerous.1 Administer in divided doses after meals and at bedtime;1 3 avoid concomitant administration with a magnesium-containing or other laxative antacid to minimize diarrhea.1
Cardiovascular Effects
Chest pain, edema, diaphoresis, hypotension, hypertension, arrhythmia, phlebitis, increased serum concentrations of cardiac enzymes, syncope, MI (some fatal), and thromboembolic events (e.g., pulmonary embolism, arterial thrombosis, cerebrovascular accident) reported; causal relationship to drug not established.1 Use with caution in patients with preexisting cardiovascular disease.1
Specific Populations
Pregnancy
Risk of serious fetal harm.1 (See Boxed Warning.)
Serious, sometimes fatal, bacterial (e.g., Clostridium sordellii) infection and sepsis or prolonged heavy vaginal bleeding reported following spontaneous, surgical, and medical abortions, including in patients receiving misoprostol with mifepristone for termination of pregnancy; causal relationship to regimen not established.241 242
Lactation
Misoprostol is metabolized rapidly to the free acid following oral administration, which is biologically active and distributed into breast milk.1 No published reports of adverse effects associated with misoprostol in breast-fed infants.1 Caution is advised if used during breast-feeding. 1
Pediatric Use
Safety and efficacy not established in children <18 years of age.1
Geriatric Use
No substantial differences in safety relative to younger adults.1
Renal Impairment
Possible increased half-life,1 3 peak plasma misoprostol acid concentrations, and AUC.1 3
Common Adverse Effects
Diarrhea,1 3 5 15 22 23 55 56 57 58 59 61 64 76 78 79 80 81 84 85 86 89 91 92 93 121 151 abdominal pain.1 5 22 32 55 56 57 61 76 81 91 92 121
Drug Interactions
Drugs Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interaction unlikely.1 3 5 41 126 127
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Aspirin |
||
|
Food and antacids |
Potential decreased rate of absorption of misoprostol, decreased peak plasma concentrations of misoprostol acid1 3 5 95 and decreased oral bioavailability of misoprostol1 5 Magnesium-containing antacids may increase the incidence of misoprostol-induced diarrhea1 |
Avoid concomitant administration of a magnesium-containing or other laxative antacid1 93 |
|
NSAIAs (ibuprofen, piroxicam, diclofenac) |
Misoprostol Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely absorbed from the GI tract;1 2 5 41 42 45 95 88% of a dose is absorbed.45
Onset
Following oral administration, inhibition of gastric acid secretion reaches a maximum within 60–90 minutes.1 5 12 24 36 95
Duration
Following oral administration, inhibition of gastric acid secretion persists for at least 3 hours.1 5 12 24 36 95 Duration is directly related to dose.1 2 12 24 33 46 55 109
Food
Food and antacids decrease the rate of absorption of misoprostol, resulting in delayed and decreased peak plasma concentrations.1 3 95 131
Special Populations
Increased peak plasma misoprostol acid concentrations and AUC in patients with renal impairment.1 3 In geriatric patients, possible increased AUC;1 3 5 43 131 however, peak plasma concentrations are not affected.3 43 131
Distribution
Extent
Distribution into human body tissues and fluids has not been fully characterized.2 5 41 Not known whether misoprostol and/or misoprostol acid cross the placenta.5 Misoprostol acid distributes into milk in humans.1 5
Plasma Protein Binding
Elimination
Metabolism
Rapidly and extensively metabolized to misoprostol acid (the free acid),1 2 5 41 42 43 45 95 at least in part in the GI tract.46 143 Misoprostol acid undergoes extensive, rapid metabolism1 2 3 41 to form inactive metabolites.1 45 127
Elimination Route
Excreted in urine (73%)1 45 100 mainly as metabolites and in feces (15%) via biliary excretion.2 45
Half-life
Biphasic; half-life of free acid is 20–40 minutes.1 5 41 131
Special Populations
In patients with renal impairment, possible increased half-life.1 3
Stability
Storage
Oral
Tablets
Store in a dry place at ≤25°C.1 5
Actions
-
Inhibits gastric acid secretion and protects the gastroduodenal mucosa.1 2 3 15 16 25 26 27 31 35 37 47 57 60 77 85
-
Exhibits substantial dose-related1 2 12 24 33 46 55 109 inhibitory effects on basal, nocturnal, and food- or histamine-stimulated gastric acid secretion1 2 6 12 14 24 32 36 95 via a direct action at the parietal cells.1 2 3 4 5 9 14 20 24 33 64
-
Protective effect may result from increased mucus secretion,1 2 3 5 10 23 25 26 27 33 35 51 95 increased bicarbonate secretion from nonparietal cells,1 2 3 5 10 23 25 26 31 33 35 53 95 enhancement or maintenance of blood flow of the mucosa (possibly via direct vasodilation),2 9 10 17 25 26 33 35 95 protection of submucosal cell proliferation,23 26 stabilization of mucosal membrane systems,23 25 35 prevention of mucosal barrier disruption,2 10 33 35 enhancement of transmucosal diffusion potential,2 117 and inhibition or reduction of back diffusion of hydrogen ions into the mucosa.2 3 33
-
Stimulates intestinal fluid secretion and effects motility.137
-
Increases the amplitude and frequency of uterine contractions and stimulates uterine bleeding and total or partial expulsion of uterine contents in pregnant women.1 3 23 55
Advice to Patients
-
Importance of providing patient a copy of manufacturer’s patient information.1 Patients should read the patient information before initiating misoprostol therapy and every time the prescription is refilled.1
-
Risk of serious fetal harm if administered in pregnant women.1 Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed; necessity for clinicians to advise women to avoid pregnancy during therapy and advise pregnant women of risk to the fetus.1 5 23 95
-
Importance of informing patient that sharing the drug with another individual, particularly a woman of childbearing potential, could be hazardous.1
-
Importance of promptly informing clinicians if they have problems with or questions about misoprostol.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements.1
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
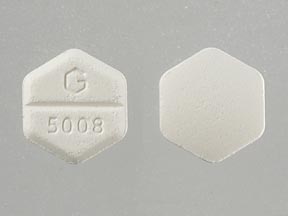
Oral |
Tablets |
100 mcg* |
Cytotec |
Pfizer |
|
Misoprostol Tablets |
||||
|
200 mcg* |
Cytotec |
Pfizer |
||
|
Misoprostol Tablets |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, enteric-coated core, film-coated |
200 mcg Misoprostol outer layer with 50 mg Diclofenac Sodium enteric-coated core |
Arthrotec |
Pfizer |
|
200 mcg Misoprostol outer layer with 75 mg Diclofenac Sodium enteric-coated core |
Arthrotec |
Pfizer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 28, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Pfizer. Cytotec (misoprostol) tablets prescribing information. NY, NY; 2018 Feb.
2. Monk JP, Clissold SP. Misoprostol: a preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in the treatment of peptic ulcer disease. Drugs. 1987; 33:1-30. https://pubmed.ncbi.nlm.nih.gov/3102205
3. Nicholson PA. A review of the therapeutic efficacy of misoprostol, a prostaglandin E1 analogue. S Afr Med J. 1988; 74:56-8. https://pubmed.ncbi.nlm.nih.gov/3133797
4. USP DI Update. No. 3. Misoprostol (systemic). Rockville, MD; The United States Pharmacopeial Convention, Inc; 1989:84-9.
5. Searle. Cytotec (misoprostol) product information form for the American Hospital Formulary Service. Skokie, IL; 1988 Dec.
6. Nakamura T, Niwa H, Muto H. Misoprostol inhibits basal gastric secretion in humans. Gastroenterology. 1986; 90(5 Part 2):1562.
7. Feldman M. Gastric bicarbonate secretion in humans: effect of pentagastrin, bethanechol, and 11,16,16-trimethyl prostaglandin E2. J Clin Invest. 1983; 72:295-303. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1129185/ https://pubmed.ncbi.nlm.nih.gov/6135708
8. Kauffman GL Jr, Reeve JJ Jr, Grossman MI. Gastric bicarbonate secretion: effect of topical and intravenous 16,16-dimethyl prostaglandin E2. Am J Physiol. 1980; 239:G44-8.
9. Colton DG, Driskill DR, Phillips EL et al. Effect of SC-29333, an inhibitor of gastric secretion, on canine gastric mucosal blood flow and serum gastrin levels. Arch Int Pharmacodyn Ther. 1978; 236:86-95. https://pubmed.ncbi.nlm.nih.gov/747466
10. Collins PW. Development and therapeutic role of synthetic prostaglandins in peptic ulcer disease. J Med Chem. 1986; 29:437-3. https://pubmed.ncbi.nlm.nih.gov/3514911
11. Collins PW, Pappo R, Dajani EZ. Chemistry and synthetic development of misoprostol. Dig Dis Sci. 1985; 30:114-7S. https://pubmed.ncbi.nlm.nih.gov/3967559
12. Steiner JA. Misoprostol clinical pharmacology: establishment of activity in man. Dig Dis Sci. 1985; 30:136-41S.
13. Wilson DE. Antisecretory and mucosal protective actions of misoprostol: potential role in the treatment of peptic ulcer disease. Am J Med. 1987; 83(Suppl 1A):2-8. https://pubmed.ncbi.nlm.nih.gov/3113241
14. Davis GR, Fordtran JS, Dajani EZ. Dose-response, meal-stimulated gastric antisecretory study of prostaglandin E1 analog, misoprostol, in man. Dig Dis Sci. 1988; 33:298-302. https://pubmed.ncbi.nlm.nih.gov/3125026
15. Jiranek GC, Kimmey MB, Saunders DR et al. Misoprostol reduces gastroduodenal injury from one week of aspirin: an endoscopic study. Gastroenterology. 1989; 96:656-61. https://pubmed.ncbi.nlm.nih.gov/2491827
16. Cohen MM, Clark L, Armstrong L et al. Reduction of aspirin-induced fecal blood loss with low-dose misoprostol tablets in man. Dig Dis Sci. 1985; 30:605-11. https://pubmed.ncbi.nlm.nih.gov/3924533
17. Sato N, Kawano S, Fukuda M et al. Misoprostol-induced changes in gastric mucosal hemodynamics. Am J Med. 1987; 83(Suppl):15-21. https://pubmed.ncbi.nlm.nih.gov/3113240
18. Clay GA, Goodwin JS. Evaluation of the effects of misoprostol on immunologic competence in normal volunteers. Dig Dis Sci. 1986; 31(Suppl):148-9S.
19. Bright-Asare P, Habte T, Yirgou B et al. Prostaglandins, H2-receptor antagonists and peptic ulcer disease. Drugs. 1988; 35(Suppl 3):1-9 (IDIS 247642)
20. Tsai BS, Kessler LK, Schoenhard G et al. Demonstration of specific E-type prostaglandin receptors using enriched preparations of canine parietal cells and [3H] misoprostol free acid. Am J Med. 1987; 83(Suppl 1A):9-14. https://pubmed.ncbi.nlm.nih.gov/2887113
21. Fich A, Arber N, Sestieri M et al. Effect of misoprostol and cimetidine on gastric cell turnover. Dig Dis Sci. 1985; 30(Suppl):133-5S.
22. Ryan JR, Vargas R, Clay GA et al. Role of misoprostol in reducing aspirin-induced gastrointestinal blood loss in arthritic patients. Am J Med. 1987; 83(Suppl 1A):41-4. https://pubmed.ncbi.nlm.nih.gov/3113245
23. Lewis JH. Summary of the 29th meeting of the gastrointestinal drugs advisory committee, Food and Drug Administration—June 10, 1985. Am J Gastroenterol. 1985; 80:743-5. https://pubmed.ncbi.nlm.nih.gov/3929594
24. Dajani EZ. Perspective on the gastric antisecretory effects of misoprostol in man. Prostaglandins. 1987; 33(Suppl):68-77. https://pubmed.ncbi.nlm.nih.gov/3122277
25. Dajani EZ. Overview of the mucosal protective effects of misoprostol in man. Prostaglandins. 1987; 33(Suppl):117-29. https://pubmed.ncbi.nlm.nih.gov/3122272
26. Wilson DE. Misoprostol and gastroduodenal mucosal protection (cytoprotection). Postgrad Med J. 1988; 64(Suppl 1):7-11. https://pubmed.ncbi.nlm.nih.gov/3138683
27. Hunt JN, Smith JL, Jiang CL et al. Effect of synthetic prostaglandin E1 analog on aspirin-induced gastric bleeding and secretion. Dig Dis Sci. 1983; 28:897-902. https://pubmed.ncbi.nlm.nih.gov/6604619
28. McGuigan JE, Chang Y, Dajani EZ. Effect of misoprostol, an antiulcer prostaglandin, on serum gastrin in patients with duodenal ulcer. Dig Dis Sci. 1986; 31(Suppl):120-5S.
29. Wagner BM. Gastric morphology in ulcer patients receiving misoprostol. Dig Dis Sci. 1985; 30(Suppl):129-32S. https://pubmed.ncbi.nlm.nih.gov/3838153
30. Brecht T. Effects of misoprostol on human circulation. Prostaglandins. 1987; 33(Suppl):51-60. https://pubmed.ncbi.nlm.nih.gov/3122275
31. Isenberg JI, Hogan DL, Selling JA et al. Duodenal bicarbonate secretion in humans: role of prostaglandins. Dig Dis Sci. 1986; 31(Suppl):130S. https://pubmed.ncbi.nlm.nih.gov/3080284
32. Akdamar K, Agrawal N, Ertan A. Inhibition of nocturnal gastric secretion in normal human volunteers by misoprostol: a synthetic prostaglandin E1 methyl ester analog. Am J Gastroenterol. 1982; 77:902-4. https://pubmed.ncbi.nlm.nih.gov/6816064
33. Bauer RF. Misoprostol preclinical pharmacology. Dig Dis Sci. 1985; 30(Suppl):118-25S.
34. Agrawal NM, Godiwala T, Arimura A et al. Cytoprotection by a synthetic prostaglandin against ethanol-induced gastric mucosal damage. Gastrointest Endosc. 1986; 32:67-70. https://pubmed.ncbi.nlm.nih.gov/3086177
35. Miller TA. Protective effects of prostaglandins against gastric mucosal damage: current knowledge and proposed mechanisms. Am J Physiol. 1983; 245:G601-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2879877/ https://pubmed.ncbi.nlm.nih.gov/6195926
36. Ramage JK, Denton A, Williams JG. Inhibition of food stimulated acid secretion by misoprostol, an orally active synthetic E1 analogue prostaglandin. Br J Clin Pharmacol. 1985; 19:9-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1463799/ https://pubmed.ncbi.nlm.nih.gov/3919751
37. Gullikson G, Anglin C, Kessler L et al. Misoprostol prevents aspirin-induced damage in canine Heidenhain pouches. Gastroenterology. 1983; 84(5 Part 2):1176.
38. Moore JG, Alazraki N, Clay GD. Effect of synthetic prostaglandin E1 analog on gastric emptying of meals in man. Dig Dis Sci. 1986; 31: 16-20. https://pubmed.ncbi.nlm.nih.gov/3079695
39. Konturek SJ, Pawlik W. Physiology and pharmacology of prostaglandins. Dig Dis Sci. 1986; 31(Suppl):6-19S.
40. Salmon PR, Barton T. Comparative inhibition of coffee-induced gastric acid secretion employing misoprostol and cimetidine. Dig Dis Sci. 1986; 31(Suppl):55-62S.
41. Schoenhard G, Oppermann J, Kohn FE. Metabolism and pharmacokinetic studies of misoprostol. Dig Dis Sci. 1985; 30(Suppl):126-8S.
42. Leese PT, Karim A, Rozek L. Technical and pharmacological considerations in evaluating misoprostol pharmacokinetic data. Dig Dis Sci. 1986; 31(Suppl):147S. https://pubmed.ncbi.nlm.nih.gov/3731990
43. Karim A, Burns TS, Miller MS et al. Pharmacokinetics and safety of the anti-ulcer prostaglandin mosiprostol in elderly male subjects. Clin Pharmacol Ther. 1987; 41:205.
44. Karim A, Rozek LF, Leese PT. Absorption of misoprostol (Cytotec), an antiulcer prostaglandin, or aspirin is not affected when given concomitantly to healthy human subjects. Gastroenterology. 1987; 92(5 Part 2):1742.
45. Karim A. Antiulcer prostaglandin misoprostol: single and multiple dose pharmacokinetic profile. Prostaglandins. 1989; 33(Suppl):40-50.
46. Tsai BS, Kessler L, Egofske P et al. Antisecretory activity and metabolism of misoprostol in isolated canine parietal cells. Dig Dis Sci. 1986; 31(Suppl):145-50S. https://pubmed.ncbi.nlm.nih.gov/3080277
47. Bauer RF, Bianchi RG, Casler J et al. Comparative mucosal protective properties of misoprostol, cimetidine, and sucralfate. Dig Dis Sci. 1986; 31(Suppl):81-5S.
48. Leung FW, Miller JC, Guth PH. Dissociated effects of misoprostol on gastric acid secretion and mucosal blood flow. Dig Dis Sci. 1986; 31(Suppl): 86-90S.
49. Smedfors B, Johansson C. Stimulation of duodenal bicarbonate secretion by misoprostol. Dig Dis Sci. 1986; 31(Suppl):96-100S.
50. Liss RH, Letourneau RJ, Schepis JP. Evaluation of cytoprotection against ethanol-induced injury in gastric mucosa pretreated with misoprostol, cimetidine, or placebo. Dig Dis Sci. 1986; 31(Suppl):108-14S.
51. Wilson DE, Quadros E, Rajapaksa T et al. Effects of misoprostol on gastric acid and mucus secretion in man. Dig Dis Sci. 1986; 31(Suppl): 126-9S. https://pubmed.ncbi.nlm.nih.gov/3080283
52. Rainsford KD. The effects of aspirin and other non-steroid anti-inflammatoryanalgesic drugs on gastro-intestinal mucus glycoprotein biosynthesis in vivo: relationship to ulcerogenic actions. Biochem Pharmacol. 1978; 27:877-85. https://pubmed.ncbi.nlm.nih.gov/306823
53. Isenberg JI, Hogan DL, Koss MA et al. Human duodenal mucosal bicarbonate secretion: evidence for basal secretion and stimulation by hydrochloric acid and a synthetic prostaglandin E1 analogue. Gastroenterology. 1986; 91:370-8. https://pubmed.ncbi.nlm.nih.gov/3087810
54. Shimizu N, Nakamura T. Prostaglandins as hormones. Dig Dis Sci. 1985; 30(Suppl):109-13S.
55. Herting RL, Nissen CH. Overview of misoprostol clinical experience. Dig Dis Sci. 1986; 31(Suppl): 47-54S. https://pubmed.ncbi.nlm.nih.gov/3080288
56. Roth S, Agrawal N, Mahowald M et al. Misoprostol heals gastroduodenal injury in patients with rheumatoid arthritis receiving aspirin. Arch Intern Med. 1989; 149:775-9. https://pubmed.ncbi.nlm.nih.gov/2495779
57. Lanza FL. A double-blind study of prophylactic effect of misoprostol on lesions of gastric and duodenal mucosa induced by oral administration of tolmetin in healthy subjects. Dig Dis Sci. 1986; 31:131-6S. https://pubmed.ncbi.nlm.nih.gov/3943440
58. Agrawal NM, Saffouri B, Kruss DM et al. Healing of benign gastric ulcer: a placebo-controlled comparison of two dosage regimens of misoprostol, a synthetic analog of prostaglandin E1. Dig Dis Sci. 1985; 30:164-70S.
59. Lanza F, Peace K, Gustitus L et al. A blinded endoscopic comparative study of misoprostol versus sucralfate and placebo in the prevention of aspirin-induced gastric and duodenal ulceration. Am J Gastroenterol. 1988; 83:143-6. https://pubmed.ncbi.nlm.nih.gov/3124604
60. Aadland E, Fausa O, Vatin M et al. Protection by misoprostol against naproxen-induced gastric mucosal damage. Am J Med. 1987; 83(Suppl 1A):37-40.
61. Graham DY, Agrawal NM, Roth SH. Prevention of NSAID-induced gastric ulcer with misoprostol: multicenter, double-blind, placebo-controlled trial. Lancet. 1988; 2:1277-80. https://pubmed.ncbi.nlm.nih.gov/2904006
62. Taha AS, McLaughlin S, Holland PJ et al. Prevention of NSAID-induced gastric ulcer with prostaglandin analogues. Lancet. 1989; 1:52. https://pubmed.ncbi.nlm.nih.gov/2563038
63. Dammann HG, Simon-Schultz J, Bauermeister W et al. Prevention of NSAID-induced gastric ulcer with prostaglandin analogues. Lancet. 1989; 1:52-3. https://pubmed.ncbi.nlm.nih.gov/2563038
64. Shield MJ, Fenn CG. Misoprostol and ulcer prophylaxis. Lancet. 1989; 1:98-9. https://pubmed.ncbi.nlm.nih.gov/2562901
65. Upadhyay R, Taha AS, Sturrock RD et al. Misoprostol and ulcer prophylaxis. Lancet. 1989; 1:212-3. https://pubmed.ncbi.nlm.nih.gov/2563111
66. Nightingale S. Warning changes on NSAIA labeling. JAMA. 1989; 261:1396.
67. Graham DY. Prevention of gastroduodenal injury induced by chronic nonsteroidal antiinflammatory drug therapy. Gastroenterology. 1989; 96:675-81. https://pubmed.ncbi.nlm.nih.gov/2642452
68. Knodel LC. Preventing NSAID-induced gastric ulcers: the role of misoprostol. Hosp Formul. 1989; 24(Suppl A):27-30.
69. Anon. Misoprostol: therapy for the prevention of NSAID-induced gastric ulceration. Hosp Formul. 1989; 24(Suppl A):2-6.
70. Nightingale SL. Approval of misoprostol. JAMA. 1989; 261:1396.
71. Lanza FL, Fakouhi D, Rubin A et al. A double-blind placebo-controlled comparison of the efficacy and safety of 50, 100, and 200 mcg of misoprostol QID in the prevention of ibuprofen-induced gastric and duodenal mucosal lesions and symptoms. Am J Gastroenterol. 1989; 84:633-6. https://pubmed.ncbi.nlm.nih.gov/2499187
72. Ramsey EJ, Harris AE Jr. Prostaglandin E1 analogue therapy in the treatment of refractory gastric ulcer in an elderly patient. Arch Intern Med. 1988; 148:2275-6. https://pubmed.ncbi.nlm.nih.gov/3140754
73. Silverstein FE, Kimmey MB, Saunders DR et al. Gastric protection by misoprostol against 1,300 mg of aspirin: an endoscopic dose-response study. Am J Med. 1987; 83(Suppl 1A):32-6. https://pubmed.ncbi.nlm.nih.gov/3113243
74. Silverstein FE, Kimmey MB, Saunders DR et al. Gastric protection by misoprostol against 1300 mg of aspirin: an endoscopic study. Dig Dis Sci. 1986; 31:137-41S.
75. Mavligit GM, Faintuch J, Levin B et al. Gastroduodenal injury during hepatic arterial infusion of chemotherapeutic agents: lack of cytoprotection by prostaglandin E1 analogue. Gastroenterology. 1987; 566-9.
76. Shield MJ. Interim results of a multicenter international comparison of misoprostol and cimetidine in the treatment of out-patients with benign gastric ulcers. Dig Dis Sci. 1985; 30(Suppl):178-84S. https://pubmed.ncbi.nlm.nih.gov/2857120
77. Dajani EZ, Nissen CH. Gastrointestinal cytoprotective effects of misoprostol: clinical efficacy overview. Dig Dis Sci. 1985; 30(Suppl): 194-200S. https://pubmed.ncbi.nlm.nih.gov/3932054
78. Birnie GG, Watkinson G, Shroff NE et al. Double-blind comparison of two dosage regimens of misoprostol in the treatment of duodenal ulceration. Dig Dis Sci. 1988; 33:1269-73. https://pubmed.ncbi.nlm.nih.gov/3139379
79. Brand DL, Roufail WM, Thomson ABR et al. Misoprostol, a synthetic PGE1 analog, in the treatment of duodenal ulcers: a multicenter double-blind study. Dig Dis Sci. 1985; 30(Suppl): 147-58S.
80. Sontag SJ, Mazure PA, Pontes JF et al. Misoprostol in the treatment of duodenal ulcer: a multicenter double-blind placebo-controlled study. Dig Dis Sci. 1985; 30:159-63S.
81. Lanza FL, Aspinall RL, Swabb EA et al. Double-blind, placebo-controlled endoscopic comparison of the mucosal protective effects of misoprostol versus cimetidine on tolmetin-induced mucosal injury to the stomach and duodenum. Gastroenterology. 1988; 95: 289-94. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3008775/ https://pubmed.ncbi.nlm.nih.gov/3134266
82. McGuigan JE, Gugler R. Summary. Dig Dis Sci. 1986; 31(Suppl):143-4S.
83. Hawkey CJ, Walt RP. Misoprostol, smoking, and duodenal ulcer healing rates. Lancet. 1987; 1:393. https://pubmed.ncbi.nlm.nih.gov/2880206
84. Mazure PA. Comparative efficacy of misoprostol and cimetidine in the treatment of acute duodenal ulcer: results of major studies. Am J Med. 1987; 83(Suppl):22-6. https://pubmed.ncbi.nlm.nih.gov/3113242
85. Watkinson G, Hopkins A, Akbar FA. The therapeutic efficacy of misoprostol in peptic ulcer disease. Postgrad Med J. 1988; 64(Suppl):60-73. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2428767/ https://pubmed.ncbi.nlm.nih.gov/3138682
86. Lam SK, Lau WY, Choi TK et al. Prostaglandin E1 (misoprostol) overcomes the adverse effect of chronic cigarette smoking on duodenal ulcer healing. Dig Dis Sci. 1986; 31(Suppl):68-74S.
87. Rachmilewitz D, Chapman JW, Nicholson PA et al. A multicenter international controlled comparison of two dosage regimens of misoprostol with cimetidine in treatment of gastric ulcer in outpatients. Dig Dis Sci. 1986; 31(Suppl):75-80S.
88. Rachmilewitz D. Role of endogenous prostanoids in pathogenesis of peptic ulcer. Postgrad Med. 1985; 78(Suppl):79-83. https://pubmed.ncbi.nlm.nih.gov/4048044
89. Bright-Asare P, Sontag SJ, Gould RJ et al. Efficacy of misoprostol (twice daily dosage) in acute healing of duodenal ulcer: a multicenter double-blind controlled trial. Dig Dis Sci. 1986; 31(Suppl):63-7S.
90. Rees WDW, Gibbons LC, Turnberg LA. Effects of non-steroidal anti-inflammatory drugs and prostaglandins on alkali secretion by rabbit gastric fundus in vitro. Gut. 1983; 24:784-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1420083/ https://pubmed.ncbi.nlm.nih.gov/6576966
91. Nicholson PA. A multicenter international controlled comparison of two dosage regimes of misoprostol and cimetidine in the treatment of duodenal ulcer in out-patients. Dig Dis Sci. 1985; 30(Suppl):171-7S.
92. Newman RD, Gitlin N, Lacayo EJ et al. Misoprostol in the treatment of duodenal ulcer refractory to H2 blocker therapy: a placebo-controlled, multicenter, double-blind, randomized trial. Am J Med. 1987; 83(Suppl 1A):27-31. https://pubmed.ncbi.nlm.nih.gov/2887112
93. Simjee AE, Spitaels JM, Pettengell KE et al. A comparative study of misoprostol and ranitidine in the healing of duodenal ulcers. S Afr Med J. 1987; 72: 15-7. https://pubmed.ncbi.nlm.nih.gov/3110981
94. O’Keefe SJD, Spitaels JM, Mannion G et al. Misoprostol, a synthetic prostaglandin E1 analogue, in the treatment of duodenal ulcers: a double-blind, cimetidine-controlled trial. S Afr Med J. 1985; 67:321-4. https://pubmed.ncbi.nlm.nih.gov/3920770
95. Stern WR. Summary of the 33rd meeting of the Food and Drug Administration’s Gastrointestinal Drugs Advisory Committee, September 15–16, 1988. Am J Gastroenterol. 1989; 84:351-3. https://pubmed.ncbi.nlm.nih.gov/2494882
96. Miller SR, Fries JF, Spitz P et al. Patients at high risk for developing upper gastrointestinal complications associated with non-steroidal antiinflammatory drugs. Am J Gastroenterol. 1988; 83:1055.
97. Schoenhard GL, Schmidt RE. Initial pharmacokinetic profile of [3H]-SC-29333, a synthetic prostaglandin E1 methyl ester analog, in the rhesus monkey and beagle dog. Fed Proc Am Soc Exp Biol Med. 1978; 37:911.
98. Palmer JF. Letter sent to Bathish J, of Wyeth Laboratories regarding labeling revisions about gastrointestinal adverse reactions to Orudis (ketoprofen). Rockville, MD: Food and Drug Administration, Division of Oncology and Radiopharmaceutical Drug Products; 1988 Sep.
99. Food and Drug Administration. Labeling revisions for NSAIDs. FDA Drug Bull. 1989; 19:3-4.
100. Schoenhard GL, Schmidt RE. Bioavailability and metabolic fate of SC-29333, a synthetic prostaglandin E1 methyl ester analog, in the beagle dog. Fed Proc Am Soc Exp Biol Med. 1979; 38:265.
101. Lacy ER. Effects of absolute ethanol, misoprostol, cimetidine, and phosphate buffer on the morphology of rat gastric mucosae. Dig Dis Sci. 1986; 31(Suppl):101-7S.
102. Hamor GH. Nonsteroidal anti-inflammatory drugs. In: Foye WO, ed. Principles of medicinal chemistry. 3rd ed. Philadelphia: Lea & Febiger; 1989:503-31.
103. Roth SH. Nonsteroidal anti-inflammatory drugs: gastropathy, deaths, and medical practice. Ann Intern Med. 1988; 109:353-4. https://pubmed.ncbi.nlm.nih.gov/3044208
104. Griffin MR, Ray WA, Schaffner W. Nonsteroidal anti-inflammatory drug use and death from peptic ulcer in elderly persons. Ann Intern Med. 1988; 109:359-63. https://pubmed.ncbi.nlm.nih.gov/3261560
105. Peoples JB. Peptic ulcer disease and the nonsteroidal anti-inflammatory drugs. Am Surg. 1985; 51:358-62. https://pubmed.ncbi.nlm.nih.gov/3994179
106. Fromm D. How do non-steroidal anti-inflammatory drugs affect gastric mucosal defenses? Clin Invest Med. 1987; 10:251-8.
107. O’Laughlin JC, Hoftiezer JW, Ivey KJ. Effect of aspirin on the human stomach in normals: endoscopic comparison of damage produced one hour, 24 hours, and 2 weeks after administration. Scand J Gastroenterol. 1981; 16(Suppl 67):211-4.
108. Clinch D, Banerjee AK, Ostick G et al. Non-steroidal anti-inflammatory drugs and gastrointestinal adverse effects. J R Coll Phys London. 1983; 17:228-30.
109. Bianchi RG, Casler JJ, Dajani EZ. Gastric antisecretory and antiulcer activity of SC-29333: a synthetic E-prostaglandin analog. Pharmacologist. 1981; 23:121.
110. Levy M. Aspirin use in patients with major upper gastrointestinal bleeding and peptic-ulcer disease. N Engl J Med. 1974; 290:1158-62. https://pubmed.ncbi.nlm.nih.gov/4545100
111. Robert A, Nezamis JE, Lancaster C et al. Cytoprotection by prostaglandins in rats: prevention of gastric necrosis produced by alcohol, HCl, NaOH, hypertonic NaCl, and thermal injury. Gastroenterology. 1979; 77:433-43. https://pubmed.ncbi.nlm.nih.gov/456839
112. Sharon P, Cohen F, Zifroni A et al. Prostanoid synthesis by cultured gastric and duodenal mucosa: possible role in the pathogenesis of duodenal ulcer. Scand J Gastroenterol. 1983; 18:1045-9. https://pubmed.ncbi.nlm.nih.gov/6584967
113. Simon B, Kather H. Human gastric mucosal adenylate cyclase activity: effects of various cytoprotective prostaglandins. Eur J Clin Invest. 1980; 10:481-5. https://pubmed.ncbi.nlm.nih.gov/6788566
114. Hawkey CJ, Rampton DS. Prostaglandins and the gastrointestinal mucosa: are they important in its function, disease, or treatment? Gastroenterology. 1985; 89:1162-88.
115. Fimmel CJ, Müller-Lissner SA, Blum AL. Bile salt-induced, acute gastric mucosal damage in man: time course and effect of misoprostol, a PGI1-analogue. Scand J Gastroenterol. 1984; 19(Suppl 92):184-8. https://pubmed.ncbi.nlm.nih.gov/6609420
116. Arvidsson S, Falt K, Haglund U. Gastric mucosal damage in sepsis—effects of pretreatment with a synthetic prostaglandin E1 analogue. Gut. 1985; 26:1025-31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1432948/ https://pubmed.ncbi.nlm.nih.gov/3932138
117. Colton DG, Callison DA, Dajani EZ. Effects of a prostaglandin E1 derivative, SC-29333, and aspirin on gastric ionic fluxes and potential difference in dogs. J Pharmacol Exp Ther. 1979; 210:283-8. https://pubmed.ncbi.nlm.nih.gov/458634
118. Larsen KR, Jensen NF, Davis EK et al. The cytoprotective effects of (±)-15-deoxy-16-α, β-hydroxy-16-methyl PGE1 methyl ester (SC-29333) versus aspirin-shock gastric ulcerogenesis in the dog. Prostaglandins. 1981; 21(Suppl):119-24. https://pubmed.ncbi.nlm.nih.gov/6795683
119. Dajani EZ, Driskill DR, Bianchi RG et al. Influence of the position of the side chain hydroxy group on the gastric antisecretory and antiulcer actions of E1 prostaglandin analogs. Prostaglandins. 1975; 10:733-45. https://pubmed.ncbi.nlm.nih.gov/1215536
120. Bianchi RG, Bauer RF. Intestinal antiulcer effect of misoprostol. Pharmacologist. 1982; 24:248.
121. Herting RL, Clay GA. Overview of clinical safety with misoprostol. Dig Dis Sci. 1985; 30(Suppl):185-93S.
122. Fakouhi T, Leese P, Nissen C et al. Tolerability of once-daily doses of 800-mcg and 400-mcg misoprostol in healthy volunteers. Curr Ther Res. 1987; 42:357-63.
123. Wildeman RA. Focus on misoprostol: review of worldwide safety data. Clin Invest Med. 1987; 10: 243-5. https://pubmed.ncbi.nlm.nih.gov/3113801
124. Kotsonis FN, Dodd DC, Regnier B et al. Preclinical toxicology profile of misoprostol. Dig Dis Sci. 1985; 30(Suppl):142-6S.
125. Rees WD, Gibbons LC, Warhurst G et al. Studies of bicarbonate secretion by the normal human stomach in vivo: effect of aspirin, sodium taurocholate, and prostaglandin E2. In: Allen A et al, eds. Mechanisms of mucosal protection in the upper gastrointestinal tract. New York: Raven Press; 1984:119-24.
126. Bennett PN, Fenn GC, Notarianni LJ. Potential drug interactions with misoprostol: effects on the pharmacokinetics of antipyrine and propranolol. Postgrad Med J. 1988; 64(Suppl 1):21-4. https://pubmed.ncbi.nlm.nih.gov/3138681
127. Garris RE, Kirkwood CF. Misoprostol: a prostaglandin E1 analogue. Clin Pharm. 1989; 8:627-44. https://pubmed.ncbi.nlm.nih.gov/2507215
128. Corboy ED Jr, Clay GA, Fakouhi DT et al. Appendix: humanitarian use of misoprostol in severe refractory upper gastrointestinal disease. Am J Med. 1987; 83(Suppl 1A):49-52. https://pubmed.ncbi.nlm.nih.gov/3113246
129. Rietbrock N, Karim A, Nicholson PA. Prevention of NSAID-induced gastric ulcer with prostaglandin analogues. Lancet. 1989; 1:844-5. https://pubmed.ncbi.nlm.nih.gov/2564928
130. Dammann HG, Simon-Schultz J, Kangah R et al. Prevention of NSAID-induced gastric ulcer with prostaglandin analogues. Lancet. 1989; 1:845. https://pubmed.ncbi.nlm.nih.gov/2564929
131. Karim A, Rozek LF, Burns TS. Pharmacokinetic profile of antiulcer prostaglandin misoprostol in humans. Postgrad Med J. 1988; 64(Suppl 1):80.
132. Okabe S, Takeuchi K, Ueki S et al. [Effects of misoprostol, (±)-methyl(11α,13E)-11,16- dihydroxy-16-methyl-9-oxoprost-13-en-l-oate, on various gastric and duodenal lesions in rats.] (Japanese; with English abstract.) Folia Pharmacol Jpn. 1986; 87: 339-350.
133. Cleghorn GJ, Shepherd RW, Holt TL. The use of a synthetic prostaglandin E1 analogue (misoprostol) as an adjunct to pancreatic enzyme replacement in cystic fibrosis. Scand J Gastroenterol. 1988; 23(Suppl 143):142-7.
134. Paller MS. The prostaglandin E1 analog misoprostol reverses acute cyclosporine nephrotoxicity. Transplant Proc. 1988; 20(Suppl 3):634-7. https://pubmed.ncbi.nlm.nih.gov/3133856
135. Hillman AL, Bloom BS. Economic effects of prophylactic use of misoprostol to prevent gastric ulcer in patients taking nonsteroidal anti-inflammatory drugs. Arch Intern Med. 1989; 149:2061-5. https://pubmed.ncbi.nlm.nih.gov/2505706
136. Flower RJ, Moncada S, Vane JR. Analgesic-antipyretics and anti-inflammatory agents: drugs employed in the treatment of gout. In: Gilman AG, Goodman LS, Rall TW et al, eds. Goodman and Gilman’s the pharmacological basis of therapeutics. 7th ed. New York: Macmillan Publishing Company; 1985:674-715.
137. Gullikson GW, Pautsch W, Bianchi RG et al. Comparative effects of misoprostol and 16,16-dimethyl PGE2 on intestinal fluid transport and myoelectric spike activity in the dog. Dig Dis Sci. 1986; 31(Suppl):148S.
138. Paller MS. Effects of the prostaglandin E1 analog misoprostol on cyclosporine nephrotoxicity. Transplantation. 1988; 45:1126-31. https://pubmed.ncbi.nlm.nih.gov/3132763
139. Robinson PG, Sly PD, Smith AL. Arch Dis Child. 1988; 63:1081-2.
140. Walt RP. Misoprostol for the treatment of peptic ulcer and antiinflammatory-drug-induced gastroduodenal ulceration. N Engl J Med. 1992; 327:1575-80. https://pubmed.ncbi.nlm.nih.gov/1435885
141. Antillon M, Cominelli F, Lo S et al. Effect of oral prostaglandin in indomethacin induced renal dysfunction in alcoholic cirrhosis: a double-blind randomized study. Gastroenterology. 1988; 94(5 Part 2):A522. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3095835/
142. Wagner BM. Gastric morphology in ulcer patients receiving misoprostol. Dig Dis Sci. 1985; 30(Suppl):129-32S. https://pubmed.ncbi.nlm.nih.gov/3838153
143. Struthers BJ (Searle, Skokie, IL): Personal Communication; 1989 Oct.
144. Reviewers’ comments (personal observations); 1989 Oct.
145. Clive DM, Stoff JS. Renal syndromes associated with nonsteroidal antiinflammatory drugs. N Engl J Med. 1984; 310:563-72. https://pubmed.ncbi.nlm.nih.gov/6363936
146. Savarino V, Scalabrini P, Mela GS et al. Evaluation of antisecretory activity of misoprostol in duodenal ulcer patients using long-term intragastric pH monitoring. Dig Dis Sci. 1988; 33:293-7. https://pubmed.ncbi.nlm.nih.gov/3125025
147. Dajani EZ, Driskill DR, Bianchi RG et al. Effect of a prostaglandin analogue, SC-30249, on canine gastric secretion. Drug Dev Res. 1983; 3:339-47.
148. Ottignon Y, Ethevenaux C, Capron MH et al. The effect of a prostaglandin1 (PGE1) on the lower esophageal sphincter (LES) in man. Gastroenterology. 1988; 94(5 Part 2):A338. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3095835/
149. Mozes M, Moran M, Kotel B et al. Misoprostol (M) improves renal function and reduces the frequency of acute rejection (AR) in cyclosporine-treated (CsA) renal transplant recipients. Proc Am Soc Nephrol. 1988:372A.
150. Blackburn WD Jr, Alarcon GS. Misoprostol treatment of gastropathy due to nonsteroidal anti-inflammatory drugs. Am J Med. 1990; 88:85. https://pubmed.ncbi.nlm.nih.gov/2104742
151. Kornbluth A, Gupta R, Gerson CD. Life-threatening diarrhea after short-term misoprostol use in a patient with Crohn ileocolitis. Ann Intern Med. 1990; 113:474-6. https://pubmed.ncbi.nlm.nih.gov/2117413
152. Peterson WL. Helicobacter pylori and peptic ulcer disease. N Engl J Med. 1991; 324:1043-8. https://pubmed.ncbi.nlm.nih.gov/2005942
153. Marshall BJ. Campylobacter pylori: Its link to gastritis and peptic ulcer disease. Clin Infect Dis. 1990; 12(Suppl 1):S87-93.
154. Reviewers’ comments (personal observations); 1993 Oct 26.
155. Blaser MJ. Helicobacter pylori: its role in disease. Clin Infect Dis. 1992; 15:386-91. https://pubmed.ncbi.nlm.nih.gov/1520782
156. Murray DM, DuPont HL, Cooperstock M et al. Evaluation of new antiinfective drugs for the treatment of gastritis and peptic ulcer disease associated with infection by Helicobacter pylori. Clin Infect Dis. 1992; 15(Suppl 1):S268-73.
157. Graham DY, Go MF. Evaluation of new antiinfective drugs for Helicobacter pylori infection: revisited and updated. Clin Infect Dis. 1993; 17:293-4. https://pubmed.ncbi.nlm.nih.gov/8399892
158. Murray DM, DuPont HL. Reply. (Evaluation of new antiinfective drugs for Helicobacter pylori infection: revisited and updated.) Clin Infect Dis. 1993; 17:294-5.
159. George LL, Borody TJ, Andrews P et al. Cure of duodenal ulcer after eradication of H. pylori. Med J Aust. 1990; 153:145-9. https://pubmed.ncbi.nlm.nih.gov/1974027
160. Farrell MK. Dr. Apley meets Helicobacter pylori. J Pediatr Gastroenterol Nutr. 1993; 16:118-9. https://pubmed.ncbi.nlm.nih.gov/8450375
161. Fiocca R, Solcia E, Santoro B. Duodenal ulcer relapse after eradication of Helicobacter pylori. Lancet. 1991; 337:1614. https://pubmed.ncbi.nlm.nih.gov/1675746
162. Graham DY, Lew GM, Evans DG et al. Effect of triple therapy (antibiotics plus bismuth) on duodenal ulcer healing. A randomized controlled trial. Ann Intern Med. 1991; 115:266-9. https://pubmed.ncbi.nlm.nih.gov/1854110
163. Marshall BJ. Treatment strategies for Helicobacter pylori infection. Gastroenterol Clin North Am. 1993; 22:183-98. https://pubmed.ncbi.nlm.nih.gov/8449566
164. Chiba N, Rao BV, Rademaker JW et al. Meta-analysis of the efficacy of antibiotic therapy in eradicating Helicobacter pylori. Am J Gastroenterol. 1992; 87:1716-27. https://pubmed.ncbi.nlm.nih.gov/1449132
165. Glassman MS. Helicobacter pylori infection in children. A clinical overview. Clin Pediatr (Phila). 1992; 31:487-7.
166. Bianchi Porro G, Parente F, Lazzaroni M. Short and long term outcome of Helicobacter pylori positive resistant duodenal ulcers treated with colloidal bismuth subcitrate plus antibiotics or sucralfate alone. Gut. 1993; 34:466-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374304/ https://pubmed.ncbi.nlm.nih.gov/8491391
167. Borody T, Andrews P, Mancuso N et al. Helicobacter pylori reinfection 4 years post-eradication. Lancet. 1992; 339:1295. https://pubmed.ncbi.nlm.nih.gov/1349686
168. Hixson LJ, Kelley Cl, Jones WN et al. Current trends in the pharmacotherapy for peptic ulcer disease. Arch Intern Med. 1992; 152:726-32. https://pubmed.ncbi.nlm.nih.gov/1558429
169. Rauws EAJ, Tytgat GNJ. Cure of duodenal ulcer with eradication of Helicobacter pylori. Lancet. 1990; 335:1233-5. https://pubmed.ncbi.nlm.nih.gov/1971318
170. Hentschel E, Brandstätter G, Dragosics B et al. Effect of ranitidine and amoxicillin plus metronidazole on the eradication of Helicobacter pylori and the recurrence of duodenal ulcer. N Engl J Med. 1993; 328:308-12. https://pubmed.ncbi.nlm.nih.gov/8419816
171. Burette A, Glupczynski Y. On: The who’s and when’s of therapy for Helicobacter pylori. 1991; 86:924-5. Letter.
172. Bell GD, Powell K, Burridge SM et al. Experience with ″triple’ anti-Helicobacter pylori eradication thearpy: side effects and the importance of testing the pre-treatment bacterial isolate for metronidazole resistance. Aliment Pharmacol Ther. 1992; 6:427-35. https://pubmed.ncbi.nlm.nih.gov/1420735
173. Sloane R, Cohen H. Common-sense management of Helicobacter pylori-associated gastroduodenal disease. Personal views. Gastroenterol Clin North Am. 1993; 22:199-206. https://pubmed.ncbi.nlm.nih.gov/8449567
174. Ateshkadi A, Lam NP, Johnson CA. Helicobacter pylori and peptic ulcer disease. Clin Pharm. 1993; 12:34-48. https://pubmed.ncbi.nlm.nih.gov/8428432
175. Bayerdorffer E, Mannes GA, Sommer A et al. Long-term follow-up after eradication of Helicobacter pylori with a combination of omeprazole and amoxycillin. Scand J Gastroenterol Suppl. 1993; 196:19-25. https://pubmed.ncbi.nlm.nih.gov/8341987
176. Unge P, Ekstrom P. Effects of combination therapy with omeprazole and an antibiotic on H. pylori and duodenal ulcer disease. Scand J Gastroenterol Suppl. 1993; 196:17-8.
177. Hunt RH. Hp and pH: implications for the eradication of Helicobacter pylori. Scand J Gastroenterol Suppl. 1993; 196:12-6. https://pubmed.ncbi.nlm.nih.gov/8341986
178. Malfertheiner P. Compliance, adverse events and antibiotic resistance in Helicobacter pylori treatment. Scand J Gastroenterol Suppl. 1993; 196:34-7. https://pubmed.ncbi.nlm.nih.gov/8341989
179. Bell GD, Powell U. Eradication of Helicobacter pylori and its effect in peptic ulcer disease. Scand J Gastroenterol Suppl. 1993; 196:7-11. https://pubmed.ncbi.nlm.nih.gov/8341990
180. Bianchi Porro G, Parente F, Lazzaroni M. Short and long term outcome of Helicobacter pylori positive resistant duodenal ulcers treated with colloidal bismuth subcitrate plus antibiotics or sucralfate alone. Gut. 1993; 34:466-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374304/ https://pubmed.ncbi.nlm.nih.gov/8491391
181. Graham DY, Go MF. Evaluation of new antiinfective drugs for Helicobacter pylori infection: revisited and updated. Clin Infect Dis. 1993; 17:293-4. https://pubmed.ncbi.nlm.nih.gov/8399892
182. Murray DM, DuPont HL. Reply. (Evaluation of new antiinfective drugs for Helicobacter pylori infection: revisited and updated.) Clin Infect Dis. 1993; 17: 294-5.
183. George LL, Borody TJ, Andrews P et al. Cure of duodenal ulcer after eradication of H. pylori. Med J Aust. 1990; 153:145-9. https://pubmed.ncbi.nlm.nih.gov/1974027
184. Farrell MK. Dr. Apley meets Helicobacter pylori. J Pediatr Gastroenterol Nutr. 1993; 16:118-9. https://pubmed.ncbi.nlm.nih.gov/8450375
185. Fiocca R, Solcia E, Santoro B. Duodenal ulcer relapse after eradication of Helicobacter pylori. Lancet. 1991; 337:1614. https://pubmed.ncbi.nlm.nih.gov/1675746
186. Marshall BJ. Campylobacter pylori: its link to gastritis and peptic ulcer disease. Clin Infect Dis. 1990; 12(Suppl 1):S87-93.
187. Borody T, Andrews P, Mancuso N et al. Helicobacter pylori reinfection 4 years post-eradication. Lancet. 1992; 339:1295. https://pubmed.ncbi.nlm.nih.gov/1349686
188. Hixson LJ, Kelley CL, Jones WN et al. Current trends in the pharmacotherapy for peptic ulcer disease. Arch Intern Med. 1992; 152:726-32. https://pubmed.ncbi.nlm.nih.gov/1558429
189. Rauws EAJ, Tytgat GNJ. Cure of duodenal ulcer with eradication of Helicobacter pylori. Lancet. 1990; 335:1233-5. https://pubmed.ncbi.nlm.nih.gov/1971318
190. Hunt RH. pH and Hp—gastric acid secretion and Helicobacter pylori: implications for ulcer healing and eradication of the organism. Am J Gastroenterol. 1993; 88:481-3. https://pubmed.ncbi.nlm.nih.gov/8470623
191. Hentschel E, Brandstatter G, Dragosics B et al. Effect of ranitidine and amoxicillin plus metronidazole on the eradication of Helicobacter pylori and the recurrence of duodenal ulcer. N Engl J Med. 1993; 328:308-12. https://pubmed.ncbi.nlm.nih.gov/8419816
192. Graham DY, Lew GM, Evans DG et al. Effect of triple therapy (antibiotics plus bismuth) on duodenal ulcer healing: a randomized controlled trial. Ann Intern Med. 1991; 115:266-9. https://pubmed.ncbi.nlm.nih.gov/1854110
193. Reviewers’ comments (personal observations) on Helicobacter pylori; 1993 Oct 26.
194. Marshall BJ. Helicobacter pylori. Am J Gastroenterol. 1994; 89(Suppl):S116-28.
195. Labenz J, Gyenes E, Rühl GH et al. Amoxicillin plus omeprazole versus triple therapy for eradication of Helicobacter pylori in duodenal ulcer disease: a prospective, randomized, and controlled study. Gut. 1993; 34:1167-70. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1375447/ https://pubmed.ncbi.nlm.nih.gov/8406147
196. Labenz J, Börsch G. Highly significant change of the clinical course of relapsing and complicated peptic ulcer disease after cure of Helicobacter pylori infection. Am J Gastroenterol. 1994; 89:1785-8. https://pubmed.ncbi.nlm.nih.gov/7942667
197. Wang WM, Chen CY, Jan CM et al. Long-term follow-up and serological study after triple therapy of Helicobacter pylori-associated duodenal ulcer. Am J Gastroenterol. 1994; 89:1793-6. https://pubmed.ncbi.nlm.nih.gov/7942669
198. Anon. Drugs for treatment of peptic ulcers. Med Lett Drugs Ther. 1994; 36:65-7. https://pubmed.ncbi.nlm.nih.gov/7912812
199. Freston JW. Emerging strategies for managing peptic ulcer disease. Scand J Gastroenterol Suppl. 1994; 201:49-54. https://pubmed.ncbi.nlm.nih.gov/8047824
200. Axon ATR. The role of acid inhibition in the treatment of Helicobacter pylori infection. Scand J Gastroenterol Suppl. 1994; 201:16-23. https://pubmed.ncbi.nlm.nih.gov/8047818
201. Labenz J, Rühl GH, Bertrams J et al. Medium- or high-dose omeprazole plus amoxicillin eradicates Helicobacter pylori in gastric ulcer disease. Am J Gastroenterol. 1994; 89:726-30. https://pubmed.ncbi.nlm.nih.gov/8172146
202. Labenz J, Borsch G. Evidence for the essential role of Helicobacter pylori in gastric ulcer disease. Gut. 1994; 35:19-22. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374625/ https://pubmed.ncbi.nlm.nih.gov/8307443
203. NIH Consensus Development Panel on. Helicobacter pylori in Peptic Ulcer Disease. JAMA. 1994; 272:65-9. https://pubmed.ncbi.nlm.nih.gov/8007082
204. Fennerty MB. Helicobacter pylori. Ann Intern Med. 1994: 154:721-7.
205. Adamek RJ, Wegener M, Labenz J et al. Medium-term results of oral and intravenous omeprazole/amoxicillin Helicobacter pylori eradication therapy. Am J Gastroenterol. 1994; 89:39-42. https://pubmed.ncbi.nlm.nih.gov/8273795
206. Bell GD, Powell KU, Burridge SM et al. Helicobacter pylori eradication: efficacy and side effect profile of a combination of omeprazole, amoxycillin and metronidazole compared with four alternative regimens. Q J Med. 1993; 86:743-50. https://pubmed.ncbi.nlm.nih.gov/8265776
207. Nomura A, Stemmermann GN, Chyou PH et al. Helicobacter pylori infection and gastric carcinoma among Japanese Americans in Hawaii. N Engl J Med. 1991; 325:1132-6. https://pubmed.ncbi.nlm.nih.gov/1891021
208. Parsonnet J, Friedman GD, Vandersteen DP et al. Helicobacter pylori infection and the risk of gastric carcinoma. N Engl J Med. 1991; 325:1127-31. https://pubmed.ncbi.nlm.nih.gov/1891020
209. The EUROGAST Study Group. An international association between Helicobacter pylori infection and gastric cancer. Lancet. 1993; 341:1359-62. https://pubmed.ncbi.nlm.nih.gov/8098787
210. Talley NJ, Zinsmeister AR, Weaver A et al. Gastric adenocarcinoma and Helicobacter pylori infection. J Natl Cancer Inst. 1991; 83:1734-9. https://pubmed.ncbi.nlm.nih.gov/1770552
211. Forman D, Newell DG, Fullerton F et al. Association between infection with Helicobacter pylori and risk of gastric cancer: evidence from a prospective investigation. BMJ. 1991; 302:1302-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1670011/ https://pubmed.ncbi.nlm.nih.gov/2059685
212. Forman D. Helicobacter pylori infection: a novel risk factor in the etiology of gastric cancer. J Natl Cancer Inst. 1991; 83:1702-3. https://pubmed.ncbi.nlm.nih.gov/1770545
213. Parsonnet J. Helicobacter pylori and gastric cancer. Gastroenterol Clin North Am. 1993; 22:89-104. https://pubmed.ncbi.nlm.nih.gov/8449573
214. Correa P. Is gastric carcinoma an infectious disease? N Engl J Med. 1991; 325:1170-1.
215. Isaacson PG, Spencer J. Is gastric lymphoma an infectious disease? Hum Pathol. 1993; 24:569-70.
216. Markham A, McTavish D. Clarithromycin and omeprazole: as Helicobacter pylori eradication therapy in patients with H. pylori-associated gastric disorders. Drugs. 1996; 51:161-78. https://pubmed.ncbi.nlm.nih.gov/8741237
217. Soll AH. Medical treatment of peptic ulcer disease. JAMA. 1996; 275:622-9. https://pubmed.ncbi.nlm.nih.gov/8594244
218. Walsh JH, Peterson WL. The treatment of Helicobacter pylori infection in the management of peptic ulcer disease. N Engl J Med. 1995; 333:984-91. https://pubmed.ncbi.nlm.nih.gov/7666920
219. Hackelsberger A, Malfertheiner P. A risk-benefit assessment of drugs used in the eradication of Helicobacter pylori infection. Drug Saf. 1996; 15:30-52. https://pubmed.ncbi.nlm.nih.gov/8862962
220. Rauws EAJ, van der Hulst RWM. Current guidelines for the eradication of Helicobacter pylori in peptic ulcer disease. Drugs. 1995; 6:984-90.
221. van der Hulst RWM, Keller JJ, Rauws EAJ et al. Treatment of Helicobacter pylori infection: a review of the world literature. Helicobacter. 1996; 1:6-19. https://pubmed.ncbi.nlm.nih.gov/9398908
222. Lind T, Veldhuyzen van Zanten S, Unge P et al. Eradication of Helicobacter pylori using one-week triple therapies combining omeprazole with two antimicrobials: the MACH I study. Helicobacter. 1996; 1:138-44. https://pubmed.ncbi.nlm.nih.gov/9398894
223. Anon. The choice of antibacterial drugs. Med Lett Drugs Ther. 1996; 38:25-34. https://pubmed.ncbi.nlm.nih.gov/8598824
224. Fennerty MB. Practice guidelines for treatment of peptic ulcer disease. JAMA. 1996; 276:1135. https://pubmed.ncbi.nlm.nih.gov/8827957
225. Soll AH. Practice guidelines for treatment of peptic ulcer disease. JAMA. 1996; 276:1136-7.
226. Langtry HD, Wilde MI. Lansoprazole: an update of its pharmacological properties and clinical efficacy in the management of acid-related disorders. Drugs. 1997; 54:473-500. https://pubmed.ncbi.nlm.nih.gov/9279507
227. TAP Pharmaceuticals, Inc. Prevacid (lansoprazole) delayed-release capsules prescribing information. Deerfield, IL; 1997 Aug.
228. Garnett RG. Lansoprazole: a proton pump inhibitor. Ann Pharmacother. 1996; 30:1425. https://pubmed.ncbi.nlm.nih.gov/8968456
229. Zimmerman AE, Katona BG. Lansoprazole: a comprehensive review. Pharmacotherapy. 1997; 17:308-26. https://pubmed.ncbi.nlm.nih.gov/9085323
230. Hatlebakk JG, Nesje LB, Hausken T et al. Lansoprazole capsules and amoxicillin oral suspension in the treatment of peptic ulcer disease. Scand J Gastroenterol. 1995; 11:1053-7.
231. Merck. Vioxx (rofecoxib) tablets and oral suspension prescribing information. West Point, PA; 1999 Sep.
232. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999; 340:1888-99. https://pubmed.ncbi.nlm.nih.gov/10369853
233. Lanza FL. A guideline for the treatment and prevention of NSAIA-induced ulcers. Am J Gastroenterol. 1998; 93:2037-46. https://pubmed.ncbi.nlm.nih.gov/9820370
235. Anon. ACOG committee opinion: induction of labor with misoprostol. Obstet Gynecol. 1999; 94:1-2.
236. Cullen M, Searle. Dear health care provider: Important drug warning concerning unapproved use of intravaginal or oral misoprostol in pregnant women for induction of labor or abortion. Skokie, IL; 2000 Aug 23.
237. American College of Obstetricians and Gynecologists. News release: ACOG issues letter on safety of misoprostol. Washington, DC; 2000 Oct 12.
238. American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins. Induction of labor. Practice Bulletin No. 10. Washington, DC: American College of Obstetricians and Gynecologists; 1999 Nov.
239. Anon. Mifepristone (RU486). Med Lett Drugs Ther. 1994; 36:78-80. https://pubmed.ncbi.nlm.nih.gov/7914667
240. Christine-Maitre S, Bouchard P, Spitz IM. Medical termination of pregnancy. N Engl J Med. 2000; 946-56.
241. Danco Laboratories, LLC. Mifeprex (mifepristone) oral tablets prescribing information. New York, NY; 2020 Oct.
242. Food and Drug Administration. Questions and answers on Mifeprex. Silver Spring, MD; 2019 Apr 12. From FDA website. https://www.fda.gov/Drugs/Postmarket-Drug-Safety-information-Patients-and-Providers/questions-and-answers-Mifeprex
243. Anon. Drugs for treatment of peptic ulcers. Med Lett Drugs Ther. 1997; 39:1-4. https://pubmed.ncbi.nlm.nih.gov/8996458
244. American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins. Medical abortion up to 70 days of gestation. Practice Bulletin No. 225. Washington, DC: American College of Obstetricians and Gynecologists; 2014 Mar. https://www.acog.org/-/media/project/acog/acogorg/clinical/files/practice-bulletin/articles/2020/10/medication-abortion-up-to-70-days-gestation.pdf
245. Lanza FL, Chan FK, Quigley EM; Practice Parameters Committee of the American College of Gastroenterology. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009 Mar;104(3):728-38. Epub 2009 Feb 24. https://pubmed.ncbi.nlm.nih.gov/19240698
Related/similar drugs
More about misoprostol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (724)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: miscellaneous GI agents
- Breastfeeding
- En español