Methotrexate Dosage
Medically reviewed by Drugs.com. Last updated on Apr 28, 2025.
Applies to the following strengths: 2.5 mg; 25 mg/mL; 25 mg/mL preservative-free; 1 g; 20 mg; 50 mg; 5 mg; 7.5 mg; 10 mg; 15 mg; 2.5 mg/mL; 10 mg/0.4 mL; 12.5 mg/0.4 mL; 15 mg/0.4 mL; 17.5 mg/0.4 mL; 20 mg/0.4 mL; 22.5 mg/0.4 mL; 25 mg/0.4 mL; 7.5 mg/0.4 mL; 7.5 mg/0.15 mL; 10 mg/0.2 mL; 12.5 mg/0.25 mL; 15 mg/0.3 mL; 17.5 mg/0.35 mL; 22.5 mg/0.45 mL; 25 mg/0.5 mL; 27.5 mg/0.55 mL; 30 mg/0.6 mL; 7.5 mg/0.3 mL; 12.5 mg/0.5 mL; 15 mg/0.6 mL; 17.5 mg/0.7 mL; 20 mg/0.8 mL; 22.5 mg/0.9 mL; 25 mg/mL-NaCl 0.9% preservative-free; 2 mg/mL
Usual Adult Dose for:
- Acute Lymphoblastic Leukemia
- Trophoblastic Disease
- Meningeal Leukemia
- Mycosis Fungoides
- Osteosarcoma
- Psoriasis
- Rheumatoid Arthritis
- non-Hodgkin's Lymphoma
- Breast Cancer
- Head and Neck Cancer
Usual Pediatric Dose for:
- Acute Lymphoblastic Leukemia
- Meningeal Leukemia
- Juvenile Rheumatoid Arthritis
- non-Hodgkin's Lymphoma
- Osteosarcoma
Additional dosage information:
Usual Adult Dose for Acute Lymphoblastic Leukemia
The recommended dose varies from 10 to 5000 mg/m2 IV.
- Lower doses from 20 to 30 mg/m2/week IM can be given.
- Tablet: 20 mg/m2 orally once weekly as a maintenance of chemotherapy combination regimen
Comments:
- When using high-dose injection of this drug regimen, adhere to the guidelines for high-dose methotrexate regimen and use leucovorin rescue as recommended.
- Tailor the dosage and timing of drug administration to the specific disease condition, patient's risk category, concomitant medications, treatment phase, and individual response to therapy.
- Following the initiation of methotrexate tablets, regularly assess the absolute neutrophil count (ANC) and platelet count, and modify the dose as needed to maintain the ANC within the desired range and prevent excessive myelosuppression.
Use: Acute lymphoblastic leukemia (ALL)
Usual Adult Dose for Trophoblastic Disease
Gestational trophoblastic neoplasia:
Usual dose:
- For patients with low-risk gestational trophoblastic neoplasia (GTN): 30 mg/m2 to 200 mg/m2 or 0.4 mg/kg to 1 mg/kg intravenously or intramuscularly
- For patients with high-risk GTN: 300 mg/m2 over 12 hours as an intravenous infusion as a component of a multi-drug regimen
Use: For the treatment of adults with GTN as part of a combination chemotherapy regimen
Usual Adult Dose for Meningeal Leukemia
Usual dose: Age based dosing of methotrexate administered intrathecally
- Less than 1 year: 6 mg
- 1 to less than 2 years: 8 mg
- 2 to less than 3 years: 10 mg
- 3 to less than 9 years: 12 mg
- Greater than or equal to 9 years: 12 to 15 mg
Comments:
- Only preservative-free formulation should be used for intrathecal injection.
- Before administering, it is necessary to dilute preservative-free methotrexate injection to a concentration of 1 mg/mL using preservative-free 0.9% Sodium Chloride Injection, USP.
- To manage meningeal leukemia, intrathecal methotrexate can be administered every 2 days or longer, with a maximum of twice per week. However, giving it at intervals shorter than 1 week may lead to increased subacute toxicity. For the prevention of meningeal leukemia, methotrexate injection is given no more frequently than once per week.
- Leucovorin rescue should be administered along with intrathecal methotrexate injection for patients with Down Syndrome.
Use: For the prophylaxis and treatment of meningeal leukemia in adult patients
Usual Adult Dose for Mycosis Fungoides
Usual dose:
- Single agent: 25 mg to 75 mg orally once weekly
- As a part of combination chemotherapy regimen: 10 mg/m2 orally twice weekly
Use: For the treatment of adults with mycosis fungoides (cutaneous T-cell lymphoma)
Usual Adult Dose for Osteosarcoma
Usual dose: As a part of combination chemotherapy regimen: 12 g/m2 (maximum 20 g/dose) as an intravenous infusion over 4 hours
Comments:
- Administer leucovorin rescue in accordance with high-dose methotrexate regimen guidelines.
- Based on the observed peak serum methotrexate concentrations, adjustments to subsequent doses may be necessary.
- The dosage and schedule may vary depending on factors such as patient comorbidities, disease state, and previous treatments.
Use: For the treatment of adult patients with osteosarcoma as part of a combination chemotherapy regimen
Usual Adult Dose for Psoriasis
Usual dose: 10 mg to 25 mg intramuscularly/intravenously/orally once weekly until adequate response is achieved
Comments:
- To attain the best clinical response, adjust the dose gradually while ensuring it does not exceed 25 mg per week.
- Once the optimal clinical response has been reached, reduce the dosage to the lowest possible dosing regimen.
- To minimize the risk of adverse reactions, it is advisable to administer folic acid or folinic acid.
Use: For the treatment of adults with severe psoriasis
Usual Adult Dose for Rheumatoid Arthritis
Usual dose:
- 7.5 mg once weekly orally/intramuscularly with escalation to achieve optimal response
Comments:
- Dosages exceeding 20 mg once weekly elevate the risk of severe adverse reactions, including myelosuppression.
- Most responses are typically observed within 3 to 6 weeks after initiating treatment, although responses have also been reported up to 12 weeks after starting treatment.
- To minimize the risk of adverse reactions, it is advisable to administer folic acid or folinic acid.
Use: For the treatment of adults with rheumatoid arthritis
Usual Adult Dose for non-Hodgkin's Lymphoma
Usual dose:
INTRAVENOUS:
- As a part of combination regimen: 10 mg/m2 to 8,000 mg/m2 intravenously
- Single agent for central nervous system-directed therapy: 8,000 mg/m2 intravenously
- Single agent for cutaneous forms of non-Hodgkin lymphoma: 5 to 75 mg intravenously
- As a part of combination chemotherapy regimen: 1,000 mg/m2 or 3,000 mg/m2 as an intravenous infusion over 24 hours followed by leucovorin rescue in accordance with high-dose methotrexate regimen guidelines
- As a part of combination with immunochemotherapy regimen: 3,000 mg/m2 to 8,000 mg/m2 followed by leucovorin rescue in accordance with high-dose methotrexate regimen guidelines
- 2.5 mg orally 2 to 4 times per week (maximum 10 mg per week) as part of a metronomic combination chemotherapy regimen
Comments:
- The recommended dose for intrathecal methotrexate injection (preservative-free) depends on the individual's age. Refer to dosing provided in the meningeal leukemia dosing section.
- The frequency of intrathecal administration differs depending on whether it is used for treatment or prophylaxis, as well as other relevant factors.
Use: For the treatment of adult patients with non-Hodgkin lymphoma
Usual Adult Dose for Breast Cancer
Usual dose: 40 mg/m2 intravenously as a part of a cyclophosphamide and fluorouracil based multi-drug regimen.
Use: For the treatment of adults with breast cancer as part of a combination chemotherapy regimen
Usual Adult Dose for Head and Neck Cancer
Usual dose: 40 to 60 mg/m2 intravenously once weekly
Use: For the treatment of adults with squamous cell carcinoma of the head and neck as a single-agent
Usual Pediatric Dose for Acute Lymphoblastic Leukemia
The recommended varies from 10 to 5000 mg/m2 IV.
- Lower doses from 20 to 30 mg/m2/week IM can be given.
- Tablet: 20 mg/m2 orally once weekly as a maintenance of chemotherapy combination regimen
Comments:
- When using high-dose injection of this drug regimen, adhere to the guidelines for high-dose methotrexate regimen and use leucovorin rescue as recommended.
- Tailor the dosage and timing of drug administration to the specific disease condition, patient's risk category, concomitant medications, treatment phase, and individual response to therapy.
- Following the initiation of methotrexate tablets, regularly assess the absolute neutrophil count (ANC) and platelet count, and modify the dosage as needed to maintain the ANC within the desired range and prevent excessive myelosuppression.
Use: Acute lymphoblastic leukemia (ALL)
Usual Pediatric Dose for Meningeal Leukemia
Usual dose:
Age based dosing of methotrexate administered intrathecally:
- less than 1 year: 6 mg
- 1 to less than 2 years: 8 mg
- 2 to less than 3 years: 10 mg
- 3 to less than 9 years: 12 mg
- greater than or equal to 9 years: 12 to 15 mg
Comments:
- Only preservative-free formulations should be used for intrathecal injection.
- Before administering, it is necessary to dilute preservative-free methotrexate injection to a concentration of 1 mg/mL using preservative-free 0.9% Sodium Chloride Injection, USP.
- To manage meningeal leukemia, intrathecal methotrexate can be administered every 2 days or longer, with a maximum of twice per week. However, giving it at intervals shorter than 1 week may lead to heightened subacute toxicity. For the prevention of meningeal leukemia, methotrexate injection is given no more frequently than once per week.
- Leucovorin rescue should be administered along with intrathecal methotrexate injection for patients with Down Syndrome.
Use: For the prophylaxis and treatment of meningeal leukemia in pediatric patients
Usual Pediatric Dose for Juvenile Rheumatoid Arthritis
Usual dose: 10 mg/m2 once weekly administered subcutaneously/intramuscularly/orally, with escalation to achieve optimal response
Comments:
- Dosages exceeding 30 mg/m2 once weekly elevate the risk of severe adverse reactions, including myelosuppression.
- Most responses are typically observed within 3 to 6 weeks after initiating treatment, although responses have also been reported up to 12 weeks after starting treatment.
- To minimize the risk of adverse reactions, it is advisable to administer folic acid or folinic acid.
Use: For the treatment of pediatric patients with polyarticular Juvenile Idiopathic Arthritis (pJIA)
Usual Pediatric Dose for non-Hodgkin's Lymphoma
Usual dose:
INTRAVENOUS:
- As a part of a combination regimen: 10 mg/m2 to 8,000 mg/m2 intravenously
- Single agent for central nervous system-directed therapy: 8,000 mg/m2 intravenously
- Single agent for cutaneous forms of non-Hodgkin's lymphoma: 5 to 75 mg intravenously
- As a part of combination chemotherapy regimen: 1,000 mg/m2 or 3,000 mg/m2 as an intravenous infusion over 24 hours followed by leucovorin rescue in accordance with high-dose methotrexate regimen guidelines
- As a part of combination with immunochemotherapy regimen: 3,000 mg/m2 to 8,000 mg/m2 followed by leucovorin rescue in accordance with high-dose methotrexate regimen guidelines
- 2.5 mg orally 2 to 4 times per week (maximum 10 mg per week) as part of a metronomic combination chemotherapy regimen
Comments:
- The recommended dose for intrathecal methotrexate injection (preservative-free) depends on the individual's age. Refer dosing provided in the meningeal leukemia section.
- The frequency of administration differs depending on whether it is used for treatment or prophylaxis, as well as other relevant factors.
Use: For the treatment of pediatric patients with non-Hodgkin's lymphoma
Usual Pediatric Dose for Osteosarcoma
Usual dose:
- As a part of a combination chemotherapy regimen: 12 g/m2 (maximum 20 g/dose) as an intravenous infusion over 4 hours
Comments:
- Administer leucovorin rescue in accordance with high-dose methotrexate regimen guidelines.
- Based on the observed peak serum methotrexate concentrations, adjustments to subsequent doses may be necessary.
- The dosage and schedule may vary depending on factors such as patient comorbidities, disease state, and previous treatments.
Use: For the treatment of pediatric patients with osteosarcoma as part of a combination chemotherapy regimen
Renal Dose Adjustments
Data not available
Comment: Consider reducing the dose or discontinuing this drug for renal impairment as appropriate.
Liver Dose Adjustments
Data not available
Comment: Consider reducing the dose or discontinuing this drug in patients with hepatic impairment as appropriate.
Dose Adjustments
Discontinue this drug for:
- Anaphylaxis or other severe hypersensitivity reactions
- Lymphoproliferative disease
Withhold, dose reduce or discontinue this drug as appropriate for:
- Myelosuppression
Withhold or discontinue this drug as appropriate for:
- Serious infections
- Renal toxicity
- Hepatotoxicity
- Neurotoxicity
- Gastrointestinal toxicity
- Pulmonary toxicity
- Dermatologic reactions
Precautions
US BOXED WARNINGS:
EMBRYO-FETAL TOXICITY, HYPERSENSITIVITY REACTIONS, BENZYL ALCOHOL TOXICITY, AND OTHER SERIOUS ADVERSE REACTIONS
- This drug has the potential to cause harm to the developing embryo or fetus, leading to fetal death. In cases of non-neoplastic diseases, this drug should not be used during pregnancy. It is important to advise individuals of reproductive potential, both females and males, to use reliable contraception methods.
- This drug is contraindicated in patients with a history of severe hypersensitivity reactions to methotrexate, including anaphylaxis.
- Formulations containing benzyl alcohol can lead to significant central nervous system toxicity or metabolic acidosis. When treating neonates or low-birth weight infants and for intrathecal use, exclusively employ preservative-free formulations. Benzyl alcohol-containing formulations should not be used for high-dose regimens, unless immediate treatment is necessary and preservative-free formulations are unavailable.
- This drug has been associated with other severe adverse reactions, including death. It is important to closely monitor for infections and adverse reactions affecting various organs such as the bone marrow, kidneys, liver, nervous system, gastrointestinal tract, lungs, and skin. If necessary, this drug should be withheld or discontinued as appropriate.
CONTRAINDICATIONS:
- History of severe hypersensitivity to this drug
- Pregnancy in patients with non-neoplastic diseases
Safety and efficacy have been established in patients with ALL, meningeal leukemia prophylaxis and treatment, non-Hodgkin lymphoma, osteosarcoma and in pJIA. Safety and effectiveness of this drug have not been established in pediatric patients for the treatment of breast cancer, squamous cell carcinoma of the head and neck, gestational trophoblastic neoplasia, rheumatoid arthritis, and psoriasis.
Consult WARNINGS section for additional precautions.
Dialysis
This drug is dialyzable via hemodialysis using a high flux dialyzer; however, no dose adjustment guidelines have been reported.
Other Comments
Administration advice:
- This drug should be used only by physicians who have knowledge and experience in the use of antimetabolite therapy because of the possibility of serious toxic reactions.
- Oral tablets are preferred when low doses are being administered since absorption is rapid and effective serum levels are obtained.
- The injectable form of this drug can be given by the IM, IV, subcutaneous, or intraarterial route. For intrathecal and high-dose therapy, the preservative-free formulation should be used (not the preserved formulation because it contains benzyl alcohol).
Storage requirements:
- Store at 20C to 25C (68F to 77F); excursions permitted to 15C to 30C (59F to 86F).
General:
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- To minimize the risk of severe adverse reactions, the following measures should be taken:
- Leucovorin rescue should be administered to patients receiving this drug at a dose of 500 mg/m2 or higher.
- Consider leucovorin rescue for patients receiving this drug at doses between 100 mg/m2 and less than 500 mg/m2. Additional information can be found in the leucovorin prescribing information.
- For intermediate or high-dose regimens of this drug, adhere to the supportive care and monitoring instructions below:
- Monitor baseline and daily electrolyte and serum creatinine levels during therapy.
- Begin intravenous fluid administration before the first dose and maintain adequate hydration and urine output throughout treatment.
- Maintain a urinary pH of 7 or higher by alkalinizing the urine, starting before the first dose and continuing throughout treatment.
- Monitor methotrexate concentrations at least daily and make adjustments to hydration and leucovorin dosage as necessary.
- In cases where patients have toxic plasma methotrexate concentrations (greater than 1 micromole per liter) and delayed methotrexate clearance due to impaired renal function, glucarpidase should be administered.
Patient advice:
- Inform females of reproductive potential about the potential risk to a developing fetus and advise them to notify their healthcare provider if they are pregnant or suspect a pregnancy.
- Advise females of reproductive potential to use effective contraception during the treatment with this drug and for 6 months following the final dose.
- Advise males of reproductive potential to use effective contraception during therapy and for 3 months after the final dose.
- Advise patients of the potential risk of hypersensitivity reactions and the contraindication of this drug in patients with a history of severe hypersensitivity to methotrexate. Promptly seek medical attention if signs or symptoms of a hypersensitivity reaction occur.
- Instruct patients to immediately contact their healthcare provider if they experience new-onset fever, signs of infection, easy bruising, or persistent bleeding.
- Inform patients about the possibility of methotrexate-induced renal toxicity. Promptly notify healthcare provider if there is a significant increase or decrease in urinary output.
- Advise patients to report any signs or symptoms of liver toxicity and to avoid consuming alcohol during methotrexate treatment.
- Instruct patients to contact their healthcare provider immediately if they develop new neurological symptoms.
- Advise patients to inform their healthcare provider if they experience diarrhea, vomiting, or stomatitis. Additionally, immediate medical attention should be sought for high fever, severe abdominal pain, persistent constipation, hematemesis, or melena.
- Inform patients to promptly contact their healthcare provider if they develop symptoms such as cough, fever, or difficulty breathing.
- Advise patients that this drug can cause severe skin rash and to notify their healthcare provider of any new or worsening skin rash. Caution them to avoid excessive sun exposure and to use appropriate sun protection measures.
- Inform patients about the potential risk of developing second primary malignancies during the treatment.
- Advise women not to breastfeed while undergoing treatment and for 1 week after the final dose.
- Inform females and males of reproductive potential about the potential of this drug to impair fertility.
- Instruct patients and caregivers to inform their healthcare provider about all medications, including prescription drugs, over-the-counter medications, vitamins, and herbal products that they are taking.
- For patients receiving treatment for neoplastic conditions, caution against using products containing folic acid or folinic acid unless specifically directed by their healthcare provider.
Frequently asked questions
- How long does chemo take? Sessions and recovery time?
- Why should I take folic acid with methotrexate?
- How long does it take for methotrexate to work?
- Does methotrexate cause weight gain?
- How do I know if methotrexate is working for rheumatoid arthritis?
- Radiation vs. Chemo: Which cancer treatment is right for you?
- What is chemo brain and how long does it last?
- What are the different brands of methotrexate?
- How soon can you start chemo after port placement?
More about methotrexate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (339)
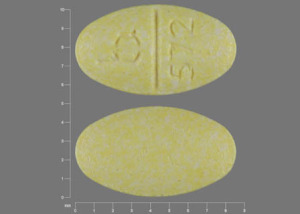
- Drug images
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: antimetabolites
- Breastfeeding
Patient resources
Other brands
Otrexup, Rasuvo, Trexall, Xatmep, ... +3 more
Professional resources
Other brands
Otrexup, Rasuvo, Trexall, Xatmep, ... +3 more
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.