Acute Lymphocytic Leukemia in Children
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is acute lymphocytic leukemia (ALL)?
ALL is a type of cancer that affects the blood and bone marrow. The bone marrow makes white blood cells (WBC), red blood cells (RBC), and platelets. WBCs help fight infection. RBCs help to carry oxygen throughout the body. Platelets help the blood clot. ALL causes your child's body to make too many immature (young) white blood cells. These cells are cancer (leukemia) cells and cannot fight infection like healthy WBCs. Cancer cells crowd the bone marrow and prevent it from making healthy blood cells. Without enough healthy blood cells, your child is at risk for infection, bleeding, and anemia. Anemia is a low level of red blood cells.
What causes ALL?
The exact cause is unknown. ALL is most common in children younger than 10 years. The following may increase your child's risk for ALL:
- Being exposed to x-rays before birth
- A history of cancer treatment with chemotherapy or radiation
- Certain genetic conditions, such as Down syndrome and Li-Fraumeni syndrome
- A brother or sister with ALL
What are the signs and symptoms of ALL?
- Fever
- Night sweats
- Easy bleeding or bruising
- Small red spots on your child's skin
- Bone, rib, or joint pain
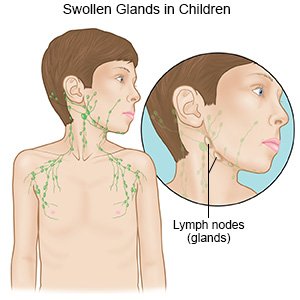
- Swollen lymph nodes in your child's neck, armpits, or groin
- Weakness, feeling tired, or looking pale
- Loss of appetite or weight loss
How is ALL diagnosed?
- Blood tests check your child's blood cell levels.
- X-rays check for swollen lymph nodes in your child's chest.
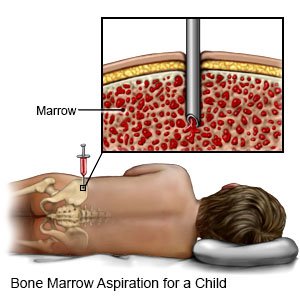
- A bone marrow biopsy is a procedure to take a sample of bone marrow from your child's hip bone. This test helps healthcare providers find out which type of leukemia your child has.
- A lumbar puncture is a procedure to remove fluid from around your child's spinal cord. The fluid can be tested for cancer.
How is ALL treated?
Treatment may depend on your child's age and the results of testing. Your child may get treatment in phases. In the first phase, healthcare providers will give your child treatments to kill leukemia cells. This helps your child's ALL go into remission. Remission means there are no longer any signs of leukemia. After your child is in remission, he or she will get the next phase of treatment, called consolidation or intensification. The goal of this phase is to kill any hidden leukemia cells and prevent relapse. The third phase is called maintenance. The goal of this phase is to kill leukemia cells that may regrow. Treatment may include the following:
- Supportive care includes medicines and blood transfusions. Medicines may be given to prevent infections. Blood transfusions may be given to increase your child's level of red blood cells, white blood cells, or platelets.
- Chemotherapy is the main treatment used to kill cancer cells. Your child's healthcare provider may give him or her different types of chemotherapy. Ask your child's healthcare provider for more information about the types of chemotherapy.
- Targeted therapy is medicine that finds and kills cancer cells.
- Radiation therapy shrinks tumors and kills cancer cells with x-rays or gamma rays. It may be given alone or with chemotherapy to treat cancer.
- A stem cell transplant is a procedure to replace cancer cells with healthy blood cells. Stem cells are taken from a donor and injected into your child's blood. The stem cells go to his or her bone marrow and become new, healthy blood cells.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Drugs used to treat this and similar conditions
Neupogen
Neupogen (filgrastim) is used to treat neutropenia, a lack of certain white blood cells caused by ...
NovoSeven RT
NovoSeven RT (coagulation Factor VIIa, recombinant) is an injectable, coagulation factor VIIa that ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Doptelet
Doptelet (avatrombopag) is used to treat thrombocytopenia in patients with chronic liver disease ...
Promacta
Promacta is used to prevent bleeding episodes in patients with chronic immune (idiopathic) ...
Rituximab
Rituximab is a monoclonal antibody drug used to treat non-hodgkin lymphoma, chronic lymphocytic ...
Coagulation factor viia
Coagulation factor viia systemic is used for factor vii deficiency, glanzmann's disease, hemophilia ...
Dexamethasone
Dexamethasone is used to treat inflammatory conditions such as allergies, skin conditions ...
Avatrombopag
Avatrombopag systemic is used for immune thrombocytopenia, thrombocytopenia
Filgrastim
Filgrastim systemic is used for aplastic anemia, bone marrow transplantation, hematopoietic ...
How can I manage my child's ALL?
- Prevent infection in your child. Wash your hands and your child's hands often. Keep your child away from people who are sick. Ask your child's healthcare provider for more information on how to prevent infection.

- Prevent bleeding and bruising in your child. Do not let your child play contact sports, such as football. Use a soft toothbrush to clean your child's teeth. Do not floss your child's teeth while his or her platelet count is low. Have your child blow his or her nose gently. Do not give your child's NSAIDs or aspirin. NSAIDs and aspirin prevent platelets from helping the blood clot. This increases your child's risk for bleeding.
- Give your child plenty of liquids as directed. Your child may need to drink extra liquids to prevent dehydration. Dehydration is possible if your child is vomiting or has diarrhea from cancer treatments. Ask how much liquid to give your child each day and which liquids are best for him or her.
- Help your child find ways to exercise. ALL or its treatment may make your child feel tired. Exercise can help your child have more energy. Ask his or her provider what exercises are safe for your child.
- Feed your child healthy foods. Healthy foods may help your child feel better and have more energy. Examples of healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask if your child needs to be on a special diet. Ask about any extra nutrition your child may need, such as nutrition shakes or vitamins.

Further information
It may be difficult for your child to go through cancer treatment. Ask your child's healthcare provider for information about camps for children with cancer.
- The Leukemia & Lymphoma Society Inc.
1311 Mamaroneck Avenue
White Plains , NY 10605
Phone: 1- 914 - 949-5213
Phone: 1- 800 - 955-4572
Web Address: http://www.leukemia-lymphoma.org
Call your local emergency number (911 in the US) if:
- Your child feels short of breath or has chest pain.
- Your child hardly moves, speaks, or opens his or her eyes.
- Your child faints or loses consciousness.
When should I seek immediate care?
- Your child's temperature is greater than 100.4°F (38°C).
- Your child has heavy bleeding.
- Your child's heart is beating faster than usual.
- Your child has blood in his urine or bowel movement.
When should I call my child's doctor?
- Your child has bruising not caused by an injury.
- Your child has nausea or is vomiting.
- Your child has trouble eating.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Acute Lymphocytic Leukemia
Treatment options
Symptoms and treatments
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
