Middle Ear Infection FAQs (Acute Otitis Media)
What is a middle ear infection?
If you’re a parent you know about ear infections, a common condition that affects children at a very young age. The late night tears, the ear tugging, the repeated trips to the pediatrician, and the pink liquid antibiotic. It’s a familiar scene. As consistently predictable as this routine seems, acute otitis media (AOM) - the medical term for the most common type of ear infection - can be more complicated.
Acute otitis media (AOM) is a swollen and often infected middle ear where fluid builds behind the eardrum and leads to pain. Infections can be viral, bacterial or a combination of both. AOM is also the most common diagnosis in a pediatrician’s office.
Roughly 25% of all infants in developed countries will have at least one ear infection by their first birthday. By age three, up to 60% of children have had an ear infection and over 25% will have had three or more. Children in day care are more prone to ear infections After respiratory infections, AOM is the second most common diagnosis in the emergency department.
Acute otitis media is less frequent in older school-age children, adolescents, and adults, but may still occur.
Common ear infection questions you might ask your doctor include:
- What are the symptoms of an ear infection?
- What are the risk factors?
- How do you diagnose an ear infection?
- Which medicines treat an ear infection?
- What if my child has frequent middle ear infections?
- Plane Travel - What to do?
- Can I prevent an ear infection?
- Are there alternative treatments for otitis media?
- What are other related ear conditions?
- How can I keep up with the latest medical news on ear infections?
What is acute otitis media?
Acute Otitis Media (AOM) is an infection in one or both ears. An “acute” ear infection is a short-term and painful ear infection that may come on quickly. This is in contrast to a Chronic Ear Infection that may last a longer time, come and go, and lead to permanent hearing damage.
- Acute otitis media (AOM) is a swelling and infection of the middle ear. "Otitis" means ear and "media" means middle. The middle ear is located just behind the eardrum. The eustachian tube in the middle ear drains fluid away from the middle ear and connects to the back of the nose and throat.
- When fluid builds up in the eustachian tube, it can lead to an increase in pressure on the eardrum, which results in pain. The ear can become infected with bacteria (germs), which can grow in the trapped fluid behind the eardrum.
- Ear infections are common in infants and toddlers (ages 6 to 24 months) because the eustachian tubes are more narrow and horizontal and can become easily clogged.
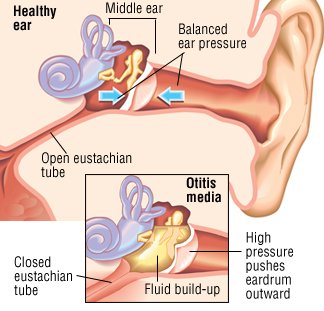
Image: Harvard Health Guide
Ear infections can be more common in children who also have a cold or flu due to a virus. Symptoms of an ear infection may begin during the 3rd to 7th day of a viral infection. Children with an ear infection usually also have a runny nose and nasal congestion.
Mild hearing loss may occur, but it is usually temporary. However, if hearing loss lasts an extended period of time, it may cause problems with speech, language and learning.
1. What are the symptoms of an ear infection?
If you think your child has an ear infection, see your pediatrician. They can make an accurate diagnosis, look for complications, and prescribe the appropriate medications, if needed. Keep in mind treatment for an acute ear infection is not always needed.
A telltale sign of an ear infection is a bulging tympanic membrane (ear drum), as visualized by your doctor with an otoscope (a medical device that looks into the ears), and ear pain. Older children may also experience hearing loss.
In younger children and infants, the symptoms of an ear infection may include:
- tugging on the ears, ear pain (especially when lying down)
- fever over 100.4 degrees F (38 degrees C)
- temporary hearing loss or trouble hearing
- trouble sleeping
- dizziness or loss of balance
- yellow fluid or pus draining from ear (otorrhea)
- irritability, fussiness, inconsolable crying
- loss of appetite
- vomiting, diarrhea (in infants)
Visit the Drugs.com Symptom Checker
See the Drugs.com Symptom Checker to make an informed decision in conjunction with your healthcare provider.
Related
2. What causes an ear infection?
Anything that causes the eustachian tubes to become swollen or blocked can lead to ear infections. These might include:
- allergies
- the common cold
- excess mucus and saliva produced during teething
- infected or overgrown adenoids
- tobacco smoke (second-hand smoke) or other irritants
Other factors that may increase your child’s chances of developing an ear infection include:
- age: acute otitis media peaks between 6 and 24 months of age
- ear infections before 6 months of age
- family history of ear infections
- day care and school attendance
- seasonal factors: fall, winter and early spring months
- child not breastfed
- drinking from bottle or "sippy" cup while lying flat
- use of a pacifier after 10 months of age
- medical conditions like a cleft palate or Down syndrome
- a recent ear infection
- lack of access to medical care
- Alaska Native heritage
Ear infections are not contagious, but viral colds are contagious and may spread through a daycare center or school and increase the risk of getting an ear infection.
Common organisms that may lead to ear infections include the bacteria Streptococcus pneumoniae, Hemophilus influenza and Moraxella catarrhalis. These bacteria may be responsible for more than 95% of bacterial earache infections. Viruses can include RSV (respiratory syncytial virus), coronavirus that causes COVID-19, influenza (flu viruses) and adenoviruses.
Drainage of green or yellow fluid out of the ear may indicate that there is a ruptured eardrum.
3. How is an ear infection diagnosed?
First, your doctor will ask about how long symptoms have been present, presence of ear pain, any discharge from the ear, and if there has been a fever. Your doctor may also inquire about a previous history of ear infections.
- Your healthcare provider can look into your child’s ear to see if there is an infection. An instrument called an otoscope, a cone-shaped tool with a light, is used to view the eardrum.
- Your healthcare provider may look for areas of dullness or redness, fluid behind the eardrum, blood or pus inside the middle ear, or a perforated eardrum (a hole in the eardrum).
- The doctor may use a puff of air to see if the eardrum moves or do a test called a tympanogram that measures how the eardrum moves.
- Sometimes wax (cerumen) may block the ear and this will need to be removed.
- A hearing test or other more advanced tests may rarely be needed in more hard-to-treat cases.
4. Which medicines are used to treat otitis media?
Some children will get better without specific antibiotic treatment, as many ear infections are viral in nature and do not need an antibiotic. Doctors may prescribe antibiotics in infants under 6 months of age, and for recurrent ear infections or severe symptoms. However, using antibiotics too often can cause bacteria to become resistant to the medicine, which lowers the effectiveness of the treatment.
Antibiotics are commonly given to children under 24 months of age or with high fever or infections in both ears. These children tend to get better more quickly with antibiotics.
In more serious cases in older children, when there is recent high fever, both ears are affected, or ear drainage, an antibiotic treatment may be appropriate.
Antibiotic choice should be based on effectiveness, patient-specific needs like allergies, taste or dosage form preference, dosing convenience and cost. It’s important to remember that although most antibiotics used for ear infections are very safe, there may still be side effects such as diarrhea or rash from antibiotic use.
Some doctors may recommend a "wait-and-see" approach for certain children with ear infections, for example:
- if the child is otherwise healthy
- if ear pain and fever are not severe
- in children 24 months and older
Parents will usually follow-up with the doctor in 2 to 3 days with the “wait-and-see” or observation approach. With or without treatment, if your child does not improve within 72 hours or gets worse, contact the healthcare provider
Talk with your doctor about the potential benefits and risks of using antibiotics. When needed, antibiotics recommended for otitis media (ear infection) treatment may include:
First-line treatment
When antibiotic therapy is recommended, the following therapies are suggested:
Amoxicillin or Amoxicillin-Clavulanate
High-dose oral amoxicillin given for 5 to 10 days is the treatment of choice in most cases. Younger children, those with a perforated eardrum, and recurrent cases are treated for 10 days, and those over 2 years of age are treated 5 to 7 days. Amoxicillin is a good choice for otitis media because it concentrates well in the middle ear. Follow your doctor's dosing instructions.
Another option is high-dose oral amoxicillin-clavulanate (Augmentin). This treatment is recommended in patients who have been treated with amoxicillin in the previous month, in those with purulent conjunctivitis ("pink eye" with a thick, pus-like discharge), or who have recurrent AOM and have failed previous amoxicillin treatment.
If the patient has a mild (delayed) penicillin allergy (without anaphylaxis, bronchospasm, or angioedema), one of these cephalosporins may be an option, usually given for either 10 days or 5 to 7 days:
- cefdinir
- cefpodoxime
- cefuroxime tablets (suspension no longer available in US)
Ceftriaxone intramuscular (IM) ir intravenous (IV) injection may also be used (for one to three doses, based on symptom improvement) if patients are vomiting or cannot have oral treatment.
If there is a severe (immediate) or serious delayed penicillin allergy, which also includes a severe allergy with cephalosporins, select from these oral macrolide options, or oral clindamycin:
If these treatments are not effective within 2 to 3 days, alternative antibiotics or an appointment with a pediatric ear-nose-throat (ENT) specialist doctor may be needed.
Ear Pain
Treatments recommended for ear pain include:
- acetaminophen (brand: Tylenol)
- ibuprofen (brand: Advil, Motrin)
Ask your doctor about the best ear pain dose for your child's age and weight. Follow your doctor's directions or the directions found on the Drug Facts Label of any over-the-counter (OTC) product.
- Acetaminophen will decrease pain and fever and is available over-the-counter (OTC). Ibuprofen is used to help with pain, fever and swelling and is also available OTC.
- Check for acetaminophen in all medicines your child receive to be sure you do not exceed the maximum daily dose. Too much acetaminophen can cause liver damage.
- Ibuprofen is used to help with pain, fever and swelling and is also available OTC. Ask your doctor if this medicine is safe for your child. It can cause stomach bleeding and kidney problems.
Do NOT give aspirin to a child or teenager with a fever, flu symptoms, or chickenpox. Use of aspirin in children can lead a dangerous condition known as Reye's Syndrome which can lead to serious problems with the brain and liver.
Tip: You should talk to your doctor first if you decide to use any ear drops to treat ear pain in your child. Some ear drops may not be safe to use (see below).
5. What if my child has frequent middle ear infections?
Recurrent ear infections can be a problematic for both parent and child. A child is considered “otitis prone” when they have 3 ear infections within a 6 month period or 4 infections within a year.
Risk factors that may increase the frequency of ear infections include:
- male gender
- winter season
- exposure to passive smoke
- symptoms lasting longer than 10 days
The insertion of tympanostomy tubes (ear tubes) may be recommended in recurrent cases. The American Academy of Pediatrics recommends tube placement consideration in patients who have had 4 or more middle ear infections in the past 12 months.
While there are inherent risks with any surgical procedure, they are infrequent with ear tube insertion. The benefits of ear tubes include fewer ear infections, maintenance of hearing and the ability to treat future infections with topical antibiotic therapy (ear drops) instead of oral drugs.
In July 2015, the FDA announced they were targeting 16 unapproved ear drop ingredients often used in infants and young children. These drugs, prescribed and sold for years to relieve ear pain and swelling, had not been evaluated for safety, quality and effectiveness. The agency notified the manufacturers to stop marketing the drops following reports of local allergic reactions of the ear, eye, face, neck and mouth. The drops can also cause itching, stinging, burning and irritation of the ear.
The products covered by this action include:
- benzocaine
- benzocaine and antipyrine
- benzocaine, antipyrine, and zinc acetate
- benzocaine, chloroxylenol, and hydrocortisone
- chloroxylenol and pramoxine
- chloroxylenol, pramoxine, and hydrocortisone.
6. Plane travel: How to avoid airplane ear?
Airplane ear (also called ear barotrauma) is the stress on your eardrum that occurs when there's a difference in the air pressure in your middle ear and the outside air. You or your child might get airplane ear during takeoff or when landing during a flight. It can occur in one or both ears, and may lead to feeling of fullness, ear pain, or a slight hearing loss or muffled sound.
To help young children:
- Encourage your child or baby to swallow. Give a baby or toddler a bottle or pacifier to suck on during take-off and landings to encourage swallowing. Children older than 4 years can try chewing gum, swallowing, drinking through a straw or blowing bubbles through a straw.
- Avoid decongestants. Decongestants, like phenylephrine or pseudoephedrine, aren't recommended for young children.
- If your child has had surgery on the ear, ask your doctor when it is safe for them to fly.
Here's more information on what to do if you or your child has upcoming plane travel.
7. How can I prevent an ear infection in my child?
Vaccines are available to help minimize ear infections in children, and are part of the normal routine vaccine schedule for pediatrics. Children should be immunized against the common bacteria that cause middle ear infections.
Be sure your child gets the required pneumococcal conjugate vaccines. In addition, most children 6 months and older should receive a seasonal influenza (flu) vaccine each year (usually in Sept or Oct), as recommended by the CDC. Follow your pediatrician's directions for COVID-19, Respiratory Syncytial Virus (RSV), Haemophilus and other childhood vaccines, as well.
Wash your hands and your child's hands frequently. Teach them to wash hands with soap and water for 20 seconds after bathroom use and before eating food. Adults should also wash hands after a diaper change.
Also, to help reduce the risk of recurrent infections:
- Keep your child away from sick children, when possible.
- Strongly consider breastfeeding your baby.
- Do not give a bottle when your child is lying down.
- Keep your child away from tobacco smoke, which can make an ear infection worse.
- Avoiding daily use of oral xylitol, a sugar substitute.
In some cases, the placement of ear tubes may be recommended for children who have frequent ear infections.
8. Are there alternative treatments for ear infections?
Complementary and alternative medical treatments are NOT recommended for ear infections in children. Home remedies for ear infections, such as olive oil and herbal extracts have not been proven to have any effect.
Get a diagnosis from your pediatrician to help prevent further complications in your child.
9. Related ear conditions
Similar conditions of the middle ear that may be related to an ear infection or result in similar middle ear problems include the following:
- Otitis media with effusion (OME) refers to middle ear fluid build-up that is NOT infected. Fluid may remain after an ear infection has cleared up or due to a blocked eustachian tube. Antibiotics are NOT required for this condition. In most children the fluid build-up will resolve on its own within 4 to 6 weeks and treatment is not usually needed.
- Chronic suppurative otitis media is a persistent ear infection that results in tearing or perforation of the eardrum.
- Otitis externa (Swimmer’s ear) is an infection in the outer ear canal that goes from the outside of the ear to the eardrum.
If you suspect any problems of the ear, contact your child's pediatrician for an evaluation right away.
10. Join the Drugs.com Otitis Media support group
While you should always follow your doctor's medical advice, you might consider joining the Drugs.com Otitis Media Support group to ask questions and share experiences with those who have similar questions and concerns about ear infections.
You can also keep up with the latest ear infection news and approvals in the Drugs.com Otitis Media Support Group.
Related Topics
See also
- Antibiotic Resistance: The Top 10 List
- Antibiotics - Common Side Effects, Allergies and Reactions
- Antibiotics and Birth Control Pill Interactions
- Antibiotics for UTI Treatment
- Can You Drink Alcohol with Antibiotics?
- Why Don’t Antibiotics Kill Viruses?
Learn more
Treatment options
- Medications for Acute Otitis Externa
- Medications for Bacterial Infection
- Medications for Chronic Otitis Media
- Medications for Ear Conditions
- Medications for Middle Ear Infections
- Medications for Otitis Media with Perforation of Ear Drum
Care guides
Symptoms and treatments
Medicine.com guides (external)
Sources
-
Danishyar A, Ashurst JV. Acute Otitis Media. [Updated 2023 Apr 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470332/
- Tahtinen P, Frost H (authors). Up to Date. Patient Education: Ear infections (otitis media in children (Beyond the Basics). Nov. 4, 2024. Accessed Mar 19, 2025 at https://www.uptodate.com/contents/ear-infections-otitis-media-in-children-beyond-the-basics
- Acute Otitis Media with Effusion (OME). Children's Hospital of Philadelphia (CHOP). Accessed March 19, 2025 at https://www.chop.edu/conditions-diseases/otitis-media-effusion-ome
- Ear Infections. Kaiser Permanente. Accessed March 19, 2025 at https://m.kp.org/georgia/health-wellness/health-encyclopedia/he.hw184385
- Ahmed S, Shapiro NL, Bhattacharyya N. Incremental health care utilization and costs for acute otitis media in children. Laryngoscope. 2014 Jan;124(1):301-5. doi: 10.1002/lary.24190
- Allan S. Lieberthal, Aaron E. Carroll, Tasnee Chonmaitree, et al; The Diagnosis and Management of Acute Otitis Media. Pediatrics March 2013; 131 (3): e964–e999. 10.1542/peds.2012-3488
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
