Phenylephrine
Pronunciation: fee-nile-eff-frin
Generic name: phenylephrine
Brand names: Nasop12, Sudafed PE, Sudafed PE Children's Nasal Decongestant, Sudafed PE Congestion, Nasop,
... show all 24 brands
Dosage form: oral tablet, extended-release oral tablet, oral liquid, nasal spray, intravenous solution
Drug classes: Decongestants, Vasopressors
What is phenylephrine?
Oral and nasal phenylephrine are used as nasal decongestants to temporarily unblock a nose or relieve sinus pressure in people with nasal and sinus congestion caused by colds, allergies, or hay fever. While phenylephrine can provide some symptom relief, it doesn't treat the underlying cause or speed recovery.
Injectable phenylephrine may be used in a hospital setting to increase blood pressure in adults with significantly low blood pressure caused primarily by vasodilation (a widening of the blood vessels), as a result of septic shock or anesthesia.
Phenylephrine works by directly stimulating receptors in the blood vessels of the nose and other parts of the body (called alpha-1 adrenergic receptors), causing vasoconstriction (narrowing of the blood vessels). This reduces nasal congestion by preventing fluid from draining from the blood vessels into the tissues lining the nasal passages. At higher dosages, phenylephrine increases blood pressure and reduces heart rate and cardiac output (particularly in people with preexisting heart disease).
Phenylephrine has been available for over 60 years, which means it wasn't subject to the same rigorous scrutiny by the FDA as newer medicines.
Phenylephrine side effects
The most common side effects of phenylephrine include:
- flushing (warmth, redness, or tingly feeling)
- loss of appetite
- feeling restless or excited (especially in children).
Serious side effects and warnings
Get emergency medical help if you have signs of an allergic reaction, such as hives; difficulty breathing; or swelling of your face, lips, tongue, or throat.
Do not use if you are taking a monoamine oxidase inhibitor (MAOI) or have used one in the past 14 days (2 weeks). MAOIs include isocarboxazid, linezolid, methylene blue injection, phenelzine, rasagiline, selegiline, or tranylcypromine, and these are typically used for depression, psychiatric or emotional conditions, or Parkinson's disease, or 2 weeks after stopping the MAOI drug. If you do not know if your prescription drug contains an MAOI, ask a doctor or pharmacist before taking this phenylephrine.
Other reported side effects of phenylephrine include:
- Cardiac disorders: Bradycardia, AV block, ventricular extrasystoles, myocardial ischemia
- Gastrointestinal disorders: Nausea, vomiting
- General disorders and administrative site conditions: Chest pain, extravasation
- Immune system disorders: Sulfite sensitivity
- Nervous system disorders: Headache, nervousness, paresthesia, tremor
- Psychiatric disorders: Excitability
- Respiratory: Pulmonary edema, rales
- Skin and subcutaneous tissue disorders: Diaphoresis, pallor, piloerection, skin blanching, skin necrosis with extravasation
- Vascular disorders: Hypertensive crisis.
Stop using phenylephrine and call your doctor at once if you have:
- fast, pounding, or irregular heartbeat
- severe dizziness or nervousness
- sleep problems (insomnia)
- increased blood pressure. Symptoms may include a severe headache, blurred vision, and pounding in your neck or ears.
Liquid phenylephrine
The liquid form of this medicine may contain phenylalanine. Check the medication label if you have phenylketonuria (PKU).
Injectable phenylephrine
Some injectable preparations of phenylephrine contain sodium metabisulfite, a sulfite that may cause allergic reactions, including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
This is not a complete list of side effects. To report suspected side effects contact the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Related/similar drugs
Before taking
Do not use phenylephrine if you have used an MAO inhibitor in the past 14 days. A dangerous drug interaction could occur. MAO inhibitors include isocarboxazid, linezolid, methylene blue injection, phenelzine, rasagiline, selegiline, tranylcypromine, and others.
You should not use phenylephrine if you are allergic to it.
Ask a doctor or pharmacist if this medicine is safe to use if you have:
- heart disease or high blood pressure
- diabetes
- a thyroid disorder
- an enlarged prostate and urination problems
- any drug allergies.
If you are pregnant or breastfeeding, ask a health professional before use.
The liquid form of this medicine may contain phenylalanine. Check the medication label if you have phenylketonuria (PKU).
Pregnancy
It is also not known whether phenylephrine can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Phenylephrine hydrochloride should be given to a pregnant woman only if needed.
Use of phenylephrine during labor and delivery
The most common side effects reported in mothers receiving phenylephrine during neuraxial anesthesia during cesarean delivery include nausea and vomiting, which are commonly associated with low blood pressure, slow heartbeat, reactive high blood pressure, and short-lasting arrhythmias. Phenylephrine does not appear to cause a decrease in perfusion of the placenta that is significant enough to affect the baby's Apgar score or blood gas levels.
Breastfeeding
It is not known if phenylephrine is excreted in human milk.
How should I take phenylephrine?
Take phenylephrine exactly as directed on the label, or as prescribed by your doctor.
- Cold medicine is only for short-term use until your symptoms clear up.
- Always follow directions on the medicine label about giving cold medicine to a child.
- You must chew the phenylephrine chewable tablet before you swallow it.
- Measure phenylephrine liquid medicine carefully. Use the dosing syringe provided, or use a medicine dose-measuring device (not a kitchen spoon).
- Remove an orally disintegrating phenylephrine tablet from the package only when you are ready to take the medicine. Place the tablet in your mouth and allow it to dissolve, without chewing. Swallow several times as the tablet dissolves.
Stop taking phenylephrine and ask a doctor if nervousness, dizziness, or sleeplessness occur or symptoms do not improve within 7 days or occur with a fever, rash, or headaches.
If you need surgery, tell your surgeon if you are currently using phenylephrine.
Phenylephrine dosage
When using phenylephrine do not exceed recommended dose.
- The safety and effectiveness of using phenylephrine in children have not been established.
- The dosage of phenylephrine may need adjusting for liver or kidney disease.
Phenylephrine dosage for nasal congestion
- Adults and children 12 years and older. 10mg every 4 hours. Do not take more than 6 tablets in 24 hours.
- Children under 12 years. Ask a doctor.
Phenylephrine dosage for low blood pressure
Perioperative dosing (adults undergoing surgery with neuraxial or general anesthesia):
- Initial dose: 50 to 250 mcg by intravenous bolus (most common doses: 50 to 100 mcg)
- Maintenance dose: 0.5 to 1.4 mcg/kg/min by intravenous continuous infusion (titrate to blood pressure goal)
Septic or Other Vasodilatory Shock
- Adults: 0.5 to 6 mcg/kg/min by intravenous continuous infusion (titrate to blood pressure goal)
- No bolus
- Doses over 6 mcg/kg/min do not show significant incremental blood pressure increases.
Usual Adult Dose for Shock. Perioperative dosing (patients undergoing surgery with neuraxial or general anesthesia):
- Initial dose: 50 to 250 mcg by intravenous bolus (most common doses: 50 to 100 mcg)
- Maintenance dose: 0.5 to 1.4 mcg/kg/min by intravenous continuous infusion (titrate to blood pressure goal)
Does phenylephrine work?
Recently, an FDA advisory panel concluded that phenylephrine is not effective as an oral decongestant and does not significantly improve symptoms compared to a placebo (an inactive pill).
Phenylephrine has been available for more than six decades but it came into use before the FDA developed a stringent approval process for new medicines back in the 1970s and received marketing authorization based on pre-existing use.
A reason for phenylephrine’s lack of effectiveness includes the fact that, even though it is well absorbed from the stomach, it undergoes extensive metabolism in the gut wall. This means only about 40% of a dose reaches the bloodstream and only 3% is excreted unchanged.
Phenylephrine is currently allowed by the FDA as a medicine based on in-house studies provided by pharmaceutical companies, not as a result of clinical trials. These unpublished studies ranged from mild successes to total failures, and a recommendation that phenylephrine should not be accepted as an oral nasal decongestant was made in 1994 but ignored. However, the efficacy of phenylephrine as a nasal spray for nasal congestion is supported by several studies.
On September 14, 2023, the FDA Drug Advisory Committee concluded that current data does not support the effectiveness of phenylephrine as an oral nasal decongestant, although there were no concerns about any toxicity at recommended dosages.
What happens if I miss a dose?
Phenylephrine for nasal symptoms is usually taken as needed according to the recommended dose so if you miss a dose, just go back to your regular dosing schedule. Do not double up the dose or take extra to make up for the next dose.
What happens if I overdose?
In case of overdose, get medical help or contact a Poison Control Center right away. (1-800-222-1222).
An overdose of phenylephrine can cause a rapid rise in blood pressure. Symptoms of overdose include headache, vomiting, high blood pressure, reflex slow heart rate, and cardiac arrhythmias, which may cause a sensation of fullness in the head and tingling of the hands and feet.
Storage
Store phenylephrine tablets and nasal spray between 20-25°C (68-77°F).
Do not use it if the blister unit is torn or broken.
Keep out of reach of children.
Phenylephrine ingredients
Active: phenylephrine
Inactive. Inactive ingredients in phenylephrine tablets, nasal sprays, and injections, vary depending on the manufacturer. See the phenylephrine package insert for each particular manufacturer for a list of inactive ingredients.
What other drugs will affect phenylephrine?
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Phenylephrine and other medicines can affect each other causing side effects.
Drugs that cause the uterus to contract (oxytocic drugs) can strengthen the blood pressure-increasing effect (pressor effect) of phenylephrine.
The blood vessel narrowing (vasoconstrictive) effects of phenylephrine are increased in patients receiving:
- Monoamine oxidase inhibitors (MAOI), such as selegiline.
- β-adrenergic blockers
- α-2 adrenergic agonists, such as clonidine
- Steroids
- Tricyclic antidepressants
- Norepinephrine transport inhibitors, such as atomoxetine
- Ergot alkaloids, such as methylergonovine maleate
- Centrally-acting sympatholytic agents, such as guanfacine or reserpine
- Atropine sulfate.
α-adrenergic blocking agents, including phenothiazines (e.g., chlorpromazine) and amiodarone block phenylephrine and are in turn blocked by phenylephrine.
Know the medications you take and the vaccines you receive. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine. See the phenylephrine package insert for a full list of interactions.
Who makes phenylephrine?
Johnson & Johnson Consumer Inc. makes phenylephrine 10 mg tablets as Sudafed PE Sinus Congestion.
Various generic manufacturers, such as Hikma Pharmaceuticals USA Inc., Nuvicare LLC, Cantrell Drug Company, and Rugby Laboratories make phenylephrine.
Popular FAQ
Phenylephrine vs Pseudoephedrine - How do they compare?
The most important difference between phenylephrine (PE) and pseudoephedrine is that phenylephrine is ineffective at relieving nasal congestion, whereas there is some evidence that oral pseudoephedrine is effective. Continue reading
Does Mucinex help with Covid?
Mucinex products do not help to prevent or treat the COVID-19 virus itself, but might help relieve some of the symptoms of COVID, like chest congestion, cough, or headache. Select a product that targets only the symptoms you have. Continue reading
References
More about phenylephrine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (24)
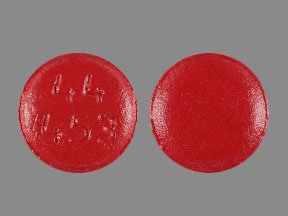
- Drug images
- Latest FDA alerts (5)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: decongestants
- Breastfeeding
- En español
Patient resources
- Phenylephrine (Intravenous) advanced reading
- Phenylephrine Tablets
- Phenylephrine Injection
- Phenylephrine Liquid
Other brands
Sudafed PE Congestion, Neo-Synephrine, Biorphen, Contac-D, ... +2 more
Professional resources
Other brands
Neo-Synephrine, Biorphen, Vazculep
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.