Clindamycin Phosphate (Topical) (Monograph)
Brand names: Cleocin, Cleocin T, Clinda-Derm, Clindagel, Clindesse, Clindets
Drug class: Antibacterials
Introduction
Antibacterial; broad-spectrum antibiotic derived from lincomycin.
Uses for Clindamycin Phosphate (Topical)
Acne Vulgaris
Treatment of inflammatory acne vulgaris; used alone or in conjunction with benzoyl peroxide.
Generally effective for treatment of mild to moderate inflammatory acne.
May induce bacterial resistance when used as monotherapy; resistance associated with decreased clinical efficacy.
Particularly useful when used in combination with benzoyl peroxide or topical retinoids; reduction in total lesion count of 50–70% reported when combination therapy used.
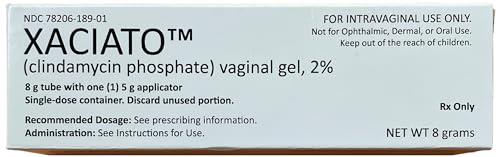
Bacterial Vaginosis
Treatment of bacterial vaginosis (formerly called Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis).
CDC recommends treatment of bacterial vaginosis in all symptomatic women (including pregnant women). In addition, asymptomatic pregnant women at high risk for complications of pregnancy should be screened (preferably at the first prenatal visit) and treatment initiated if needed.
Treatment recommendations for bacterial vaginosis in HIV-infected women are the same as those for women without HIV infection.
Regimens of choice in nonpregnant women are a 7-day regimen of oral metronidazole; a 5-day regimen of intravaginal metronidazole gel; or a 7-day regimen of intravaginal clindamycin cream; alternative regimens are a 7-day regimen of oral clindamycin or 3-day regimen of intravaginal clindamycin suppositories. The preferred regimens for pregnant women are a 7-day regimen of oral metronidazole or oral clindamycin.
Regardless of regimen used, relapse or recurrence is common; an alternative regimen (e.g., oral therapy when topical was used initially) may be used in such situations.
Routine treatment of asymptomatic male sexual contacts of women who have relapsing or recurrent bacterial vaginosis not recommended.
Clindamycin Phosphate (Topical) Dosage and Administration
Administration
Administer topically to the skin or intravaginally in appropriate formulations.
Topical skin preparations are for external use only and should not be used orally, intravaginally, or near or in eyes or mucous membranes.
Intravaginal preparations are for intravaginal administration only and should not be used orally, topically on the skin, or near or in eyes.
Topical Administration
Apply topically to the skin as a gel, lotion, or solution containing clindamycin 1% or as a gel containing clindamycin 1% in combination with benzoyl peroxide 5%. Apply to all areas of skin prone to acne.
Do not use near eyes, nose, mouth, or other mucous membranes.
Shake lotion well immediately prior to use.
Remove solution-containing pledgets from their foil immediately before use; do not use if seal is broken. Use each pledget only once and then discard; may use more than 1 pledget for each application if needed to cover the affected area.
Reconstitution
BenzaClin
Prepare BenzaClin topical gel containing clindamycin and benzoyl peroxide at the time of dispensing.
Reconstitute vial containing clindamycin powder by adding 5 mL of purified water and shaking immediately to completely dissolve the drug; if needed, add additional purified water to bring level up to the mark on the vial.
Add the reconstituted clindamycin solution to the benzyl peroxide gel provided by the manufacturer; stir until homogenous in appearance (1 to 1.5 minutes).
Duac
Duac topical gel containing clindamycin and benzoyl peroxide does not need reconstitution and is used as provided by the manufacturer.
Intravaginal Topical Administration
Administer intravaginally as a cream containing clindamycin 2% or as 100-mg vaginal suppositories.
Dosage
Pediatric Patients
Acne Vulgaris
Maintenance therapy needed to prevent recurrence.
Single-entity Clindamycin Preparations
TopicalChildren ≥12 years of age: apply a thin film of gel, lotion, or solution to the cleansed affected area twice daily.
Clindamycin and Benzoyl Peroxide Combination Preparations
TopicalChildren ≥12 years of age: apply a thin film of BenzaClin gel to the cleansed affected area twice daily (morning and evening) or as directed by clinician.
Children ≥12 years of age: apply a thin film of Duac gel to the cleansed affected areas once daily in the evening or as directed by clinician.
Bacterial Vaginosis
Treatment in Nonpregnant Postmenarchal Females
IntravaginalClindesse vaginal cream: One applicatorful (single dose).
Vaginal suppositories: 1 suppository daily (preferably at bedtime) for 3 days.
Adults
Acne Vulgaris
Maintenance therapy needed to prevent recurrence.
Treatment with Single-entity Clindamycin Preparations
TopicalApply a thin film of gel, lotion, or solution to the cleansed affected area twice daily.
Treatment with Clindamycin and Benzoyl Peroxide Combination Preparations
TopicalBenzaClin gel: apply a thin film to the cleansed affected area twice daily (morning and evening) or as directed by clinician.
Duac gel: apply a thin film to the cleansed affected areas once daily in the evening or as directed by clinician.
Bacterial Vaginosis
Treatment in Nonpregnant Women
IntravaginalCleocin vaginal cream: 1 applicatorful once daily (preferably at bedtime) for 3 or 7 consecutive days. CDC recommends a 7-day regimen.
Clindesse vaginal cream: One applicatorful (single dose).
Vaginal suppositories: 1 suppository once daily (preferably at bedtime) for 3 consecutive days.
Treatment in Pregnant Women
IntravaginalVaginal cream: 1 applicatorful once daily (preferably at bedtime) for 7 consecutive days.
Cautions for Clindamycin Phosphate (Topical)
Contraindications
-
Hypersensitivity to clindamycin, lincomycin, or any ingredient in the formulations.
-
History of regional enteritis, ulcerative colitis, or antibiotic-associated colitis.
Warnings/Precautions
Warnings
Clostridium difficile-associated Diarrhea
Treatment with anti-infectives may permit overgrowth of Clostridium difficile. C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) has been reported with use of topical or systemic clindamycin. Consider CDAD if diarrhea develops during or following topical or intravaginal clindamycin therapy and manage accordingly.
Some mild cases of CDAD may respond to discontinuance alone. Manage moderate to severe cases with fluid, electrolyte, and protein supplementation; appropriate anti-infective therapy (e.g., oral metronidazole or vancomycin) recommended if colitis is severe.
Sensitivity Reactions
Contact dermatitis has been reported following use of topical clindamycin.
Consider possibility that patients who become sensitized to topical clindamycin also may be sensitive to systemic clindamycin or lincomycin.
Urticaria, rash, application-site pain, and pruritus occur rarely.
Use topical gel, lotion, and solution with caution in atopic individuals.
General Precautions
Superinfection
Possible emergence and overgrowth of nonsusceptible bacteria or fungi.
Vaginal and nonvaginal candidiasis (moniliasis) and vaginitis have occurred with intravaginal clindamycin.
Gram-negative folliculitis has been reported rarely following topical clindamycin.
If suprainfection or superinfection occurs, discontinue the drug and institute appropriate therapy.
Vaginal Intercourse and Use of Vaginal Products
Patients receiving intravaginal clindamycin should not engage in vaginal intercourse and should refrain from use of vaginal products (e.g., douches, tampons) during the entire course of therapy.
Efficacy of clindamycin could be reduced (e.g., by dislodgment and/or dilution, by increased vaginal pH secondary to deposition of semen).
Latex or rubber products (e.g., condoms, vaginal contraceptive diaphragms) are weakened by oleaginous bases (e.g., mineral oil) in vaginal cream and suppositories and may not be effective as contraceptives and/or microbial barriers if used within 72 hours following intravaginal Cleocin or within 5 days following intravaginal Clindesse.
Systemic Adverse Effects
Clindamycin is absorbed following topical or intravaginal application, and can be absorbed in sufficient amounts to produce systemic effects.
Administration Precautions
Vaginal cream may cause ocular burning and irritation; avoid contact with the eyes, and irrigate eyes with copious amounts of cool water if contact occurs.
Topical solution contains alcohol which can burn and irritate sensitive surfaces (e.g., eyes, abraded skin, mucous membranes); bathe surfaces with copious amounts of cool water if contact occurs.
Topical solution has an unpleasant taste; use caution when applying around the mouth.
Specific Populations
Pregnancy
Category B (topical and vaginal single-entity clindamycin preparations).
Category C (topical combination preparations containing clindamycin and benzoyl peroxide).
CDC states clindamycin vaginal preparations should be used only during the first half of pregnancy.
Lactation
Distributed into milk following systemic administration; not known whether clindamycin is distributed into milk following topical or intravaginal administration.
Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy of single-entity topical gel, lotion, or solution containing clindamycin not established in children <12 years of age.
Safety and efficacy of topical gels containing clindamycin in combination with benzoyl peroxide not established in children <12 years of age.
Safety and efficacy of vaginal cream (Cleocin) not established in children <16 years of age.
Safety and efficacy of vaginal suppositories (Cleocin) and vaginal cream (Clindesse) established in postmenarchal females based on extrapolation of data from adult women; safety and efficacy not established in premenarchal females.
Geriatric Use
Insufficient experience with vaginal or topical clindamycin preparations in patients ≥65 years of age to determine whether geriatric patients respond differently than younger patients.
Common Adverse Effects
Topical application to the skin: burning, pruritus, dryness, erythema, oily skin, peeling.
Intravaginal administration: vaginal candidiasis, vulvovaginitis, vulvovaginal disorder, trichomonal vaginitis, vaginal pain, body moniliasis, fungal infection.
Drug Interactions
Because clindamycin can be absorbed systemically following topical application to the skin or following intravaginal administration, the possibility that drug interactions could occur with these routes should be considered.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol (e.g., in astringents, after-shave lotions) |
Possible cumulative irritant or drying effect |
|
|
Erythromycin |
In vitro evidence of antagonism |
Do not use concomitantly |
|
Neuromuscular blocking agents (e.g., ether, tubocurarine, pancuronium) |
Systemically absorbed clindamycin after intravaginal administration has potential for enhanced neuromuscular blocking action |
Use intravaginal clindamycin with caution in patients receiving neuromuscular blocking agents; observe for neuromuscular blockade prolongation |
|
Salicylic acid |
Possible cumulative irritant effect |
Use with caution |
|
Soap (abrasive, medicated) |
Possible cumulative irritant or drying effect |
|
|
Sulfur |
Possible cumulative irritant effect |
Use with caution |
|
Tretinoin |
Possible cumulative irritant effect |
Use with caution |
Clindamycin Phosphate (Topical) Pharmacokinetics
Absorption
Bioavailability
Absorbed systemically following topical or intravaginal administration.
Approximately 5% of an intravaginal dose of clindamycin 2% vaginal cream (Cleocin) is absorbed systemically; peak serum concentrations attained approximately 14 hours after the intravaginal dose.
Systemic absorption following intravaginal administration of Clindesse vaginal cream is reported to be lower than that following administration of Cleocin vaginal cream.
Following intravaginal administration of vaginal suppository (100-mg vaginal suppository once daily for 3 days), almost 30% of the dose is absorbed systemically.
Distribution
Not fully characterized following intravaginal administration.
Elimination
Not fully characterized following intravaginal administration.
Half-life
1.5–2.6 hours following intravaginal administration of vaginal cream (Cleocin).
11 hours (range: 4–35 hours) following intravaginal administration of vaginal suppository.
Stability
Storage
Topical
Gel, Lotion, or Solution
Tight container at 20–25°C; do not freeze.
Clindamycin and Benzoyl Peroxide Gel Combinations
BenzaClin: room temperature ≤25°C before or after dispensing. Stable for 3 months following reconstitution of clindamycin powder and mixture with benzoyl peroxide gel.
Duac: 2–8°C before dispensing. Stable at room temperature ≤25°C for 60 days after dispensing; do not freeze.
Intravaginal
Cream
Cleocin: 20–25°C; do not freeze.
Clindesse: 25°C (may be exposed to 15–30°C). Avoid temperatures >30°C.
Suppositories
25°C (may be exposed to 15–30°C). Avoid temperatures >30°C and avoid high humidity.
Actions and Spectrum
-
May be bactericidal or bacteriostatic in action, depending on concentration attained at site of infection and susceptibility of the infecting organism.
-
Inhibits protein synthesis in susceptible organisms by reversible binding 50S ribosomal subunits.
-
Clindamycin phosphate is inactive until hydrolyzed in vivo to free clindamycin.
-
Exact mechanisms of action in treatment of acne vulgaris not fully elucidated; antibacterial activity may result in reduction of acne vulgaris lesions, but other mechanisms also appear to be involved.
-
Inhibits skin surface growth of susceptible organisms (primarily Propionibacterium acnes), reduces formation and concentration of comedogenic (and possibly inflammatory lesion-inducing) free fatty acid in sebum.
-
In vitro, inhibits leukocyte chemotaxis; if this occurs in vivo, may be another mechanism for suppression of inflammatory acne vulgaris lesions.
-
In vitro spectrum of activity includes many gram-positive aerobic bacteria, some gram-negative aerobic bacteria, and many gram-positive and -negative anaerobic bacteria. Inactive against fungi and viruses.
-
Clindamycin-resistant P. acnes have been reported.
-
Complete cross-resistance occurs between clindamycin and lincomycin; partial cross-resistance occurs between clindamycin, lincomycin, and erythromycin.
Advice to Patients
-
Importance of discontinuing use and notifying clinician if GI symptoms (e.g., diarrhea) occur.
-
Importance of notifying clinician if local reactions or any other adverse reactions occur.
-
Instruct patients regarding vaginal applicator use, and provide a copy of the manufacturer’s instructions.
-
Advise patients using topical gels containing clindamycin and benzyl peroxide that these preparations may bleach hair or colored fabric.
-
Advise women using intravaginal cream or suppositories not to engage in vaginal intercourse and to refrain from use of vaginal products (e.g., douches or tampons) during the entire course of therapy.
-
Advise women using Cleocin intravaginal cream or suppositories not to rely on latex or rubber products (e.g., condoms, vaginal contraceptive diaphragms) as contraceptives and/or microbial barriers if used within 72 hours following administration of the vaginal cream or suppository.
-
Advise women using Clindesse intravaginal cream not to rely on latex or rubber products (e.g., condoms, vaginal contraceptive diaphragms) as contraceptives and/or microbial barriers if used within 5 days following administration of the vaginal cream.
-
If using topical skin preparations, importance of avoiding contact with eyes, abraded skin, or mucous membranes; need to bathe area with copious amounts of cool water if contact occurs.
-
If using vaginal cream, importance of avoiding contact of the cream with eyes; need to irrigate eyes with copious amounts of cool water if contact occurs.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Topical |
Gel |
1% (of clindamycin)* |
Cleocin T |
Pfizer |
|
Clindagel |
Galderma |
|||
|
Lotion |
1% (of clindamycin) |
Cleocin T |
Pfizer |
|
|
Pledgets (saturated with solution) |
1% (of clindamycin)* |
Cleocin T Pledgets |
Pfizer |
|
|
Clindamycin Phosphate Pledgets |
||||
|
Clindets Pledgets |
Stiefel |
|||
|
Solution |
1% (of clindamycin)* |
Cleocin T 1% |
Pfizer |
|
|
Clinda-Derm |
Paddock |
|||
|
Clindamycin Phosphate Topical Solution |
||||
|
Vaginal |
Cream |
2% (of clindamycin) |
Cleocin (with 7 disposable vaginal applicators) |
Pfizer |
|
Clindesse (available in prefilled, disposable applicators) |
Ther-Rx |
|||
|
Suppositories |
100 mg (of clindamycin) |
Cleocin Vaginal Ovules (with vaginal applicator) |
Pfizer |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Topical |
For gel |
300 mg (of clindamycin phosphate to prepare a clindamycin 1% gel) with Benzoyl Peroxide 5% |
BenzaClin (with 1 or 2 vials containing clindamycin phosphate [300 mg of clindamycin] powder and container of benzoyl peroxide gel 5%) |
Dermik |
|
Gel |
1% (of clindamycin) with Benzoyl Peroxide 5% |
Duac |
Stiefel |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about clindamycin topical
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (232)
- Side effects
- Dosage information
- During pregnancy
- Drug class: topical acne agents
- Breastfeeding
Patient resources
Professional resources
- Clindacin Foam prescribing information
- Clindamycin Foam (FDA)
- Clindamycin Gel (FDA)
- Clindamycin Lotion (FDA)
- Clindamycin Pledget (FDA)
Other brands
Clindagel, Cleocin Vaginal, Clindamax, Xaciato, ... +4 more