Clindamycin Phosphate (Topical) (Monograph)
Brand names: Cleocin, Cleocin T, Clinda-Derm, Clindagel, Clindesse, Clindets
Drug class: Antibacterials
Introduction
Antibacterial; broad-spectrum antibiotic derived from lincomycin.5 6 7 100
Uses for Clindamycin Phosphate (Topical)
Acne Vulgaris
Treatment of inflammatory acne vulgaris; used alone or in conjunction with benzoyl peroxide.1 178 179 186 187
Generally effective for treatment of mild to moderate inflammatory acne.a 186 187
May induce bacterial resistance when used as monotherapy;186 187 resistance associated with decreased clinical efficacy.186
Particularly useful when used in combination with benzoyl peroxide or topical retinoids;186 187 reduction in total lesion count of 50–70% reported when combination therapy used.186
Bacterial Vaginosis
Treatment of bacterial vaginosis (formerly called Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis).100 101 102 103 104 105 107 109 114 115 120 131 132 133 145 176 177 180
CDC recommends treatment of bacterial vaginosis in all symptomatic women (including pregnant women).101 In addition, asymptomatic pregnant women at high risk for complications of pregnancy should be screened (preferably at the first prenatal visit) and treatment initiated if needed.101
Treatment recommendations for bacterial vaginosis in HIV-infected women are the same as those for women without HIV infection.101
Regimens of choice in nonpregnant women are a 7-day regimen of oral metronidazole; a 5-day regimen of intravaginal metronidazole gel; or a 7-day regimen of intravaginal clindamycin cream;101 alternative regimens are a 7-day regimen of oral clindamycin or 3-day regimen of intravaginal clindamycin suppositories.101 The preferred regimens for pregnant women are a 7-day regimen of oral metronidazole or oral clindamycin.101
Regardless of regimen used, relapse or recurrence is common;101 102 114 115 132 136 an alternative regimen (e.g., oral therapy when topical was used initially) may be used in such situations.101 120
Routine treatment of asymptomatic male sexual contacts of women who have relapsing or recurrent bacterial vaginosis not recommended.101
Clindamycin Phosphate (Topical) Dosage and Administration
Administration
Administer topically to the skin1 178 179 or intravaginally100 176 180 in appropriate formulations.
Topical skin preparations are for external use only and should not be used orally, intravaginally, or near or in eyes or mucous membranes.178 179
Intravaginal preparations are for intravaginal administration only and should not be used orally, topically on the skin, or near or in eyes.a
Topical Administration
Apply topically to the skin as a gel, lotion, or solution containing clindamycin 1%1 or as a gel containing clindamycin 1% in combination with benzoyl peroxide 5%.178 179 Apply to all areas of skin prone to acne.186
Do not use near eyes, nose, mouth, or other mucous membranes.178 179
Shake lotion well immediately prior to use.1
Remove solution-containing pledgets from their foil immediately before use; do not use if seal is broken.1 Use each pledget only once and then discard; may use more than 1 pledget for each application if needed to cover the affected area.1
Reconstitution
BenzaClin
Prepare BenzaClin topical gel containing clindamycin and benzoyl peroxide at the time of dispensing.179
Reconstitute vial containing clindamycin powder by adding 5 mL of purified water and shaking immediately to completely dissolve the drug; if needed, add additional purified water to bring level up to the mark on the vial.179
Add the reconstituted clindamycin solution to the benzyl peroxide gel provided by the manufacturer; stir until homogenous in appearance (1 to 1.5 minutes).179
Duac
Duac topical gel containing clindamycin and benzoyl peroxide does not need reconstitution and is used as provided by the manufacturer.178
Intravaginal Topical Administration
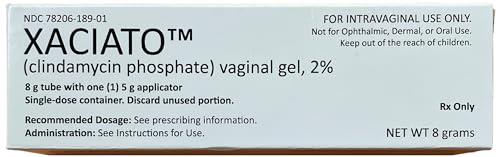
Administer intravaginally as a cream containing clindamycin 2% or as 100-mg vaginal suppositories.100 101 103 104 105 107 114 131 145 180
Dosage
Pediatric Patients
Acne Vulgaris
Maintenance therapy needed to prevent recurrence.186
Single-entity Clindamycin Preparations
TopicalChildren ≥12 years of age: apply a thin film of gel, lotion, or solution to the cleansed affected area twice daily.1
Clindamycin and Benzoyl Peroxide Combination Preparations
TopicalChildren ≥12 years of age: apply a thin film of BenzaClin gel to the cleansed affected area twice daily (morning and evening) or as directed by clinician.179
Children ≥12 years of age: apply a thin film of Duac gel to the cleansed affected areas once daily in the evening or as directed by clinician.178
Bacterial Vaginosis
Treatment in Nonpregnant Postmenarchal Females
IntravaginalClindesse vaginal cream: One applicatorful (single dose).180
Vaginal suppositories: 1 suppository daily (preferably at bedtime) for 3 days.176
Adults
Acne Vulgaris
Maintenance therapy needed to prevent recurrence.186
Treatment with Single-entity Clindamycin Preparations
TopicalApply a thin film of gel, lotion, or solution to the cleansed affected area twice daily.1
Treatment with Clindamycin and Benzoyl Peroxide Combination Preparations
TopicalBenzaClin gel: apply a thin film to the cleansed affected area twice daily (morning and evening) or as directed by clinician.179
Duac gel: apply a thin film to the cleansed affected areas once daily in the evening or as directed by clinician.178
Bacterial Vaginosis
Treatment in Nonpregnant Women
IntravaginalCleocin vaginal cream: 1 applicatorful once daily (preferably at bedtime) for 3 or 7 consecutive days.100 101 104 105 107 CDC recommends a 7-day regimen.101
Clindesse vaginal cream: One applicatorful (single dose).180
Vaginal suppositories: 1 suppository once daily (preferably at bedtime) for 3 consecutive days.101 176
Treatment in Pregnant Women
IntravaginalVaginal cream: 1 applicatorful once daily (preferably at bedtime) for 7 consecutive days.163 164
Cautions for Clindamycin Phosphate (Topical)
Contraindications
-
Hypersensitivity to clindamycin, lincomycin, or any ingredient in the formulations.1 100 178 179
-
History of regional enteritis, ulcerative colitis, or antibiotic-associated colitis.1 100 176 178 179
Warnings/Precautions
Warnings
Clostridium difficile-associated Diarrhea
Treatment with anti-infectives may permit overgrowth of Clostridium difficile.1 100 176 178 179 180 C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) has been reported with use of topical or systemic clindamycin.1 100 176 178 179 180 Consider CDAD if diarrhea develops during or following topical or intravaginal clindamycin therapy and manage accordingly.1 100 176 178 179 180 181 182 183 184 185
Some mild cases of CDAD may respond to discontinuance alone.1 100 176 178 179 180 181 182 183 184 185 Manage moderate to severe cases with fluid, electrolyte, and protein supplementation; appropriate anti-infective therapy (e.g., oral metronidazole or vancomycin) recommended if colitis is severe.1 100 176 178 179 180 181 182 183 184 185
Sensitivity Reactions
Contact dermatitis has been reported following use of topical clindamycin.a
Consider possibility that patients who become sensitized to topical clindamycin also may be sensitive to systemic clindamycin or lincomycin.a
Urticaria, rash, application-site pain, and pruritus occur rarely.100 145 176
Use topical gel, lotion, and solution with caution in atopic individuals.1
General Precautions
Superinfection
Possible emergence and overgrowth of nonsusceptible bacteria or fungi.176 178 179
Vaginal and nonvaginal candidiasis (moniliasis) and vaginitis have occurred with intravaginal clindamycin.176
Gram-negative folliculitis has been reported rarely following topical clindamycin.a
If suprainfection or superinfection occurs, discontinue the drug and institute appropriate therapy.a 178 179
Vaginal Intercourse and Use of Vaginal Products
Patients receiving intravaginal clindamycin should not engage in vaginal intercourse and should refrain from use of vaginal products (e.g., douches, tampons) during the entire course of therapy.100 103 105 107 131 176
Efficacy of clindamycin could be reduced (e.g., by dislodgment and/or dilution, by increased vaginal pH secondary to deposition of semen).120 147
Latex or rubber products (e.g., condoms, vaginal contraceptive diaphragms) are weakened by oleaginous bases (e.g., mineral oil) in vaginal cream and suppositories and may not be effective as contraceptives and/or microbial barriers if used within 72 hours following intravaginal Cleocin or within 5 days following intravaginal Clindesse.100 176 180
Systemic Adverse Effects
Clindamycin is absorbed following topical or intravaginal application,1 100 176 178 179 and can be absorbed in sufficient amounts to produce systemic effects.1 100 176
Administration Precautions
Vaginal cream may cause ocular burning and irritation; avoid contact with the eyes, and irrigate eyes with copious amounts of cool water if contact occurs.100 150
Topical solution contains alcohol which can burn and irritate sensitive surfaces (e.g., eyes, abraded skin, mucous membranes); bathe surfaces with copious amounts of cool water if contact occurs.1
Topical solution has an unpleasant taste; use caution when applying around the mouth.a
Specific Populations
Pregnancy
Category B (topical and vaginal single-entity clindamycin preparations).a 1 100 180
Category C (topical combination preparations containing clindamycin and benzoyl peroxide).178 179
CDC states clindamycin vaginal preparations should be used only during the first half of pregnancy.101
Lactation
Distributed into milk following systemic administration; not known whether clindamycin is distributed into milk following topical or intravaginal administration.1 100
Discontinue nursing or the drug.1 100 178 179
Pediatric Use
Safety and efficacy of single-entity topical gel, lotion, or solution containing clindamycin not established in children <12 years of age.1
Safety and efficacy of topical gels containing clindamycin in combination with benzoyl peroxide not established in children <12 years of age.178 179
Safety and efficacy of vaginal cream (Cleocin) not established in children <16 years of age.100 150
Safety and efficacy of vaginal suppositories (Cleocin) and vaginal cream (Clindesse) established in postmenarchal females based on extrapolation of data from adult women; safety and efficacy not established in premenarchal females.176 180
Geriatric Use
Insufficient experience with vaginal or topical clindamycin preparations in patients ≥65 years of age to determine whether geriatric patients respond differently than younger patients.1 100 176 180
Common Adverse Effects
Topical application to the skin: burning, pruritus, dryness, erythema, oily skin, peeling.1 178 179
Intravaginal administration: vaginal candidiasis, vulvovaginitis, vulvovaginal disorder, trichomonal vaginitis, vaginal pain, body moniliasis, fungal infection.100 176 180
Drug Interactions
Because clindamycin can be absorbed systemically following topical application to the skin or following intravaginal administration, the possibility that drug interactions could occur with these routes should be considered.100 108
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol (e.g., in astringents, after-shave lotions) |
Possible cumulative irritant or drying effecta |
|
|
Erythromycin |
||
|
Neuromuscular blocking agents (e.g., ether, tubocurarine, pancuronium) |
Systemically absorbed clindamycin after intravaginal administration has potential for enhanced neuromuscular blocking action100 125 126 176 |
Use intravaginal clindamycin with caution in patients receiving neuromuscular blocking agents; observe for neuromuscular blockade prolongation 100 125 126 176 |
|
Salicylic acid |
Possible cumulative irritant effecta |
Use with cautiona |
|
Soap (abrasive, medicated) |
Possible cumulative irritant or drying effecta |
|
|
Sulfur |
Possible cumulative irritant effecta |
Use with cautiona |
|
Tretinoin |
Possible cumulative irritant effecta |
Use with cautiona |
Clindamycin Phosphate (Topical) Pharmacokinetics
Absorption
Bioavailability
Absorbed systemically following topical or intravaginal administration.1 100 108 176
Approximately 5% of an intravaginal dose of clindamycin 2% vaginal cream (Cleocin) is absorbed systemically; peak serum concentrations attained approximately 14 hours after the intravaginal dose.100
Systemic absorption following intravaginal administration of Clindesse vaginal cream is reported to be lower than that following administration of Cleocin vaginal cream.180
Following intravaginal administration of vaginal suppository (100-mg vaginal suppository once daily for 3 days), almost 30% of the dose is absorbed systemically.176
Distribution
Not fully characterized following intravaginal administration.150
Elimination
Not fully characterized following intravaginal administration.150
Half-life
1.5–2.6 hours following intravaginal administration of vaginal cream (Cleocin).100
11 hours (range: 4–35 hours) following intravaginal administration of vaginal suppository.176
Stability
Storage
Topical
Gel, Lotion, or Solution
Tight container at 20–25°C; do not freeze.1
Clindamycin and Benzoyl Peroxide Gel Combinations
BenzaClin: room temperature ≤25°C before or after dispensing.179 Stable for 3 months following reconstitution of clindamycin powder and mixture with benzoyl peroxide gel.179
Duac: 2–8°C before dispensing.178 Stable at room temperature ≤25°C for 60 days after dispensing; do not freeze.178
Intravaginal
Cream
Cleocin: 20–25°C; do not freeze.1
Clindesse: 25°C (may be exposed to 15–30°C).180 Avoid temperatures >30°C.180
Suppositories
25°C (may be exposed to 15–30°C).176 Avoid temperatures >30°C and avoid high humidity.176
Actions and Spectrum
-
May be bactericidal or bacteriostatic in action, depending on concentration attained at site of infection and susceptibility of the infecting organism.a
-
Inhibits protein synthesis in susceptible organisms by reversible binding 50S ribosomal subunits.a
-
Clindamycin phosphate is inactive until hydrolyzed in vivo to free clindamycin.1
-
Exact mechanisms of action in treatment of acne vulgaris not fully elucidated; antibacterial activity may result in reduction of acne vulgaris lesions, but other mechanisms also appear to be involved.a
-
Inhibits skin surface growth of susceptible organisms (primarily Propionibacterium acnes), reduces formation and concentration of comedogenic (and possibly inflammatory lesion-inducing) free fatty acid in sebum.a
-
In vitro, inhibits leukocyte chemotaxis; if this occurs in vivo, may be another mechanism for suppression of inflammatory acne vulgaris lesions.a
-
In vitro spectrum of activity includes many gram-positive aerobic bacteria, some gram-negative aerobic bacteria, and many gram-positive and -negative anaerobic bacteria.5 6 10 Inactive against fungi and viruses.
-
Clindamycin-resistant P. acnes have been reported.178
-
Complete cross-resistance occurs between clindamycin and lincomycin; partial cross-resistance occurs between clindamycin, lincomycin, and erythromycin.a
Advice to Patients
-
Importance of discontinuing use and notifying clinician if GI symptoms (e.g., diarrhea) occur.1 100 178 179
-
Importance of notifying clinician if local reactions or any other adverse reactions occur.178 179
-
Instruct patients regarding vaginal applicator use, and provide a copy of the manufacturer’s instructions.100
-
Advise patients using topical gels containing clindamycin and benzyl peroxide that these preparations may bleach hair or colored fabric.178 179
-
Advise women using intravaginal cream or suppositories not to engage in vaginal intercourse and to refrain from use of vaginal products (e.g., douches or tampons) during the entire course of therapy.100 103 105 107 131 176 180
-
Advise women using Cleocin intravaginal cream or suppositories not to rely on latex or rubber products (e.g., condoms, vaginal contraceptive diaphragms) as contraceptives and/or microbial barriers if used within 72 hours following administration of the vaginal cream or suppository.100 176
-
Advise women using Clindesse intravaginal cream not to rely on latex or rubber products (e.g., condoms, vaginal contraceptive diaphragms) as contraceptives and/or microbial barriers if used within 5 days following administration of the vaginal cream.180
-
If using topical skin preparations, importance of avoiding contact with eyes, abraded skin, or mucous membranes; need to bathe area with copious amounts of cool water if contact occurs.1 178 179
-
If using vaginal cream, importance of avoiding contact of the cream with eyes; need to irrigate eyes with copious amounts of cool water if contact occurs.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Topical |
Gel |
1% (of clindamycin)* |
Cleocin T |
Pfizer |
|
Clindagel |
Galderma |
|||
|
Lotion |
1% (of clindamycin) |
Cleocin T |
Pfizer |
|
|
Pledgets (saturated with solution) |
1% (of clindamycin)* |
Cleocin T Pledgets |
Pfizer |
|
|
Clindamycin Phosphate Pledgets |
||||
|
Clindets Pledgets |
Stiefel |
|||
|
Solution |
1% (of clindamycin)* |
Cleocin T 1% |
Pfizer |
|
|
Clinda-Derm |
Paddock |
|||
|
Clindamycin Phosphate Topical Solution |
||||
|
Vaginal |
Cream |
2% (of clindamycin) |
Cleocin (with 7 disposable vaginal applicators) |
Pfizer |
|
Clindesse (available in prefilled, disposable applicators) |
Ther-Rx |
|||
|
Suppositories |
100 mg (of clindamycin) |
Cleocin Vaginal Ovules (with vaginal applicator) |
Pfizer |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Topical |
For gel |
300 mg (of clindamycin phosphate to prepare a clindamycin 1% gel) with Benzoyl Peroxide 5% |
BenzaClin (with 1 or 2 vials containing clindamycin phosphate [300 mg of clindamycin] powder and container of benzoyl peroxide gel 5%) |
Dermik |
|
Gel |
1% (of clindamycin) with Benzoyl Peroxide 5% |
Duac |
Stiefel |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
Only references cited for selected revisions after 1984 are available electronically.
1. Pharmacia & Upjohn. Cleocin T (clindamycin phosphate topical solution, topical gel, and topical lotion) prescribing information. New York, NY; 2005 Nov.
5. Kucers A, Bennett N. The use of antibiotics. 3rd ed. Philadelphia: JB Lippincott; 1979:470-95.
6. Kagan BM. Antimicrobial therapy. 3rd ed. Philadelphia: WB Saunders; 1980:97-116.
7. Grenzach HS. Antibiotics and chemotherapy. Vol 25. New York: S Karger; 1978:204-9.
10. Sutter VL. In vitro susceptibility of anaerobes: comparison of clindamycin and other antimicrobial agents. J Infect Dis. 1977; 135:7-12.
13. Wang WL, Everett ED, Johnson M et al. Susceptibility of Propionibacterium acnes to seventeen antibiotics. Antimicrob Agents Chemother. 1977; 11:171-3. https://pubmed.ncbi.nlm.nih.gov/836012
14. Rosenthal SL, Freundlich LF, Gilardi GL et al. In vitro antibiotic sensitivity of Moraxella species. Chemotherapy. 1978; 24:360-3. https://pubmed.ncbi.nlm.nih.gov/699676
22. Crawford WW, Crawford IP, Stoughton RB et al. Laboratory induction and clinical occurrence of combined clindamycin and erythromycin resistance in Corynebacterium acnes . J Invest Derm. 1979; 72:187-90. https://pubmed.ncbi.nlm.nih.gov/429800
100. Pharmacia & Upjohn Company. Cleocin (clindamycin phosphate vaginal cream) prescribing information. New York, NY; 2005 Nov.
101. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006; 55(RR-11):1-95.
102. Hillier S, Holmes KK. Bacterial vaginosis. In: Holmes KK, Mardh PA, Sparling PF et al, eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill; 1990:547-59.
103. Livengood CH III, Thomason JL, Hill GB. Bacterial vaginosis: treatment with topical intravaginal clindamycin phosphate. Obstet Gynecol. 1990; 76:118-23. https://pubmed.ncbi.nlm.nih.gov/2193261
104. Hillier S, Krohn MA, Watts H et al. Microbiologic efficacy of intravaginal clindamycin cream for the treatment of bacterial vaginosis. Obstet Gynecol. 1990; 76:407-13. https://pubmed.ncbi.nlm.nih.gov/2381617
105. Schmitt C, Sobel JD, Meriwether C. Bacterial vaginosis: treatment with clindamycin cream versus oral metronidazole. Obstet Gynecol. 1992; 79:1020-3. https://pubmed.ncbi.nlm.nih.gov/1579299
106. Sobel JD, Schmitt C, Meriwether C. Long-term follow-up of patients with bacterial vaginosis treated with oral metronidazole and topical clindamycin. J Infect Dis. 1993; 167:783-4. https://pubmed.ncbi.nlm.nih.gov/8440952
107. Andres FJ, Parker R, Hosein I et al. Clindamycin vaginal cream versus oral metronidazole in the treatment of bacterial vaginosis: a prospective double-blind clinical trial. South Med J. 1992; 85:1077-80. https://pubmed.ncbi.nlm.nih.gov/1439943
108. Borin MT. Systemic absorption of clindamycin following intravaginal application of clindamycin phosphate 1% cream. J Clin Pharmacol. 1990; 30:33-8. https://pubmed.ncbi.nlm.nih.gov/2303578
109. Anon. Drugs for sexually transmitted infections. Treat Guidel Med Lett. 2004; 2:67-74. https://pubmed.ncbi.nlm.nih.gov/15529116
110. Anon. Topical treatment for bacterial vaginosis. Med Lett Drugs Ther. 1992; 34:109. https://pubmed.ncbi.nlm.nih.gov/1435507
111. Lugo-Miro VI, Green M, Mazur L. Comparison of different metronidazole therapeutic regimens for bacterial vaginosis: a meta-analysis. JAMA. 1992; 268:92-5. https://pubmed.ncbi.nlm.nih.gov/1535108
112. Mardh PA. The vaginal ecosystem. Am J Obstet Gynecol. 1991; 165:1163-8. https://pubmed.ncbi.nlm.nih.gov/1951571
113. Thomason JL, Gelbart SM, Anderson RJ et al. Statistical evaluation of diagnostic criteria for bacterial vaginosis. Am J Obstet Gynecol. 1990; 162:155-60. https://pubmed.ncbi.nlm.nih.gov/1689107
114. Depew CC. Manufacturer letter regarding the use of Cleocin vaginal cream for bacterial vaginosis. Kalamazoo, MI: The Upjohn Company; 1992 Nov 25.
115. Thomason JL, Gelbart SM, Scaglione NJ. Bacterial vaginosis: current review with indications for asymptomatic therapy. Am J Obstet Gynecol. 1991; 165:1210-7. https://pubmed.ncbi.nlm.nih.gov/1951577
117. McCarthy LR, Mickelsen PA, Smith EG. Antibiotic susceptibility of Haemophilus vaginalis (Corynebacterium vaginale) to 21 antibiotics. Antimicrob Agents Chemother. 1979; 16:186-9. https://pubmed.ncbi.nlm.nih.gov/314776
118. Spiegel CA, Eschenbach DA, Amsel R et al. Curved anaerobic bacteria in bacterial (nonspecific) vaginosis and their response to antimicrobial therapy. J Infect Dis. 1983; 148:817-22. https://pubmed.ncbi.nlm.nih.gov/6631073
119. Larsson PG, Platz-Christensen JJ, Thejls H et al. Incidence of pelvic inflammatory disease after first-trimester legal abortion in women with bacterial vaginosis after treatment with metronidazole: a double-blind, randomized study. Am J Obstet Gynecol. 1992; 166:100-3. https://pubmed.ncbi.nlm.nih.gov/1733176
120. Centers for Disease Control and Prevention, Atlanta, GA: Personal communication.
121. American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin: Vaginitis. Number 72. Washington, DC: American College of Obstetricians and Gynecologists; 2006 May.
122. Goldstein EJC, Citron DM, Cherubin CE et al. Comparative susceptibility of the Bacteroides fragilis group species and other anaerobic bacteria to meropenem, imipenem, piperacillin, cefoxitin, ampicillin/sulbactam, clindamycin, and metronidazole. J Antimicrob Chemother. 1993; 31:363-72. https://pubmed.ncbi.nlm.nih.gov/8486570
123. Spiegel CA. Susceptibility of Mobiluncus species to 23 antimicrobial agents and 15 other compounds. Antimicrob Agents Chemother. 1987; 31:249-52. https://pubmed.ncbi.nlm.nih.gov/3566250
124. Ohm-Smith MJ, Sweet RL, Hadley WK. In vitro activity of cefbuperazone and other antimicrobial agents against isolates from the female genital tract. Antimicrob Agents Chemother. 1985; 27:958-60. https://pubmed.ncbi.nlm.nih.gov/4026268
125. Nondepolarizing muscle relaxants/lincosamides. In: Tatro DS, Olin BR, Hebel SK, eds. Drug interaction facts. St. Louis: JB Lippincott Co; 1991(Jan):530.
126. Clindamycin (Cleocin) interactions. In: Hansten PD, Horn JR. Drug interactions & updates. Vancouver, WA: Applied Therapeutics; 1993(Jul):217.
127. Hill GB. The microbiology of bacterial vaginosis. Am J Obstet Gynecol. 1993; 169:450-4. https://pubmed.ncbi.nlm.nih.gov/8357043
128. Greaves WL, Chungafung J, Morris B et al. Clindamycin versus metronidazole in the treatment of bacterial vaginosis. Obstet Gynecol. 1988; 72:799-802. https://pubmed.ncbi.nlm.nih.gov/3050654
129. Bignardi GE. Clindamycin versus metronidazole in the treatment of bacterial vaginosis. Obstet Gynecol. 1989; 74:281. https://pubmed.ncbi.nlm.nih.gov/2748067
130. Greaves WL. Clindamycin versus metronidazole in the treatment of bacterial vaginosis. Obstet Gynecol. 1989; 74:281-2. https://pubmed.ncbi.nlm.nih.gov/2748067
131. Higuera F, Hidalgo H, Sanchez CJ et al. Bacterial vaginosis: a comparative, double-blind study of clindamycin vaginal cream versus oral metronidazole. Curr Ther Res. 1993; 54:98-110.
132. Thomason JL, Gelbart SM, Broekhuizen FF. Advances in the understanding of bacterial vaginosis. J Reprod Med. 1989; 34(Suppl):581-7. https://pubmed.ncbi.nlm.nih.gov/2677362
133. Sweet RL. New approaches for the treatment of bacterial vaginosis. Am J Obstet Gynecol. 1993; 169:479-82. https://pubmed.ncbi.nlm.nih.gov/8357050
134. Waites KB, Duffy LB, Schmid T et al. In vitro susceptibilities of Mycoplasma pneumoniae, Mycoplasma hominis, and Ureaplasma urealyticum to sparfloxacin and PD 127391. Antimicrob Agents Chemother. 1991; 35:1181-5. https://pubmed.ncbi.nlm.nih.gov/1929260
135. Balows A, Hausler WJ, Herrmann KL et al, eds. Manual of clinical microbiology. 5th ed. Washington, DC: American Society for Microbiology; 1991:481,484.
136. Lossick JG. Treatment of sexually transmitted vaginosis/vaginitis. Clin Infect Dis. 1990; 12(Suppl 6):S665-81.
137. Amsel R, Totten PA, Spiegel CA et al. Nonspecific vaginitis: diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983; 74:14-22. https://pubmed.ncbi.nlm.nih.gov/6600371
138. 3M Pharmaceuticals. MetroGel-Vaginal (metronidazole vaginal gel) prescribing information. Northridge, CA; 1997 May.
139. Hillier SL, Lipinski C, Briselden AM et al. Efficacy of intravaginal 0.75% metronidazole gel for the treatment of bacterial vaginosis. Obstet Gynecol. 1993; 81:963-7. https://pubmed.ncbi.nlm.nih.gov/8497364
140. Livengood CH 3rd, McGregor JA, Soper DE et al. Bacterial vaginosis: efficacy and safety of intravaginal metronidazole treatment. Am J Obstet Gynecol. 1994;170:759-64.
141. Ahmed-Jushuf IH, Shahmanesh M, Arya OP. The treatment of bacterial vaginosis with a 3 day course of 2% clindamycin cream: results of a multicentre, double blind, placebo controlled trial. BV Investigators Group. Genitourin Med. 1995; 71:254-6. https://pubmed.ncbi.nlm.nih.gov/7590720
142. Pharmacia & Upjohn Company. Cleocin HCl (clindamycin hydrochloride capsules) prescribing information. Kalamazoo, MI; 1998 April.
143. Curatek Pharmaceuticals. Clinical monograph on MetroGel-Vaginal (metronidazole vaginal gel). Elk Grove Village, IL; 1992 Dec.
144. Dhar J, Arya OP, Timmina DJ et al. Treatment of bacterial vaginosis with a three day course of 2% clindamycin vaginal cream: a pilot study. Genitourin Med. 1994; 70:121-3. https://pubmed.ncbi.nlm.nih.gov/8206470
145. Fischbach F, Petersen EE, Weissenbacher ER et al. Efficacy of clindamycin vaginal cream versus oral metronidazole in the treatment of bacterial vaginosis. Obstet Gynecol. 1993; 82:405-10. https://pubmed.ncbi.nlm.nih.gov/8355942
146. Livengood CH III, Thomason JL, Hill GB. Bacterial vaginosis: diagnostic and pathogenetic findings during topical clindamycin therapy. Am J Obstet Gynecol. 1990; 163:515-20. https://pubmed.ncbi.nlm.nih.gov/2201189
147. Reviewers’ comments (personal observations).
148. Hillier SL. Diagnostic microbiology of bacterial vaginosis. Am J Obstet Gynecol. 1993; 169:455-9. https://pubmed.ncbi.nlm.nih.gov/8357044
149. Bump RC, Zuspan FP, Buesching WJ III et al. The prevalence, six-month persistence, and predictive values of laboratory indicators of bacterial vaginosis (nonspecific vaginitis) in asymptomatic women. Am J Obstet Gynecol. 1984; 150:917-24. https://pubmed.ncbi.nlm.nih.gov/6391177
150. The Upjohn Company, Kalamazoo, MI: Personal communication.
151. Stein GE, Christensen SL, Mummaw NL et al. Placebo-controlled trial of intravaginal clindamycin 2% cream for the treatment of bacterial vaginosis. Ann Pharmacother. 1993; 27:1343-5. https://pubmed.ncbi.nlm.nih.gov/8286805
152. Eschenbach DA, Duff P, McGregor JA et al. 2% Clindamycin vaginal cream treatment of bacterial vaginosis in pregnancy. Presented at the annual meeting of Infectious Diseases Society for Obstetrics and Gynecology. Stowe, VT: 1993 Aug 4-7. Abstract.
153. Sobel JD. Vaginitis. N Engl J Med. 1997; 337:1896-903. https://pubmed.ncbi.nlm.nih.gov/9407158
154. Ferris DG, Litaker MS, Woodward L et al. Treatment of bacterial vaginosis: a comparison of oral metronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J Fam Pract. 1995; 41:443-9. https://pubmed.ncbi.nlm.nih.gov/7595261
155. Newton ER, Piper J, Peairs W. Bacterial vaginosis and intraamniotic infection. Am J Obstet Gynecol. 1997; 176:672-7. https://pubmed.ncbi.nlm.nih.gov/9077627
156. McGregor JA, French JI, Seo K. Premature rupture of membranes and bacterial vaginosis. Am J Obstet Gynecol. 1993; 169:463-6. https://pubmed.ncbi.nlm.nih.gov/8357046
157. Hay PE, Lamont RF, Taylor-Robinson D et al. Abnormal bacterial colonisation of the genital tract and subsequent preterm delivery and late miscarriage. BMJ. 1994; 308:295-8. https://pubmed.ncbi.nlm.nih.gov/8124116
158. Meis PJ, Goldenberg RL, Mercer B et al. The preterm prediction study: significance of vaginal infections. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1995; 173:1231-5. https://pubmed.ncbi.nlm.nih.gov/7485327
159. Hillier SL, Nugent RP, Eschenbach DA et al. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. The Vaginal Infections and Prematurity Study Group. N Engl J Med. 1995; 333:1737-42. https://pubmed.ncbi.nlm.nih.gov/7491137
160. Ferris DG. Management of bacterial vaginosis during pregnancy. Am Fam Physician. 1998; 57:1215-8. https://pubmed.ncbi.nlm.nih.gov/9531904
161. Morales WJ, Schorr S, Albritton J. Effect of metronidazole in patients with preterm birth in preceding pregnancy and bacterial vaginosis: a placebo-controlled, double-blind study. Am J Obstet Gynecol. 1994; 171:345-7. https://pubmed.ncbi.nlm.nih.gov/8059811
162. Hauth JC, Goldenberg RL, Andrews WW et al. Reduced incidence of preterm delivery with metronidazole and erythromycin in women with bacterial vaginosis. N Engl J Med. 1995; 333:1732-6. https://pubmed.ncbi.nlm.nih.gov/7491136
163. Joesoef MR, Hillier SL, Wiknjosastro G et al. Intravaginal clindamycin treatment for bacterial vaginosis: effects on preterm delivery and low birth weight. Am J Obstet Gynecol. 1995;173:1527-31.
164. McGregor JA, French JI, Jones W et al. Bacterial vaginosis is associated with prematurity and vaginal fluid mucinase and sialidase: results of a controlled trial of topical clindamycin cream. Am J Obstet Gynecol. 1994;170:1048-59.
165. Hack M, Merkatz IR. Preterm delivery and low birth weight—a dire legacy. N Engl J Med. 1995; 333:1772-4. https://pubmed.ncbi.nlm.nih.gov/7491144
166. McGregor JA, French JI, Parker R et al. Prevention of premature birth by screening and treatment for common genital tract infections: results of a prospective controlled evaluation. Am J Obstet Gynecol. 1995; 173:157-67. https://pubmed.ncbi.nlm.nih.gov/7631673
167. Moi H, Erkkola R, Jerve F et al. Should male consorts of women with bacterial vaginosis be treated? Genitourin Med. 1989; 65:263-8.
168. Vejtorp M, Bollerup AC, Vejtorp L et al. Bacterial vaginosis: a double-blind randomized trial of the effect of treatment of the sexual partner. Br J Obstet Gynaecol. 1988; 95:920-6. https://pubmed.ncbi.nlm.nih.gov/3056506
169. Mengel MB, Berg AO, Weaver CH et al. The effectiveness of single-dose metronidazole therapy for patients and their partners with bacterial vaginosis. J Fam Pract. 1989; 28:163-71. https://pubmed.ncbi.nlm.nih.gov/2644391
170. Colli E, Landoni M, Parazzini F. Treatment of male partners and recurrence of bacterial vaginosis: a randomised trial. Genitourin Med. 1997; 73:267-70. https://pubmed.ncbi.nlm.nih.gov/9389947
171. Meadowcroft AM, Diaz PR, Latham GS. Clostridium difficile toxin-induced colitis after use of clindamycin phosphate vaginal cream. Ann Pharmacother. 1998; 32:309-11. https://pubmed.ncbi.nlm.nih.gov/9533061
172. Trexler MF, Fraser TG, Jones MP. Fulminant pseudomembranous colitis caused by clindamycin phosphate vaginal cream. Am J Gastroenterol. 1997; 92:2112-3. https://pubmed.ncbi.nlm.nih.gov/9362204
173. G.D. Searle & Co. Flagyl ER (metronidazole extended release tablets) prescribing information. Chicago, IL; 1998 Mar 9.
174. Peipert JF, Montagno AB, Cooper AS et al. Bacterial vaginosis as a risk factor for upper genital tract infection. Am J Obstet Gynecol. 1997; 177:1184-7. https://pubmed.ncbi.nlm.nih.gov/9396917
175. Reviewers’ comments (personal observations) on metronidazole 8:40.
176. Pharmacia & Upjohn Company. Cleocin vaginal ovules (clindamycin phosphate vaginal suppositories) prescribing information. Kalamazoo, MI; 2003 Jan.
177. Paavonen J, Mangioni C, Martin MA et al. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: a randomized trial. Obstet Gynecol. 2000; 96:256-60. https://pubmed.ncbi.nlm.nih.gov/10908773
178. Stiefel Laboratories. Duac (clindamycin 1%-benzoyl peroxide 5%) topical gel prescribing information. Coral Gables, FL; 2004 Jan.
179. Dermik Laboratories. BenzaClin (clindamycin-benzoyl peroxide) topical gel prescribing information. Bridgewater, NJ; 2007 May.
180. Ther-Rx. Clindesse (clindamycin phosphate) vaginal cream prescribing information. St. Louis, MO; 2004 Nov.
181. Johnson S, Gerding DN. Clostridium difficile-associated diarrhea. Clin Infect Dis. 1998; 26:1027-36. https://pubmed.ncbi.nlm.nih.gov/9597221
182. Gerding DN, Johnson S, Peterson LR et al for the Society for Healthcare Epidemiology of America. Position paper on Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol. 1995; 16:459-77. https://pubmed.ncbi.nlm.nih.gov/7594392
183. Fekety R for the American College of Gastroenterology Practice Parameters Committee. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. Am J Gastroenterol. 1997; 92:739-50. https://pubmed.ncbi.nlm.nih.gov/9149180
184. American Society of Health-System Pharmacists Commission on Therapeutics. ASHP therapeutic position statement on the preferential use of metronidazole for the treatment of Clostridium difficile-associated disease. Am J Health-Syst Pharm. 1998; 55:1407-11. https://pubmed.ncbi.nlm.nih.gov/9659970
185. Wilcox MH. Treatment of Clostridium difficile infection. J Antimicrob Chemother. 1998; 41(Suppl C):41-6. https://pubmed.ncbi.nlm.nih.gov/9630373
186. James WD. Acne. N Engl J Med. 2005; 352:1463-72. https://pubmed.ncbi.nlm.nih.gov/15814882
187. Strauss JS, Krowchuk DP, Leyden JJ et al. Guidelines of care for acne vulgaris management. J Am Acad Dematol. 2007; 56:651-63.
a. AHFS drug information 2004. McEvoy GK, ed. Clindamycin Phosphate. Bethesda, MD: American Society of health-System Pharmacists; 2004:3306-11.
More about clindamycin topical
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (232)
- Side effects
- Dosage information
- During pregnancy
- Drug class: topical acne agents
- Breastfeeding
Patient resources
Professional resources
- Clindacin Foam prescribing information
- Clindamycin Foam (FDA)
- Clindamycin Gel (FDA)
- Clindamycin Lotion (FDA)
- Clindamycin Pledget (FDA)
Other brands
Clindagel, Clindamax, Clindesse, Cleocin Vaginal, ... +4 more