Avapritinib (Monograph)
Brand name: Ayvakit
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; potent and selective inhibitor of platelet-derived growth factor receptor alpha (PDGFR-α), PDGFR-α with D842 mutations, and c-Kit with exon 11, 11/17, and 17 mutations.
Uses for Avapritinib
GI Stromal Tumor (GIST)
Treatment of adults with unresectable or metastatic GIST harboring PDGFR-α exon 18 mutation, including PDGFR-α D842V mutations (designated an orphan drug by FDA for treatment of this cancer). In cases of PDGFR-α exon 18 D842V mutant GIST resistant to imatinib, neoadjuvant avapritinib treatment may be used. Avapritinib is recommended first-line in metastatic disease in PDGFR-α exon 18 D842V mutant disease.
Confirmation of the presence of PDGFR-α exon 18 mutation is necessary prior to initiation of therapy. In clinical studies, presence of PDGFR-α exon 18 mutation was determined by polymerase chain reaction (PCR) or next-generation sequencing (NGS) assay.
Advanced Systemic Mastocytosis (AdvSM)
Treatment of adults with AdvSM, which includes patients with aggressive systemic mastocytosis (ASM), systemic mastocytosis with an associated hematological neoplasm (SM-AHN), and mast-cell leukemia (MCL) (designated an orphan drug by FDA for treatment). Treatment of adult SM is highly individualized. Aggressive SM often requires mast cell-directed cytoreductive treatments to alleviate organ dysfunction; options for treatment include avapritinib, midostaurin, cladribine, imatinib, interferon-α, or allogeneic stem cell transplantation in refractory/relapsed disease.
Indolent Systemic Mastocytosis (ISM)
Treatment of adults with ISM, a clonal disease caused by mast-cell accumulation and activation, primarily driven by the KIT D816V mutation. Designated as an orphan drug by FDA for treatment.
Current recommendations for managment of ISM include treatment with a potent selective mutant KIT inhibitor such as avapritinib.
Avapritinib Dosage and Administration
General
Pretreatment Screening
-
When used for GI stromal tumor (GIST), confirm presence of platelet-derived growth factor receptor alpha (PDGFR-α) exon 18 mutation prior to initiating therapy with avapritinib.
-
In patients with advanced systemic mastocytosis (AdvSM) or indolent systemic mastocytosis (ISM), perform a platelet count before initiating therapy. In patients with platelets <50,000/mm3, avapritinib is not recommended.
-
Confirm pregnancy status prior to initiating avapritinib.
Patient Monitoring
-
Following the initiation of avapritinib for AdvSM, monitor platelet counts every 2 weeks for the first 8 weeks regardless of baseline platelet count; after 8 weeks of treatment, monitor platelet counts every 2 weeks (or more frequently if clinically indicated) if platelets are <75,000/mm3, every 4 weeks if platelets are between 75,000/mm3 and 100,000/mm3, and as clinically indicated if platelets are >100,000/mm3.
-
Monitor patients closely for intracranial hemorrhage, particularly those with thrombocytopenia, vascular aneurysm, or a history of intracranial hemorrhage or cerebrovascular accident within the prior year.
Administration
Oral Administration
Administer orally once daily on an empty stomach (i.e., ≥1 hour before or 2 hours after a meal).
If a dose of avapritinib is missed, administer the missed dose as soon as it is remembered. Do not take a missed dose within 8 hours of the next scheduled dose.
If a dose is vomited, do not repeat the dose to make up for the vomited dose. Take the next dose at the regularly scheduled time.
Dosage
Adults
GIST Harboring PDGFR-α Exon 18 Mutations.
Oral
300 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
AdvSM
Oral
200 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
ISM
Oral
25 mg once daily.
Dosage Modification for Toxicity
Oral
Temporary interruption of therapy, dosage reduction, and/or permanent discontinuance of drug may be necessary. When dosage reduction is required, reduce dosage of avapritinib as described in Table 1.
Permanently discontinue avapritinib in patients with GIST unable to tolerate a dose of 100 mg daily.
Permanently discontinue avapritinib in patients with AdvSM unable to tolerate a dose of 25 mg daily.
|
Dosage Reduction |
GIST |
AdvSM |
|---|---|---|
|
First Dose Reduction |
200 mg once daily |
100 mg once daily |
|
Second Dose Reduction |
100 mg once daily |
50 mg once daily |
|
Third Dose Reduction |
Discontinue avapritinib |
25 mg once daily |
If an adverse reaction occurs, modify dosage accordingly (see Table 2).
|
Adverse Reaction and Severity |
Dosage Modification |
|---|---|
|
Patients with GIST or AdvSM with intracranial hemorrhage |
Any grade: Permanently discontinue therapy |
|
Patients with GIST or AdvSM with cognitive effects |
Grade 1: Continue at same or reduced dosage, or withhold therapy until toxicity resolves or improves to baseline and then resume at same or reduced dosage Grade 2 or 3: Withhold therapy; when toxicity resolves or improves to baseline or grade 1, resume at same or reduced dosage Grade 4: Permanently discontinue therapy |
|
Patients with GIST or AdvSM with other toxicity |
Grade 3 or 4: withhold therapy; when toxicity improves to grade 2 or less, resume at same or reduced dosage |
|
Patients with AdvSM with thrombocytopenia |
Platelets <50,000/mm3: interrupt treatment until platelet count ≥50,000/mm3, then resume at reduced dosage. If platelet counts do not recover to ≥50,000/mm3, consider platelet support |
Dosage Modification for Concomitant Use of CYP3A Inhibitors
Avoid concomitant use of avapritinib with strong or moderate inhibitors of CYP3A. If concomitant use of a moderate CYP3A inhibitor cannot be avoided, reduce the initial dosage for patients with GIST to 100 mg once daily, and for patients with AdvSM to 50 mg once daily.
Avoid concomitant use of avapritinib with strong or moderateCYP3A inhibitors in patients with ISM.
Special Populations
Hepatic Impairment
Mild (total bilirubin concentration ≤ the ULN with AST concentration exceeding ULN, or total bilirubin concentration exceeding ULN, but not >1.5 times ULN, with any AST concentration) or moderate (total bilirubin concentration exceeding 1.5 times ULN, but not >3 times ULN, with any AST concentration) hepatic impairment: No dosage adjustment required.
Dosage adjustments are recommended in patients with severe hepatic impairment (Child-Pugh Class C). The manufacturer recommends 200 mg once daily (for patients with GIST), 100 mg once daily (for patients with AdvSM), and 25 mg every other day (for patients with ISM).
Renal Impairment
Mild or moderate renal impairment (Clcr 30–89 mL/minute): No dosage adjustment required.
Severe renal impairment or end-stage renal disease (Clcr ≤29 mL/minute): No specific dosage recommendations.
Geriatric Patients
No specific dosage recommendations.
Cautions for Avapritinib
Contraindications
-
None.
Warnings/Precautions
Intracranial Hemorrhage
Intracranial hemorrhage (e.g., subdural hematoma, intracranial or cerebral hemorrhage) reported in patients with AdvSM or GIST, including fatalities in <1% of patients. Intracranial hemorrhage not reported in a clinical study in patients with ISM.
Monitor patients closely for risk factors of intracranial hemorrhage, which may include history of vascular aneurysm, intracranial hemorrhage, or cerebrovascular accident within the prior year, concomitant use of anticoagulant drugs, or thrombocytopenia. Advise patients to seek immediate medical attention for signs or symptoms (headache, nausea, vomiting, vision changes, or altered mental status) of intracranial hemorrhage. If intracranial hemorrhagic events of any severity occur, permanently discontinue avapritinib.
Perform a platelet count in patients with advanced systemic mastocytosis (AdvSM) before initiating therapy. In patients with baseline platelets <50,000/mm3, avapritinib is not recommended. Monitor platelet counts every 2 weeks for the first 8 weeks; after 8 weeks of treatment, monitor platelet counts every 2 weeks (or more frequently if clinically indicated) if platelets are <75,000/mm3, every 4 weeks if platelets are 75,000–100,000/mm3, and as clinically indicated if platelets are >100,000/mm3.
Manage platelet counts <50,000/mm3 by reducing avapritinib dosage or interrupting treatment as recommended; avapritinib not recommended in patients with AdvSM or ISM with platelet counts <50,000/mm3.
Cognitive Effects
Avapritinib can cause a broad spectrum of adverse CNS effects (i.e., cognitive impairment; dizziness; hallucinations; sleep, speech, or mood disorders). Median time to initial onset was 8.4 weeks, 2.3 months, and 13.3 weeks in clinical trials for GI stromal tumor (GIST), ISM, and AdvSM, respectively.
Inform patients and their caregivers of the risk of adverse CNS effects. Advise patients not to drive or operate hazardous machinery if they are experiencing adverse CNS effects. If adverse CNS effects occur, interruption of therapy, dosage reduction, and/or permanent discontinuance of avapritinib may be necessary.
Photosensitivity
May cause photosensitivity reactions. Advise patients to limit direct UV exposure during therapy and for 1 week after treatment discontinuation.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. Embryofetal toxicity and teratogenicity demonstrated in animals.
Perform pregnancy test prior to initiating avapritinib therapy in females of reproductive potential.
Avoid pregnancy during therapy and for 6 weeks after the last dose of the drug. Advise females of reproductive potential and males who are partners of such females to use effective contraception while receiving the drug and for 6 weeks after the last dose of the drug.
If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Specific Populations
Pregnancy
May cause fetal harm. Pregnancy should be avoided during avapritinib therapy. If pregnancy occurs during avapritinib therapy, apprise the patient of the potential hazard to the fetus.
Lactation
Not known whether avapritinib or its metabolites distribute into milk or affect milk production or the nursing infant.
Patients should not breast-feed during therapy and for 2 weeks after the last dose of the drug.
Females and Males of Reproductive Potential
Perform a pregnancy test prior to initiation of avapritinib therapy in females of reproductive potential and advise such patients to use effective contraceptive methods while receiving avapritinib and for 6 weeks after the last dose of the drug. In addition, advise males with such female partners to use effective contraceptive methods while receiving avapritinib and for 6 weeks after the last dose of the drug.
Results of animal studies suggest avapritinib may impair male and female fertility.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
In the NAVIGATOR EXPLORER/PATHFINDER, and PIONEER studies, 40%, 62%, and 6% of patients were ≥65 years of age, respectively, and 6%, 21%, and <1% were ≥75 years of age, respectively. No overall differences in safety and efficacy were observed between geriatric patients and younger adults.
Hepatic Impairment
Pharmacokinetics not substantially altered by mild or moderate hepatic impairment; dosage adjustment not necessary in such patients.
Drug exposure was 61% higher in patients with severe hepatic impairment (Child-Pugh Class C) compared with healthy subjects with normal hepatic function. A lower starting dose is recommended in patients with severe hepatic impairment.
Renal Impairment
Pharmacokinetics not substantially altered by mild or moderate renal impairment; dosage adjustment not necessary in such patients. Not studied in patients with severe renal impairment or end-stage renal disease.
Common Adverse Effects
The most common adverse reactions in clinical trials for GIST (occurring in ≥20% of patients receiving avapritinib) include: edema, nausea, fatigue/asthenia, cognitive impairment, vomiting, decreased appetite, diarrhea, hair color changes, increased lacrimation, abdominal pain, constipation, rash, dizziness.
The most common adverse reactions in clinical trials for AdvSM (occurring in ≥20% of patients receiving avapritinib) include: edema, diarrhea, nausea, fatigue/asthenia.
The most common adverse reactions in a clinical trial for ISM (occuring in ≥10% of patients receiving avapritinib) include: eye edema, dizziness, peripheral edema, flushing.
Drug Interactions
Metabolized principally by CYP3A4, CYP3A5, and to a lesser extent by CYP2C9; major circulating metabolites are M690 and M499. Substrate of CYP3A. Formation of M690 is catalyzed by UDP-glucuronosyltransferase (UGT) 1A3.
Avapritinib: Time-dependent inhibitor and inducer of CYP3A. Inhibits 2C9 in vitro. Does not inhibit CYP isoenzymes 1A2, 2B6, 2C8, 2C19, or 2D6 or induce CYP isoenzymes 1A2 or 2B6 at clinically relevant concentrations.
M499: Inhibits CYP isoenzymes 3A, 2C8, and 2C9, but not CYP isoenzymes 1A2, 2B6, 2C19, and 2D6 at clinically relevant concentrations.
Avapritinib: Inhibits P-glycoprotein (P-gp), intestinal breast cancer resistance protein (BCRP), multidrug and toxic compound extrusion protein (MATE) 1, MATE2K, and bile salt export pump (BSEP) in vitro. Does not inhibit organic anion-transporting polypeptides (OATP) 1B1, OATP1B3, organic anion transporter (OAT) 1, OAT3, organic cation transporter (OCT) 1, and OCT2. Not a substrate for P-gp, BCRP, OAT1, OAT3, OCT1, OCT2, OATP1B1, OATP1B3, MATE1, MATE2-K, or BSEP.
M499: Effect on transporter systems not known.
Drugs Affecting Hepatic Microsomal Enzymes
Potent or moderate inhibitors of CYP3A: Possible increased systemic exposure to, and increased toxicity of, avapritinib. Avoid concomitant use. If concomitant use of a moderate CYP3A inhibitor cannot be avoided, reduce avapritinib dosage to 100 mg once daily (for GIST) or 50 mg once daily (for AdvSM).
Potent or moderate inducers of CYP3A: Possible decreased systemic exposure to, and decreased therapeutic efficacy of, avapritinib. Avoid concomitant use.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antifungals, azoles (e.g., fluconazole, itraconazole) |
Itraconazole: Increased avapritinib AUC by 600% expected Fluconazole: Increased avapritinib AUC by 210% expected |
Potent CYP3A inhibitors (e.g., itraconazole): Avoid concomitant use Moderate CYP3A inhibitors (e.g., fluconazole): Avoid concomitant use; if concomitant use cannot be avoided, reduce avapritinib dosage |
|
Efavirenz |
Decreased AUC and peak concentration of avapritinib by 62 and 55%, respectively, expected |
Avoid concomitant use |
|
Proton-pump inhibitors |
No clinically meaningful effect on pharmacokinetics of avapritinib |
|
|
Rifampin |
Decreased AUC and peak concentration of avapritinib by 92 and 72%, respectively |
Avoid concomitant use |
Avapritinib Pharmacokinetics
Absorption
Bioavailability
Median time to peak plasma concentrations is 2–4.1 hours following oral administration.
Systemic exposure increases in a dose proportional manner over dosage range of 30–400 mg daily.
Steady-state concentrations achieved in 15 days; mean accumulation ratio is 3.82 and 6.41 in GIST and systemic mastocytosis, respectively.
Food
Administration with a high-fat, high-calorie meal (i.e., approximately 909 calories, 56 g of fat) increased AUC and peak plasma concentration by 29 and 59%, respectively.
Special Populations
Mild hepatic impairment (total bilirubin concentration not exceeding the ULN with AST concentration exceeding ULN, or total bilirubin concentration exceeding ULN, but not >1.5 times the ULN, with any AST concentration) or moderate hepatic impairment (total bilirubin concentration exceeding 1.5 times ULN, but not >3 times ULN, with any AST concentration) does not affect pharmacokinetics of avapritinib.
Severe hepatic impairment (total bilirubin concentrations >3 times ULN with any AST concentration): Pharmacokinetics not studied.
Mild or moderate renal impairment (Clcr 30–89 mL/minute) does not affect pharmacokinetics of avapritinib.
Severe renal impairment (Clcr ≤29 mL/minute) or end-stage renal disease: Pharmacokinetics not studied.
Age (18–90 years), sex, race, and body weight (39.5–156.3 kg) do not substantially affect pharmacokinetics of avapritinib.
Distribution
Extent
Not known whether avapritinib or its metabolites are distributed into human milk.
Plasma Protein Binding
98.8% (independent of avapritinib concentration).
Elimination
Metabolism
Principally metabolized by CYP3A4, CYP3A5, and to a lesser extent by CYP2C9.
Main circulating metabolites are M690 (hydroxy glucuronide metabolite) and M499 (oxidative metabolite); M499 accounts for approximately 80% of systemic exposure to the drug at steady state.
Elimination Route
Eliminated in feces (70%; 11% as unchanged drug) and urine (18%; 0.23% as unchanged drug).
Half-life
32–57 hours in patients with GIST, 20–39 hours in patients with AdvSM, and 38–45 hours in patients with ISM.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Actions
-
Potent and selective inhibitor of PDGFR-α, PDGFR-α with D842 mutations, and c-Kit with exon 11, 11/17 and 17 mutations.
-
Some mutations in PDGFR-α and c-Kit increase autophosphorylation and activation, independent of ligand binding, of the tyrosine kinase receptor resulting in increased tumor cell proliferation and survival.
-
Inhibits autophosphorylation of PDGFR-α D842V and c-Kit D816V mutations associated with resistance to other tyrosine kinase inhibitors (e.g., imatinib, regorafenib, sunitinib).
-
Demonstrates antitumor activity in patient-derived xenograft models of imatinib-resistant GIST harboring c-Kit exon 11/17 mutations.
-
Inhibits proliferation in KIT mutant murine mastocytoma cell lines and human mast cell leukemia cell lines.
-
M499 metabolite unlikely to contribute to activity of avapritinib at recommended dose.
Advice to Patients
-
Importance of instructing patients to read the manufacturer's patient information.
-
Importance of advising patients to take avapritinib tablets once daily on an empty stomach at least 1 hour before or 2 hours after a meal.
-
If a dose is missed, importance of advising patients to take it as soon as they remember unless the next dose is due in less than 8 hours.
-
If vomiting occurs, a replacement dose should not be administered. Patients should be advised to resume dosing at the time of the next scheduled dose.
-
Risk of intracranial hemorrhagic events. Importance of immediately informing clinician if severe headache, vision problems, severe drowsiness, dizziness, confusion, slurred speech, or paralysis occurs. Importance of regular platelet monitoring in patients being treated for advanced systemic mastocytosis.
-
Risk of adverse CNS effects. Importance of informing clinician if new or worsening manifestations of CNS symptoms (e.g., confusion, speech difficulty, dizziness, drowsiness, forgetfulness, trouble thinking, insomnia, hallucinations, changes in behavior or mood) occur. Necessity of advising patients to avoid driving or operating hazardous machinery if they experience adverse CNS effects.
-
Inform patients that there is a potential risk of photosensitivity reactions with avapritinib. Advise patients to limit direct ultraviolet exposure by using sunscreen and protective clothing during treatment with avapritinib.
-
Risk of fetal harm. Necessity of advising females of reproductive potential and males who are partners of such females that they should use effective methods of contraception during therapy and for 6 weeks after the last dose of the drug. Importance of patients informing their clinicians if they become pregnant during therapy or think they may be pregnant. Advise males and females of reproductive potential of potential risk to the fetus.
-
Importance of advising women to avoid breast-feeding while receiving avapritinib and for 2 weeks after the last dose of the drug.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Avapritinib is available only from designated specialty pharmacies. The manufacturer should be contacted for additional information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
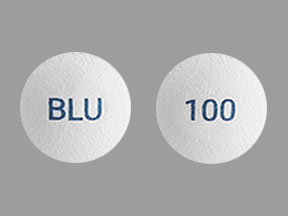
Oral |
Tablets, film-coated |
25 mg |
Ayvakit |
Blueprint Medicines |
|
50 mg |
Ayvakit |
Blueprint Medicines |
||
|
100 mg |
Ayvakit |
Blueprint Medicines |
||
|
200 mg |
Ayvakit |
Blueprint Medicines |
||
|
300 mg |
Ayvakit |
Blueprint Medicines |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Prilosec
Prilosec (omeprazole) is used to treat symptoms of GERD and other conditions caused by excess ...
Prevacid
Prevacid is used to treat and prevent stomach and intestinal ulcers. Learn about side effects ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Gleevec
Gleevec is targeted cancer therapy for specific types of leukemia (blood cancer), bone marrow ...
Gastrocrom
Gastrocrom is used for inflammatory bowel disease, systemic mastocytosis
Ayvakit
Ayvakit (avapritinib) is a prescription medicine used for the treatment of gastrointestinal stromal ...
Midostaurin
Midostaurin is used for acute myeloid leukemia, systemic mastocytosis
Cromolyn
Cromolyn is used for asthma, maintenance, inflammatory bowel disease, systemic mastocytosis
More about avapritinib
- Check interactions
- Compare alternatives
- Reviews (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: multikinase inhibitors
- Breastfeeding
- En español