Ozempic FDA Alerts
The FDA Alerts below may be specifically about Ozempic or relate to a group or class of drugs which include Ozempic.
MedWatch Safety Alerts are distributed by the FDA and published by Drugs.com. Following is a list of possible medication recalls, market withdrawals, alerts and warnings.
Recent FDA Alerts for Ozempic
FDA Warns Consumers Not to Use Counterfeit Ozempic (semaglutide) Found in U.S. Drug Supply Chain
April 14, 2025 -- FDA was notified by Novo Nordisk on April 3, 2025, that several hundred units of counterfeit Ozempic (semaglutide) injection 1 mg were in the U.S. drug supply chain. The counterfeit products were distributed outside the Novo Nordisk authorized supply chain in the U.S. FDA seized the identified counterfeit products on April 9, 2025.
The agency advises patients, wholesalers, retail pharmacies and health care professionals to check the Ozempic products they have received and not use, distribute or sell products labeled with lot number PAR0362 and serial number starting with the first eight digits 51746517 as pictured below.
FDA is aware of six adverse event reports associated with this lot, however none of them appear to be associated with the counterfeit product. All six adverse events were reported by Novo Nordisk.
FDA and Novo Nordisk are testing the seized products and do not yet have information about the identity, quality or safety of these drugs. FDA’s investigation is ongoing, and the agency is working to protect the U.S. drug supply. Visit Novo Nordisk’s announcement for more information.

Source: FDA
FDA Clarifies Policies for Compounders as National GLP-1 Supply Begins to Stabilize
October 2, 2024 -- The U.S. Food and Drug Administration has determined the shortage of tirzepatide injection, a glucagon-like peptide 1 (GLP-1) medication, has been resolved. Tirzepatide injection has been in shortage since 2022 due to increased demand.
FDA confirmed with the drug’s manufacturer that their stated product availability and manufacturing capacity can meet the present and projected national demand. Patients and prescribers may still see intermittent localized supply disruptions as the products move through the supply chain from the manufacturer and distributors to local pharmacies.
FDA reminds compounders of the legal restrictions on making copies of FDA-approved drugs
Compounded drugs are not approved by FDA. FDA-approved drugs go through FDA’s rigorous review for safety, effectiveness, and quality as part of the premarket approval process. Compounded drugs must meet conditions to qualify for exemptions under sections 503A and 503B of the Federal Food, Drug and Cosmetic (FD&C) Act. Among the conditions are:
- Section 503A of the FD&C Act includes restrictions on compounding drugs that are essentially copies of a commercially available drug. When a drug shortage is resolved, FDA generally considers the drug to be commercially available. Certain amounts are permissible under the law as long as the compounding is not done “regularly or in inordinate amounts.”
- Section 503B of the FD&C Act restricts outsourcing facilities from making compounded drugs that are essentially a copy of one or more FDA-approved drugs. Among other things, this means the compounded drug may not be identical or nearly identical to an FDA-approved drug unless the approved drug is on FDA’s drug shortage list.
Current shortage status of GLP-1 products (as of October 02, 2024):
- Tirzepatide injection: Shortage resolved.
- Dulaglutide injection: In shortage.
- Semaglutide injection: In shortage. Manufacturer has reported all but one of the presentations are available.
- Liraglutide injection: In shortage. Manufacturer has reported 2 presentations are available, and three have limited availability.
The agency will continue to work with manufacturers to help resolve the current shortages, and, as shortages resolve, will closely monitor the situation and provide any assistance we can to help manufacturers ensure an adequate supply. Before determining that a shortage is resolved, FDA considers a variety of factors, including the company's ability to meet current and historical demand, the amount in a manufacturer’s stock, affected market share, ability of alternate manufacturers to cover the demand, and confirmed market stabilization. Please visit FDA’s Drug Shortages Database for the most recent information on the status of GLP-1 medicines and other drugs in shortage.
Source: FDA
Drug Safety Communication: Certain Type of Medicines Approved for Type 2 Diabetes and Obesity - Update on FDA’s Ongoing Evaluation of Reports of Suicidal Thoughts or Actions
ISSUE: The FDA has been evaluating reports of suicidal thoughts or actions in patients treated with a class of medicines called glucagon-like peptide-1 receptor agonists (GLP-1 RAs; see the list in Table 1 below). These medicines are used to treat people with type 2 diabetes or to help those with obesity or overweight to lose weight. FDA's preliminary evaluation has not found evidence that use of these medicines causes suicidal thoughts or actions.
Over the last several months, the FDA has conducted detailed reviews of reports of suicidal thoughts or actions received in the FDA Adverse Event Reporting System (FAERS). Because the information provided was often limited and because these events can be influenced by other potential factors, the FDA determined that the information in these reports did not demonstrate a clear relationship with the use of GLP-1 RAs. Similarly, the FDA's reviews of the clinical trials, including large outcome studies and observational studies did not find an association between use of GLP-1 RAs and the occurrence of suicidal thoughts or actions. However, because of the small number of suicidal thoughts or actions observed in both people using GLP-1 RAs and in the comparative control groups, the FDA cannot definitively rule out that a small risk may exist; therefore, the FDA is continuing to look into this issue.
Additional evaluations include a meta-analysis of clinical trials across all GLP-1 RA products and an analysis of postmarketing data in the Sentinel System. A meta-analysis is a large, combined analysis of findings from clinical trials. Sentinel is a very large data network that contains health insurance claims and patient health records that can be used to investigate safety questions about FDA-regulated products. The FDA will communicate final conclusions and recommendations after completion of the review or when there is more information to share.
BACKGROUND:
-
GLP-1 RAs are a class of several medicines used to improve blood sugar (glucose) control and reduce the risk of heart disease in patients with type 2 diabetes. Some of these medicines are also used to help patients with obesity or overweight to lose weight.
RECOMMENDATIONS:
Patients
-
You should not stop taking GLP-1 RAs without first consulting your health care professional, as stopping these medicines may worsen your condition.
-
Talk to your health care professional if you have questions or concerns.
-
Tell your health care professional if you experience new or worsening depression, suicidal thoughts, or any unusual changes in mood or behavior.
-
Call or text 988 or go to the website at https://988lifeline.org/, which provides free support for people in distress 24 hours a day, 7 days a week.
Health Care Professionals
The current prescribing information for the GLP-1 RAs approved to treat patients with obesity or overweight contains information about the risk of suicidal thoughts and actions. This information is also included in the labels of other types of weight loss medicines and is based on reports of such events observed with a variety of older medicines used or tested for weight loss.
-
Consistent with the prescribing information for these medications, health care professionals should monitor for and advise patients using GLP-1 RAs to report new or worsening depression, suicidal thoughts, or any unusual changes in mood or behavior.
-
Health care professionals should consult the prescribing information when treating patients with these medications.
GLP-1 RAs are a class of several medicines (see list in Table 1) used to improve blood sugar (glucose) control and reduce the risk of heart disease in patients with type 2 diabetes. Some of these medicines are also used to help patients with obesity or overweight to lose weight. FDA approved the first GLP-1 RA in 2005, and there are now several in this class. GLP-1 RAs work by mimicking a hormone in the intestines called GLP-1 to stimulate the release of insulin and reduce blood glucose after eating a meal. These medicines also slow down food traveling through the digestive tract, which can help make someone feel full longer. GLP-1 receptors are also present in parts of the brain that regulate appetite.
Table 1. FDA-Approved GLP-1 RAs
|
Trade name |
Generic name |
Population (indication) |
Approval year |
|---|---|---|---|
|
exenatide |
Type 2 diabetes |
2005 |
|
|
liraglutide |
Type 2 diabetes |
2010 |
|
|
dulaglutide |
Type 2 diabetes |
2014 |
|
|
liraglutide |
Obesity/overweight |
2014 |
|
|
lixisenatide |
Type 2 diabetes |
2016 |
|
|
liraglutide + insulin degludec |
Type 2 diabetes |
2016 |
|
|
lixisenatide + insulin glargine |
Type 2 diabetes |
2016 |
|
|
exenatide |
Type 2 diabetes |
2017 |
|
|
semaglutide |
Type 2 diabetes |
2017 |
|
|
semaglutide |
Type 2 diabetes |
2019 |
|
|
semaglutide |
Obesity/overweight |
2021 |
|
|
tirzepatide** |
Type 2 diabetes |
2022 |
|
|
tirzepatide** |
Obesity/overweight |
2023 |
**Tirzepatide is a dual gastric inhibitory polypeptide (GIP) receptor and GLP-1 RA.
Health care professionals, patients and consumers can sign up for email alerts about Drug Safety Communications on medicines or medical specialties of interest to you.
Related Information:
-
The FDA’s Drug Review Process: Ensuring Drugs Are Safe and Effective
-
Think It Through: Managing the Benefits and Risks of Medicines
Health professionals and patients are encouraged to report adverse events or side effects related to the use of these products to the FDA's MedWatch Safety Information and Adverse Event Reporting Program:
- Complete and submit the report online.
- Download form or call 1-800-332-1088 to request a reporting form, then complete and return to the address on form, or submit by fax to 1-800-FDA-0178.
Source: FDA
FDA Warns Consumers Not to Use Counterfeit Ozempic (semaglutide) Found in U.S. Drug Supply Chain
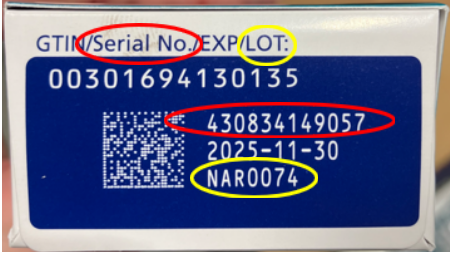
December 21, 2023 -- FDA continues to investigate counterfeit Ozempic (semaglutide) injection 1 milligram (mg) in the legitimate U.S. drug supply chain and has seized thousands of units of the product. The agency advises wholesalers, retail pharmacies, health care practitioners and patients to check the product they have received and not distribute, use, or sell products labeled with lot number NAR0074 and serial number 430834149057 as pictured below. Some counterfeit products may still be available for purchase.
FDA and Novo Nordisk (manufacturer of Ozempic) are testing the seized products and do not yet have information about the drugs’ identity, quality, or safety.
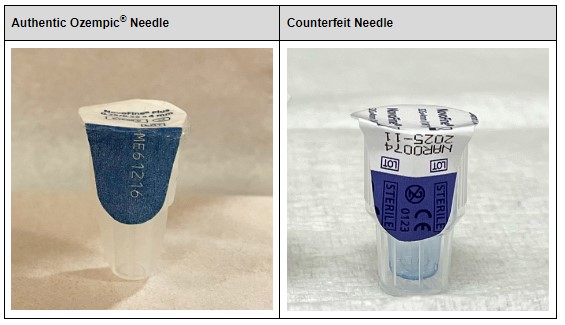
Additionally, analysis found the needles from the samples are counterfeit. Accordingly, the sterility of the needles cannot be confirmed, which presents an increased risk of infection for patients who use the counterfeit products. Based on analyses completed to date, other confirmed counterfeit components within the seized products are the pen label, accompanying health care professional and patient information, and carton.
FDA is aware of five adverse events from this lot, none of which are serious and are consistent with known common adverse reactions to authentic Ozempic, which are nausea, vomiting, diarrhea, abdominal pain and constipation.
FDA recommends retail pharmacies only purchase authentic Ozempic through authorized distributors of Novo Nordisk and review the photographs and information to confirm the legitimacy of their shipments. Patients should only obtain Ozempic with a valid prescription through state-licensed pharmacies and check the product before using for any signs of counterfeiting.
FDA takes reports of possible counterfeit products seriously and works closely with other federal agencies and the private sector to help protect the nation’s drug supply. FDA’s investigation is ongoing, and the agency is working with Novo Nordisk to identify, investigate, and remove further suspected counterfeit semaglutide injectable products found in the U.S.
Health care professionals and consumers should report adverse events or side effects related to the use of this product to FDA’s MedWatch Safety Information and Adverse Event Reporting Program:
- Complete and submit the report online at MedWatch Online Voluntary Reporting Form or
- Download and complete the form, then submit it via fax at 1-800-FDA-0178.
Entities, including online sellers, selling counterfeit and/or tampered medicines should be reported to FDA. Suspected counterfeit products may be reported to FDA by calling your local FDA consumer complaint coordinator or by reporting it directly at report suspected criminal activity.
Retailers and patients may also contact Novo Nordisk customer care at 1-800-727-6500 Monday through Friday from 8:30 a.m. to 6 p.m. ET with questions or concerns.
Visuals of authentic and counterfeit needles are shown below:

More information: Medications Containing Semaglutide Marketed for Type 2 Diabetes or Weight Loss
Source: FDA
FDA Issues Warning About Compounded Medications Containing Semaglutide Marketed for Type 2 Diabetes or Weight Loss
On May 30, 2023, the FDA posted information about medications containing semaglutide marketed for type 2 diabetes or weight loss. There are currently three FDA-approved semaglutide products which are only available with a prescription. Due to two of the drugs being in shortage, these two drugs are able to be compounded if they meet certain requirements in the Federal Food, Drug, and Cosmetic Act. The FDA has received adverse event reports after patients used compounded semaglutide. The FDA has also received reports that in some cases, compounders may be using salt forms of semaglutide, including semaglutide sodium and semaglutide acetate, which have not been shown to be safe or effective. The salt forms are different active ingredients than is used the approved drugs, which contain the base form of semaglutide. Patients should be aware that some products sold as 'semaglutide' may not contain the same active ingredient as FDA-approved semaglutide products and may be the salt formulations. Patients should only obtain drugs containing semaglutide with a prescription from a licensed health care provider, and only obtain medicines from state-licensed pharmacies or outsourcing facilities registered with the FDA.
What is semaglutide?
Semaglutide belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists. It mimics the GLP-1 hormone that is released in the gastrointestinal tract in response to eating. One role of GLP-1 is to prompt the body to produce more insulin, which reduces blood glucose (sugar). GLP-1 in higher amounts also interacts with the parts of the brain that reduce appetite and signal a feeling of fullness.
There are currently three FDA-approved semaglutide products:
- Ozempic injection and Rybelsus tablets are approved to lower blood sugar levels in adults with type 2 diabetes mellitus, in addition to diet and exercise. Ozempic is also approved to reduce the risk of heart attack, stroke, or death in adults with type 2 diabetes mellitus and known heart disease.
- Wegovy injection is approved to help adults and children aged 12 years and older with obesity or some adults with excess weight (overweight), who also have weight-related medical problems, to lose weight and keep the weight off, in addition to diet and exercise.
All three medications are only available with a prescription, and there are no approved generic versions.
What is compounding?
Drug compounding is the process of combining, mixing, or altering ingredients to create a medication tailored to the needs of an individual patient. Compounding includes the combining of two or more drugs. Compounded drugs are not FDA-approved, and the agency does not verify the safety or effectiveness of compounded drugs.
Can semaglutide be compounded?
When a drug is in shortage, compounders may be able to prepare a compounded version of that drug if they meet certain requirements in the Federal Food, Drug, and Cosmetic (FD&C) Act. As of May 2023, Ozempic and Wegovy are both listed on FDA’s Drug Shortages list.
Are there concerns with compounded semaglutide?
FDA has received adverse event reports after patients used compounded semaglutide. Patients should not use a compounded drug if an approved drug is available to treat a patient. Patients and health care professionals should understand that the agency does not review compounded versions of these drugs for safety, effectiveness, or quality.
Additionally, FDA has received reports that in some cases, compounders may be using salt forms of semaglutide, including semaglutide sodium and semaglutide acetate. The salt forms are different active ingredients than is used the approved drugs, which contain the base form of semaglutide. The agency is not aware of any basis for compounding using the salt forms that would meet the FD&C requirements for types of active ingredients that can be compounded. On April 27, 2023, FDA wrote to the National Association of Boards of Pharmacy expressing the agency’s concerns with use of the salt forms in compounded products.
What should patients know?
Patients should be aware that some products sold as ‘semaglutide’ may not contain the same active ingredient as FDA-approved semaglutide products and may be the salt formulations. Products containing these salts, such as semaglutide sodium and semaglutide acetate, have not been shown to be safe and effective.
Patients should only obtain drugs containing semaglutide with a prescription from a licensed health care provider, and only obtain medicines from state-licensed pharmacies or outsourcing facilities registered with FDA.
Purchasing medicine online from unregulated, unlicensed sources can expose patients to potentially unsafe products that have not undergone appropriate evaluation or approval, or do not meet quality standards. If you choose to use an online pharmacy, FDA’s BeSafeRx campaign resources and tools can assist in making safer, more informed decisions when purchasing prescription medicine online.
What should health care professionals know?
Health care professionals who are considering working with compounders to obtain semaglutide products should be aware that compounders may be using salt forms of semaglutide. FDA is not aware of any basis for compounding a drug using semaglutide salts that would meet federal requirements.
Reporting issues to the FDA
FDA encourages health care professionals, patients, and compounders to report adverse events or quality problems with these or any medications to FDA’s MedWatch Adverse Event Reporting program:
- Complete and submit the report online; or
- Download and complete the form, then submit it via fax at 1-800-FDA-0178.
Source: FDA
