Hypoxemia
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is hypoxemia?
Hypoxemia occurs when there is a low level of oxygen in your blood. Oxygen is needed to keep your organs and tissues alive. Long-term hypoxemia can become life threatening if it is not treated.
What are common causes of hypoxemia?
- Anemia
- Respiratory conditions such as pneumonia, pulmonary edema, and pulmonary embolism
- Respiratory diseases such as COPD, ARDS, and interstitial lung diseases
- High altitudes, especially during exercise
- Sleep apnea or blocked airways
- Medicines such as anesthetics or narcotics
- Heart disease present at birth
What are the symptoms of hypoxemia?
- Feeling of not being able to catch your breath
- Frequent headaches
- Severe sleepiness
- Severe mood changes or irritability
Drugs used to treat this and similar conditions
Symbicort
Symbicort (budesonide and formoterol) is used to prevent bronchospasm in people with asthma or ...
Mucinex
Mucinex (guaifenesin) is used to relieve the symptoms of cough and loosen mucus in the chest ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Azithromycin Dose Pack
Azithromycin Dose Pack is used for babesiosis, bacterial endocarditis prevention, bacterial ...
Trelegy Ellipta
Trelegy Ellipta is an inhalation powder used to improve symptoms and prevent bronchospasm in adults ...
Wegovy
Wegovy is a once-weekly semaglutide injection used for chronic weight management and to reduce ...
Mounjaro
Mounjaro (tirzepatide) is FDA-approved to manage type 2 diabetes in adults. It lowers blood sugar ...
Breztri Aerosphere
Breztri (budesonide/glycopyrrolate/formoterol fumarate) is a combination inhaler that may be used ...
Topiramate
Topiramate systemic is used for bipolar disorder, borderline personality disorder, bulimia ...
Amoxicillin
Amoxicillin is a penicillin antibiotic that fights bacteria. It is used to treat many types of ...
How is hypoxemia diagnosed?
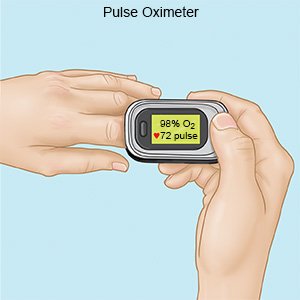
Hypoxemia is diagnosed by measuring the amount of oxygen in your blood. This is done by pulse oximetry or by an arterial blood gas (ABG) test. Pulse oximetry is done using a small instrument placed on your finger. The pulse oximeter gives a digital reading of the amount of oxygen in your blood. During an ABG, your healthcare provider will remove a small amount of blood from an artery on the underside of your wrist. The blood will be tested for the amount of oxygen it contains.
 |
How is hypoxemia treated?
Treatment will depend on how severe your hypoxemia is.
- Oxygen therapy may be needed for activity, such as exercise. You may need oxygen only when you sleep. Your healthcare provider may have you use oxygen all the time if you have severe hypoxemia.
- Pulmonary rehabilitation (PR) may be ordered if the cause of your hypoxemia is related to certain conditions, such as COPD. PR consists of exercise training and nutrition and disease education. You will learn ways to conserve (save) your energy and develop a breathing action plan. PR also offers counseling and support groups.
When should I contact my healthcare provider?
- Your symptoms do not change or become worse with treatment.
- You have questions or concerns about your condition or care.
When should I seek immediate care?
- You have fainting spells with activity.
- You have chest pain.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Hypoxemia
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
