Hiatal Hernia
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is a hiatal hernia?
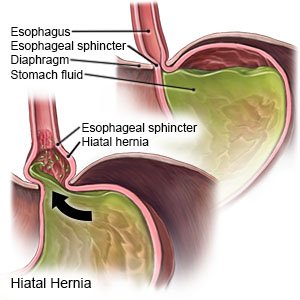
A hiatal hernia is a condition that causes part of your stomach to bulge through the hiatus (small opening) in your diaphragm. The part of the stomach may move up and down, or it may get trapped above the diaphragm.
 |
What increases my risk for a hiatal hernia?
The exact cause of a hiatal hernia is not known. You may have been born with a large or weak hiatus. The following may increase your risk for a hiatal hernia:
- High body weight, pregnancy, or chronic constipation
- Age older than 50 years
- A chronic cough
- Intense exercise or lifting heavy objects often
- A medical condition such as diverticulosis or esophagitis
- Past esophagus or stomach surgery or trauma, such as from a motor vehicle accident
What are the types of hiatal hernia?
- Type I (sliding hiatal hernia) happens when the stomach slides in and out of the hiatus. This type is the most common and may cause gastroesophageal reflux disease (GERD). GERD occurs when the esophageal sphincter does not close properly and causes acid reflux. The esophageal sphincter is the lower muscle of the esophagus.
- Type II (paraesophageal hiatal hernia) develops when a part of the stomach squeezes through the hiatus and forms a bulge next to the esophagus.
- Type III (combined hiatal hernia) is a combination of a sliding and a paraesophageal hiatal hernia.
- Type IV (complex paraesophageal hiatal hernia) happens when 2 or more abdominal organs slide through the hiatus. The stomach, small and large bowels, spleen, pancreas, or liver may be pushed up into your chest.
What are the signs and symptoms of a hiatal hernia?
The most common symptom is heartburn. This may occur after meals and can spread to your neck, jaw, or shoulder. You may have no signs or symptoms, or you may have any of the following:
- Abdominal pain, especially in the area just above your bellybutton
- Bitter or acid taste in your mouth
- Trouble swallowing
- Cough or hoarseness
- Chest pain or shortness of breath after you eat
- Burping or hiccups that happen often
- Feeling full soon after you start eating
How is a hiatal hernia diagnosed?
Your healthcare provider will ask about your symptoms and when they started. Tell your provider about other medical conditions you have, your eating habits, and your activities. You may also need any of the following:
- An upper GI series test includes x-rays of your esophagus, stomach, and your small intestines. It is also called a barium swallow test. You will be given barium (a chalky liquid) to drink before the pictures are taken. This liquid helps your stomach and intestines show up better on the x-rays. An upper GI series can show if you have an ulcer, a blocked intestine, or other problems.
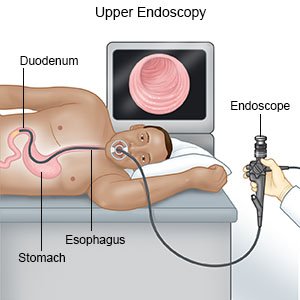
- An endoscopy uses a scope to see the inside of your esophagus and stomach. A scope is a long, bendable tube with a light on the end. A camera may be hooked to the scope to take pictures.
- Esophageal manometry measures the pressure within the esophagus and stomach.
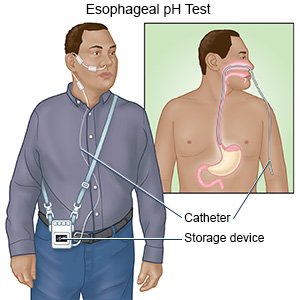
- Esophageal pH monitoring measures the amount of stomach acid that enters your esophagus. A small probe is placed inside the esophagus to check the pH level. The pH level measures how acidic or alkaline (basic) something is.
How is a hiatal hernia treated?
Treatment depends on the type of hiatal hernia you have and on your symptoms. You may not need any treatment. Any of the following may be used to treat the hernia or symptoms it causes:
- Medicines may be given to relieve heartburn symptoms. These medicines help to decrease or block stomach acid. You may also be given medicines that help tighten the esophageal sphincter.
- Surgery may be done when medicines cannot control your symptoms, or other problems are present. Your healthcare provider may also suggest surgery depending on the type of hernia you have. A surgeon can put your stomach back into its normal location. The surgeon may make the hiatus (hole) smaller and anchor your stomach in your abdomen. Fundoplication is a surgery that wraps the upper part of the stomach around the esophageal sphincter to strengthen it.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
- omeprazole
- famotidine
- lansoprazole
- aluminum hydroxide/magnesium hydroxide/simethicone
- aluminum hydroxide/magnesium trisilicate
How can I manage my symptoms?
The following nutrition and lifestyle changes may be recommended to relieve symptoms of heartburn:
 |
- Avoid foods or drinks that may increase heartburn. These include chocolate, peppermint, fatty or fried foods, drinks that contain caffeine, or carbonated drinks (soda). Other foods include spicy foods, onions, tomatoes, and tomato-based foods. Do not have foods or drinks that can irritate your esophagus, such as citrus fruits, juices, and alcohol.
- Eat several small meals during the day. When you eat a lot of food at one time, your stomach needs more acid to digest it. Eat 6 small meals each day instead of 3 large meals. Eat slowly.
- Do not lie down after you eat. Do not eat meals 2 to 3 hours before bedtime.
- Do not put pressure on your abdomen. Pressure may worsen your hiatal hernia. Do not wear clothing that is tight around your waist. Do not bend forward after you eat.
- Maintain a healthy weight. If your body weight is higher than recommended, weight loss may help relieve your symptoms. Your healthcare provider will tell you what a healthy weight is for you. Your provider can help you create a safe weight loss plan, if needed.
- Elevate the head of your bed. Place 6-inch blocks under the head of your bed frame. You may also place more than one pillow or a foam wedge under your head and shoulders when you sleep.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars may worsen heartburn. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
Call your local emergency number (911 in the US) if:
- You have severe chest pain and sudden trouble breathing.
When should I seek immediate care?
- You have severe abdominal pain.
- You try to vomit but nothing comes out (retching).
- Your bowel movements are black or bloody.
- Your vomit looks like coffee grounds or has blood in it.
- You cannot swallow food or liquids.
When should I call my doctor?
- Your symptoms get worse or do not improve with treatment.
- You are losing weight without trying.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Hiatal Hernia
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
