Imbruvica Side Effects
Generic name: ibrutinib
Note: This document provides detailed information about Imbruvica Side Effects associated with ibrutinib. Some dosage forms listed on this page may not apply specifically to the brand name Imbruvica.
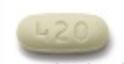
Applies to ibrutinib: oral capsule, oral suspension, oral tablet.
Precautions
It is very important that your doctor check your progress at regular visits while you are using this medicine. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it. Blood and urine tests may be needed to check for unwanted effects.
Using this medicine while you are pregnant can harm your unborn baby. If you are a woman who can bear children, your doctor may give you a pregnancy test before you start using this medicine to make sure you are not pregnant. Women should use an effective form of birth control during treatment and for 1 month after the last dose. Men should use an effective form of birth control during treatment and for 1 month after the last dose to prevent pregnancy in a sexual partner. If you think a pregnancy has occurred with this medicine, tell your doctor right away.
This medicine may cause bleeding problems. Check with your doctor right away if you have bloody or black, tarry stools, red or dark brown urine, severe stomach pain, unusual bleeding, bruising, or weakness, or vomiting of blood or material that looks like coffee grounds.
Make sure any doctor or dentist who treats you knows that you are using this medicine. You may need to stop using this medicine several days before and after having surgery.
This medicine may increase your risk of developing infections, including a serious brain infection called progressive multifocal leukoencephalopathy. Call your doctor right away if you have a cough that would not go away, back pain, dizziness or drowsiness, weight loss, night sweats, fever, chills, or flu-like symptoms, such as a runny or stuffy nose, headache, blurred vision, or feeling generally ill.
Ibrutinib can temporarily lower the number of white blood cells in your blood, increasing the chance of getting an infection. It can also lower the number of platelets, which are necessary for proper blood clotting. If this occurs, there are certain precautions you can take, especially when your blood count is low, to reduce the risk of infection or bleeding:
- If you can, avoid people with infections. Check with your doctor immediately if you think you are getting an infection or if you get a fever or chills, cough or hoarseness, lower back or side pain, or painful or difficult urination.
- Check with your doctor immediately if you notice any unusual bleeding or bruising, black, tarry stools, blood in the urine or stools, or pinpoint red spots on your skin.
- Be careful when using a regular toothbrush, dental floss, or toothpick. Your medical doctor, dentist, or nurse may recommend other ways to clean your teeth and gums. Check with your medical doctor before having any dental work done.
- Do not touch your eyes or the inside of your nose unless you have just washed your hands and have not touched anything else in the meantime.
- Be careful not to cut yourself when you are using sharp objects such as a safety razor or fingernail or toenail cutters.
- Avoid contact sports or other situations where bruising or injury could occur.
Check with your doctor right away if you have chest pain or tightness, decreased urine output, dilated neck veins, irregular breathing, irregular heartbeat, swelling of the face, fingers, feet, or lower legs, trouble breathing, unusual tiredness or weakness, or weight gain. These may be symptoms of a serious heart problem (eg, heart rhythm problems, heart failure).
This medicine may cause a heart condition called atrial flutter or atrial fibrillation. Check with your doctor right away if you have a fast or irregular heartbeat, trouble breathing, lightheadedness, dizziness, or fainting.
Your doctor will check your blood pressure on a regular basis while you are using this medicine. You might need to monitor your blood pressure at home. Tell your doctor right away if you have a severe headache, lightheadedness, or changes in your vision.
Using this medicine may increase your risk of getting new cancers, including skin cancer. Talk to your doctor if you have concerns about this risk.
This medicine may cause a serious type of reaction called tumor lysis syndrome. Your doctor may give you a medicine to help prevent this. Call your doctor right away if you have a change in how much or how often you urinate, joint pain, rapid weight gain, muscle or joint pain, swelling of the feet or lower legs, or unusual tiredness or weakness.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of Imbruvica
Along with its needed effects, ibrutinib (the active ingredient contained in Imbruvica) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking ibrutinib:
More common side effects
- back pain
- bladder pain
- bloating or swelling of the face, arms, hands, lower legs, or feet
- bloody or black, tarry stools
- bloody or cloudy urine
- blurred vision
- body aches or pain
- chest pain or tightness
- chills
- confusion
- cough
- decreased frequency or amount of urine
- difficult, burning, or painful urination
- dizziness or lightheadedness
- drowsiness
- dry mouth
- fainting
- fast or irregular heartbeat
- fever
- frequent urge to urinate
- headache
- hoarseness
- increased thirst
- irregular heartbeat
- itching
- loss of appetite
- lower back or side pain
- nausea
- rapid weight gain
- seizures
- severe headache
- severe stomach pain
- sore throat
- tingling of the hands or feet
- trouble breathing
- ulcers, sores, or white spots in the mouth
- unusual bleeding or bruising
- unusual tiredness or weakness
- unusual weight gain or loss
- vomiting
- vomiting of blood or material that looks like coffee grounds
- wrinkled skin
Less common side effects
- persistent non-healing sore
- pink skin growth
- reddish skin patch or irritated area
- shiny skin bump
- white, yellow or waxy scar-like area on the skin
Incidence not known
- blistering, peeling, or loosening of the skin
- dark urine
- diarrhea
- dilated neck veins
- difficulty swallowing
- general feeling of tiredness or weakness
- hives, skin rash
- joint pain, stiffness, or swelling
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- light-colored stools
- muscle pain
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- red skin lesions, often with a purple center
- red, irritated eyes
- yellow eyes or skin
Other side effects of Imbruvica
Some side effects of ibrutinib may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- belching
- decreased appetite
- difficulty having a bowel movement
- heartburn or indigestion
- indigestion
- lack or loss of strength
- muscle stiffness or spasms
- small red or purple spots on the skin
- stomach discomfort, upset, or pain
- swelling or inflammation of the mouth
See also:
For healthcare professionals
Applies to ibrutinib: oral capsule, oral suspension, oral tablet.
General adverse events
The most common adverse reactions in patients with B-cell malignancies were thrombocytopenia, diarrhea, fatigue, musculoskeletal pain, neutropenia, rash, anemia, bruising, nausea, hemorrhage, arthralgia, and upper respiratory tract infection.
The most common adverse reactions in patients with chronic graft-versus-host disease were fatigue, anemia, bruising, diarrhea, thrombocytopenia, musculoskeletal pain, pyrexia, muscle spasms, stomatitis, hemorrhage, nausea, abdominal pain, pneumonia, and headache.[Ref]
Cardiovascular
- Very common (10% or more): Hypertension (up to 42%), atrial fibrillation (up to 15%), sinus tachycardia (up to 11%)
- Common (1% to 10%): Atrial flutter, cardiac failure, ventricular tachyarrhythmias (includes ventricular extrasystoles, ventricular arrhythmias, ventricular fibrillation, ventricular flutter, ventricular tachycardia), deaths due to cardiac causes/sudden deaths
- Uncommon (0.1% to 1%): Cardiac arrest
- Frequency not reported: Cardiac arrhythmias
- Postmarketing reports: Cardiac failure, ventricular tachyarrhythmia
Hypertension occurred in 19% of 1476 patients with B-cell malignancies who received this drug in clinical trials; grade 3 or greater hypertension occurred in 8% of patients. Based on data from a subset of these patients (N=1124), the median time to onset was 5.9 months (range: 0 to 24 months). In a long-term safety analysis over 5 years of 1284 patients with B-cell malignancies treated for a median of 36 months (range: 0 to 98 months), the cumulative rate of hypertension increased over time. The prevalence for grade 3 or greater hypertension was 4% (year 0 to 1), 7% (year 1 to 2), 9% (year 2 to 3), 9% (year 3 to 4), and 9% (year 4 to 5); the overall incidence for the 5-year period was 11%.
Fatal and serious cardiac arrhythmias and cardiac failure have occurred with this drug. Deaths due to cardiac causes or sudden deaths occurred in 1% of 4896 patients who received this drug in clinical trials, including in those who received this drug in unapproved monotherapy or combination regimens. These adverse reactions occurred in patients with and without preexisting hypertension or cardiac comorbidities.
Grade 3 or greater ventricular tachyarrhythmias were reported in 0.2%, grade 3 or greater atrial fibrillation and atrial flutter were reported in 3.7%, and grade 3 or greater cardiac failure was reported in 1.3% of 4896 patients who received this drug in clinical trials, including in those who received this drug in unapproved monotherapy or combination regimens, and especially in patients with acute infections or cardiac risk factors (including hypertension, diabetes mellitus, history of cardiac arrhythmias).
Dermatologic
- Very common (10% or more): Bruising/contusion (up to 51%), rash (up to 49%), petechiae (up to 16%), skin infection (up to 18%), pruritus (up to 13%)
- Common (1% to 10%): Erythema, urticaria
- Uncommon (0.1% to 1%): Angioedema
- Postmarketing reports: Angioedema, urticaria, Stevens-Johnson syndrome, onychoclasis, panniculitis, neutrophilic dermatoses, erythema
Gastrointestinal
- Very common (10% or more): Diarrhea (up to 59%), nausea (up to 40%), stomatitis (up to 29%), abdominal pain (up to 23%), constipation (up to 22%), vomiting (up to 19%), dyspepsia (up to 16%), gastroesophageal reflux disease (up to 12%)
Genitourinary
- Very common (10% or more): Urinary tract infection (up to 13%)
Hematologic
- Very common (10% or more): Decreased platelets (up to 69%), neutropenia (up to 66%), decreased neutrophils (up to 55%), decreased hemoglobin (up to 49%), bleeding events (including bruising, petechiae; up to 39%), thrombocytopenia (up to 36%), hemorrhage (up to 32%), anemia (up to 17%), lymphocytosis (up to 15%)
- Common (1% to 10%): Major hemorrhage (e.g., intracranial hemorrhage [including subdural hematoma], gastrointestinal bleeding, hematuria, postprocedural hemorrhage), febrile neutropenia, leukocytosis, subdural hematoma
- Uncommon (0.1% to 1%): Fatal bleeding events, leukostasis syndrome
Fatal bleeding events have occurred in patients who received this drug. Major hemorrhage (grade 3 or greater, serious, or any central nervous system events, e.g., intracranial hemorrhage [including subdural hematoma], gastrointestinal bleeding, hematuria, and postprocedural hemorrhage) occurred in 4.2% of patients, with fatalities occurring in 0.4% of 2838 patients who received this drug in 27 clinical trials. Bleeding events (any grade) including bruising and petechiae occurred in 39% and excluding bruising and petechiae occurred in 23% of patients who received this drug, respectively.
Across clinical trials, 3.1% of 2838 patients who received this drug without antiplatelet or anticoagulant therapy experienced major hemorrhage. The addition of antiplatelet therapy (with or without anticoagulant therapy) increased the incidence to 4.4%, and the addition of anticoagulant therapy (with or without antiplatelet therapy) increased the incidence to 6.1%.
In 645 patients with B-cell malignancies who received this drug as a single agent, grade 3 or 4 neutropenia occurred in 23% of patients, grade 3 or 4 thrombocytopenia in 8% of patients, and grade 3 or 4 anemia in 2.8% of patients, based on laboratory measurements.
Hepatic
- Very common (10% or more): Increased bilirubin (up to 30%), increased AST (up to 25%), increased ALT (up to 11%)
- Postmarketing reports: Hepatic failure (including acute events, fatal events), hepatic cirrhosis, hepatitis B reactivation, hepatotoxicity
Hypersensitivity
- Postmarketing reports: Anaphylactic shock
Immunologic
- Very common (10% or more): Hypogammaglobulinemia (up to 11%)
Metabolic
- Very common (10% or more): Hyperuricemia (up to 19%), decreased appetite (up to 16%), hypokalemia (up to 15%)
- Common (1% to 10%): Tumor lysis syndrome, hyponatremia
- Postmarketing reports: Tumor lysis syndrome
Musculoskeletal
- Very common (10% or more): Musculoskeletal pain (up to 61%), arthralgia (up to 41%), muscle spasms (up to 29%), osteonecrosis (up to 11%)
Nervous system
- Very common (10% or more): Headache (up to 40%), dizziness (up to 21%), peripheral neuropathy (up to 19%)
- Common (1% to 10%): Ischemic cerebrovascular events (includes cerebrovascular accidents, ischemic stroke, cerebral ischemia, transient ischemic attack)
- Frequency not reported: Progressive multifocal leukoencephalopathy
- Postmarketing reports: Peripheral neuropathy, cerebrovascular accident, transient ischemic attack, ischemic stroke
Ocular
- Very common (10% or more): Dry eye (up to 17%), blurred vision (up to 13%), increased lacrimation (up to 13%), reduced visual acuity (up to 11%), conjunctivitis (up to 11%)
- Postmarketing reports: Eye hemorrhage
Oncologic
- Very common (10% or more): Second malignancies (10%), other malignancies (including nonskin carcinomas; 10%)
- Common (1% to 10%): Nonmelanoma skin cancer, nonskin carcinomas, basal cell carcinoma, squamous cell carcinoma
- Frequency not reported: Histiocytic sarcoma
Other malignancies (10%), including nonskin carcinomas (3.9%), occurred among the 1476 patients with B-cell malignancies who received this drug in clinical trials. The most frequent second primary malignancy was nonmelanoma skin cancer (6%).
Other
- Very common (10% or more): Fatigue (up to 80%), pyrexia (up to 30%), peripheral edema (up to 28%), infusion related reaction (up to 25%), pain (up to 23%), infections (at least 21%), fall (up to 17%), asthenia (up to 14%), chills (up to 12%), sepsis (up to 11%), decreased weight (10%)
- Uncommon (0.1% to 1%): Cryptococcal infections, Pneumocystis infections, Aspergillus infections
- Frequency not reported: Fatal/nonfatal infections (including bacterial, viral, fungal)
Fatal and nonfatal infections (including bacterial, viral, or fungal) have occurred with this drug. Grade 3 or greater infections occurred in 21% of 1476 patients with B cell malignancies who received this drug in clinical trials.
Psychiatric
- Very common (10% or more): Insomnia (up to 16%)
Renal
- Very common (10% or more): Increased blood creatinine (up to 38%)
Respiratory
- Very common (10% or more): Upper respiratory tract infection (up to 47%), cough (up to 32%), pneumonia (up to 23%), dyspnea (up to 22%), sinusitis (up to 22%), oropharyngeal pain (up to 14%), bronchitis (up to 13%), nasopharyngitis (up to 12%), influenza (up to 12%), viral upper respiratory tract infection (up to 11%)
- Common (1% to 10%): Epistaxis
- Frequency not reported: Pneumocystis jirovecii pneumonia, acute respiratory distress syndrome
- Postmarketing reports: Interstitial lung disease
References
1. (2023) "Product Information. Imbruvica (ibrutinib)." Pharmacyclics Inc, SUPPL-40
2. (2023) "Product Information. Imbruvica (ibrutinib)." Janssen-Cilag Pty Ltd
3. (2023) "Product Information. Imbruvica (ibrutinib)." Janssen-Cilag Ltd
Frequently asked questions
- How much does Imbruvica cost?
- How long can you stay on Imbruvica (ibrutinib)?
- How quickly does Imbruvica (ibrutinib) work?
- Does ibrutinib cause hair loss?
- How to apply for and use the Imbruvica copay card?
- Is Imbruvica a chemotherapy drug?
- What are the names of the BTK inhibitors?
- Who makes Imbruvica?
More about Imbruvica (ibrutinib)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (69)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- FDA approval history
- Drug class: BTK inhibitors
- Breastfeeding
- En español
Patient resources
Professional resources
Related treatment guides
Further information
Imbruvica side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.