Subdural hematoma
Medically reviewed by Drugs.com. Last updated on Jun 16, 2025.
What is Subdural hematoma?

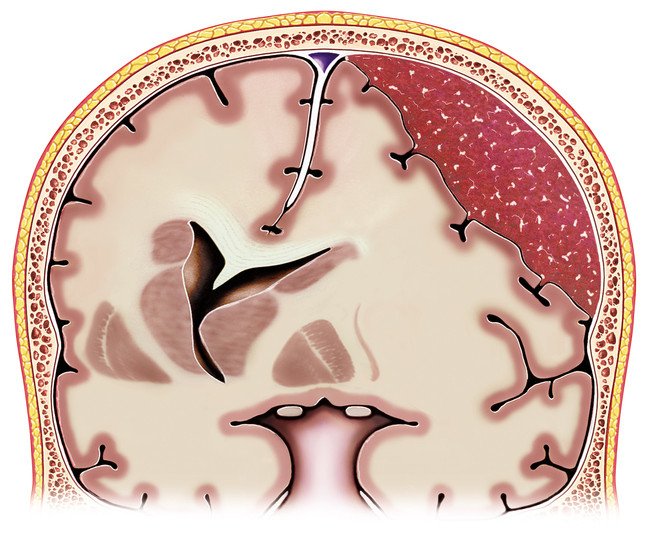
A subdural hematoma occurs when a blood vessel near the surface of the brain bursts. Blood builds up between the brain and the brain's tough outer lining. The condition is also called a subdural hemorrhage.
In a subdural hematoma, blood collects immediately beneath the dura mater. The dura mater is the outermost layer of the meninges. The meninges is the three-layer protective covering of the brain.
A subdural hematoma is a life-threatening problem because it can compress the brain.
|
|
Most subdural hemorrhages result from trauma to the head. The trauma damages tiny veins within the meninges.
In young, healthy people, bleeding usually is triggered by a significant impact. This type of impact might occur in a high-speed motor vehicle accident.
In contrast, older people may bleed after only a minor trauma. For example, it might happen from falling out of a chair.
A subdural hematoma is also more common in people
- taking medications that thin the blood
- who abuse alcohol
- who have seizures.
An acute subdural hemorrhage is bleeding that develops shortly after a serious blow to the head. Blood accumulates rapidly, causing pressure to rise within the brain. This can result in loss of consciousness, paralysis, or death.
When bleeding develops slowly, it is known as a chronic subdural hemorrhage. Bleeding may develop over a period of weeks to months.
This form of bleeding is much more common in older people. The head trauma that causes chronic subdural hemorrhage is often minor. Many of those affected cannot recall a head injury.
Symptoms
Acute subdural hemorrhage usually develops after severe head trauma. Injuries that result in this condition are typically forceful enough to cause a temporary loss of consciousness.
Usually, in the minutes to hours after head injury, the person recovers consciousness. Then, the person gradually loses consciousness again, this time from subdural bleeding.
Other common symptoms of an acute subdural hemorrhage include
- severe headache
- weakness on one side of the body
- seizures
- changes in vision or speech.
Chronic subdural hemorrhages produce more subtle symptoms. These symptoms may continue for more than a month before the diagnosis is recognized.
These symptoms include
- mild headache
- nausea or vomiting
- change in personality
- memory loss
- loss of balance or difficulty walking
- double vision
- weakness, numbness, or tingling in arms or legs.
The symptoms caused by chronic subdural hemorrhage can mimic other common conditions. For example, they may resemble strokes and brain tumors. Occasionally, the gradual memory loss and personality changes can be mistaken for dementia.
Diagnosis
All head injuries should be evaluated promptly by a physician. This is especially true if there has been any loss of consciousness.
A doctor usually will want to know
- how the injury occurred
- what symptoms developed
- whether there have been head injuries in the past (repeat injuries are more likely to cause serious damage)
- whether the person has other medical problems
- what medications the person is taking
- whether the person has been drinking alcohol or using drugs
- whether there are symptoms of other injuries (neck pain, shortness of breath, etc.).
The doctor will perform a thorough physical and neurological exam. He or she will check
- blood pressure and pulse
- vision and the way the eyes respond to light
- reflexes and balance
- ability to answer questions and remember things.
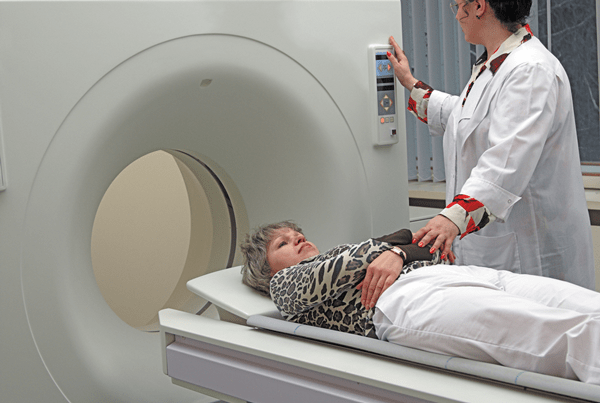
If the doctor suspects bleeding in the head, he or she will usually order a computer tomography (CT) scan. A CT scan is the fastest way to determine the location and amount of bleeding. It can also identify any injuries to the brain, skull, or neck. If needed, a brain MRI might also be performed.
|
|
A doctor may suspect a chronic subdural hemorrhage if an older patient develops new neurological symptoms. This is more likely if there has been a fall or minor trauma to the head.
Expected duration
An acute subdural hemorrhage develops over minutes to hours. If not diagnosed and treated promptly, it can cause severe brain injury and sometimes death.
A chronic subdural hemorrhage develops over many days to weeks. The symptoms may be subtle and develop so slowly that the person and family are not alarmed.
As is the case with any brain injury, symptoms can be slow to go away after treatment. Some symptoms may be permanent.
Occasionally, a subdural hematoma is small enough that you may not need surgery to remove the blood. The blood will be reabsorbed gradually by the body. This process may require a few months. But it is sometimes the safest treatment plan.
Prevention
Accidents, including head injuries, are the leading cause of death in young people. Many of these accidents are related to drugs and alcohol. Many others could be prevented with simple precautions or safety equipment.
To help prevent head injuries:
- If you drink alcohol, drink in moderation. Never drive after drinking or using drugs.
- If your job involves working high above the ground, use approved safety equipment to prevent accidental falls.
- Never work in a high place if you
- feel lightheaded or unsteady
- have been drinking alcohol
- are taking medication that can make you dizzy or affect your balance.
- Have your vision checked regularly. Poor vision can increase your risk of falls and other types of accidents.
- If you are an older adult, clear your home of hazards that could cause you to trip and fall. These include throw rugs and extension cords.
- If you feel unsteady on your feet, consider using a cane or walker.
- If you play a contact sport such as football and you experience a significant head injury, allow adequate time for healing before you start playing again. After a head injury, complete healing can take up to 15 days. This is true even if symptoms go away much sooner. A repeated head injury during this fragile repair period is likely to result in more bleeding. This is called second impact syndrome.
"Blood-thinning" medications increase your risk of bleeding within the head. Examples include
- aspirin
- clopidogrel (Plavix) and prasugrel (Effient)
- direct-acting anticoagulants, such as apixaban (Eliquis) and rivaroxaban (Xarelto)
- heparin
- warfarin (Coumadin).
Treatment
An acute subdural hemorrhage requires immediate medical attention. In most cases, emergency surgery must be done to drain the hematoma and to control bleeding.
In contrast, only some chronic subdural hemorrhages require emergency surgery. Most physicians will recommend surgery for larger hemorrhages and those that cause neurological symptoms. However, treatment with bed rest, medications, and observation may be reasonable in some cases. This may be the case for smaller hematomas that cause minimal or no symptoms.
People who develop a subdural hemorrhage are at risk of seizures. Seizures may occur even after the hematoma has been treated.
When to call a professional
Call for emergency assistance if you find someone unconscious at an accident scene.
Also seek immediate attention if someone with a head injury experiences
- drowsiness or a decrease in alertness
- nausea or vomiting
- confusion or amnesia
- difficulty walking or poor coordination
- slurred speech
- double vision
- irrational or aggressive behavior
- seizures
- numbness or paralysis in any part of the body.
Even if a head injury appears minor, with mild symptoms, certain people are at high risk of serious bleeding. Call a doctor or go to an emergency room immediately if a person with head injury also:
- is elderly
- takes medications to prevent unwanted blood clots
- has a bleeding disorder
- has a history of heavy alcohol use.
Prognosis
The outlook for acute subdural hemorrhages generally is guarded and some people die even with prompt surgery. Usually there are injuries to other parts of the brain from the trauma. This tends to be true regardless of the size of the hematoma. Many of those who survive may be left with permanent neurological problems.
The prognosis for an acute or chronic subdural hematoma is best in people who:
- don't lose consciousness or are unconscious for a short period of time
- are awake and alert
- have no or few neurological symptoms when evaluated by a doctor
- are younger than age 50
- do not have alcohol use disorder
- do not have other associated brain injuries
- receive prompt medical attention.
The prognosis for chronic subdural hemorrhage is quite favorable. Most people are able to resume their level of previous functioning.
Additional info
National Institute of Neurological Disorders and Stroke
https://www.ninds.nih.gov/
Brain Injury Association of America
https://www.biausa.org/
Learn more about Subdural hematoma
Treatment options
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.