Alogliptin / pioglitazone Side Effects
Medically reviewed by Drugs.com. Last updated on Jan 15, 2024.
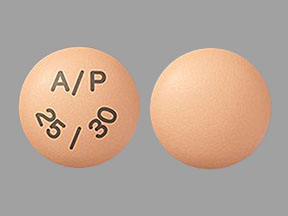
Applies to alogliptin / pioglitazone: oral tablet.
Warning
Oral route (Tablet)
Congestive Heart FailureThiazolidinediones, including pioglitazone, cause or exacerbate congestive heart failure in some patients.After initiation of alogliptin/pioglitazone and after dose increases, monitor patients carefully for signs and symptoms of heart failure (eg, excessive, rapid weight gain, dyspnea, and/or edema). If heart failure develops, it should be managed according to current standards of care and discontinuation or dose reduction of pioglitazone in alogliptin / pioglitazone must be considered.Alogliptin / pioglitazone is not recommended in patients with symptomatic heart failure.Initiation of alogliptin / pioglitazone in patients with established New York Heart Association (NYHA) Class III or IV heart failure is contraindicated.
Serious side effects
Along with its needed effects, alogliptin / pioglitazone may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking alogliptin / pioglitazone:
More common
- Anxiety
- blurred vision
- chest pain
- chills
- cold sweats
- confusion
- cool, pale skin
- decreased urine output
- depression
- dilated neck veins
- dizziness
- extreme tiredness or weakness
- fast heartbeat
- headache
- increased hunger
- irregular breathing
- irregular heartbeat
- nausea
- nightmares
- seizures
- shakiness
- slurred speech
- swelling of the face, fingers, feet, or lower legs
- tightness in the chest
- troubled breathing
- unusual tiredness or weakness
- weight gain
Rare
- Blistering, peeling, or loosening of the skin
- bloating
- blood in the urine
- constipation
- cough
- darkened urine
- diarrhea
- difficulty with swallowing
- feeling of discomfort
- fever
- frequent, strong, or increased urge to urinate
- hives, itching, or rash
- indigestion
- inflammation of the joints
- joint or muscle pain
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- loss of appetite
- muscle aches
- pain in the back, lower abdomen, or stomach
- painful urination
- pains in the stomach, side, or abdomen, possibly radiating to the back
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- red skin lesions, often with a purple center
- red, irritated eyes
- sore throat
- sores, ulcers, or white spots in the mouth or on the lips
- swollen lymph glands
- vomiting
- yellow eyes or skin
Incidence not known
- Change in vision
- general feeling of tiredness or weakness
- light-colored stools
- severe joint pain
- stomach pain, continuing
Other side effects
Some side effects of alogliptin / pioglitazone may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
- Back pain
- body aches or pain
- ear congestion
- loss of voice
- sneezing
- stuffy or runny nose
For Healthcare Professionals
Applies to alogliptin / pioglitazone: oral tablet.
General
The most common side effect reported include nasopharyngitis, back pain and upper respiratory tract infection.[Ref]
Cardiovascular
Alogliptin:
Common (1% to 10%): Hypertension, Congestive heart failure (CHF) hospitalization
Pioglitazone:
Common (1% to 10%): CHF hospitalization
Postmarketing reports: CHF with and without known heart disease and with and without concomitant insulin[Ref]
Alogliptin:
In the EXAMINE trial which enrolled patients with type 2 diabetes and recent acute coronary syndrome, more patients (3.9%; n=106) on alogliptin therapy were hospitalized for congestive heart failure (CHF) compare with placebo (3.3%; n=89).
Pioglitazone:
In the PROactive trial, a study in 5238 patients with type 2 diabetes and a history of macrovascular disease who were force-uptitrated to pioglitazone 45 mg once a day or given placebo in addition to standard of care, edema occurred in 27.3% of patients treated with pioglitazone (n=2605) compared with 15.9% of placebo (n=2633) patients. Treatment-emergent adverse events leading to at least 1 hospitalized congestive heart failure event occurred in 5.7% of patients receiving pioglitazone and 4.1% of patients receiving placebo.
The primary objective of the 3-year PROactive trial was to examine the effect of pioglitazone on mortality and macrovascular morbidity in high-risk patients. No statistically significant difference between pioglitazone and placebo/standard care were observed for time to the first occurrence of their first event (all-cause mortality, nonfatal myocardial infarction (MI) including silent MI, stroke, acute coronary syndrome, cardiac intervention including coronary artery bypass grafting or percutaneous intervention, major leg amputation above the ankle, and bypass surgery or revascularization in the leg). A total of 514 patients receiving pioglitazone experienced at least 1 event compared with 572 patients receiving placebo/standard care.
Pioglitazone is associated with edema (peripheral, generalized, and pitting edema and fluid retention) when used alone or when used in combination therapy. In pioglitazone monotherapy trials, edema occurred in 2.5% (n=81), 4.7% (n=275), and 6.5% (n=169) of patients receiving 15 mg, 30 mg, and 45 mg of pioglitazone daily for 16 to 26 weeks. Pioglitazone in combination with a sulfonylurea for 16 to 24 weeks resulted in edema in 1.6% (n=184), 11.3% (n=540), and 23.1% (n=351) of patients receiving 15 mg, 30 mg, and 45 mg of pioglitazone daily, respectively. In a study in patients with NYHA class II or III heart failure the percentage of patients experiencing CHF progression during the study was 13.4% and 8.2% in patients receiving pioglitazone (n=262) and glyburide (n=256), respectively.
Postmarketing reports of congestive heart failure have been received in patients treated with pioglitazone. Reports have been received from patients both with and without a history of a known history of heart disease and both with and without concomitant insulin use.[Ref]
Endocrine
Alogliptin-Pioglitazone:
Common (1% to 10%): Hypoglycemia (up to 4.5%)
Alogliptin:
Common (1% to 10%): Hypoglycemia (up to 5.4%)
Pioglitazone:
Common (1% to 10%): Hypoglycemia (up to 4.7%)[Ref]
Gastrointestinal
Alogliptin:
Uncommon (0.1% to 1%): Pancreatitis (0.2%)
Postmarketing reports: Acute pancreatitis[Ref]
Acute pancreatitis was reported in 0.2% (n=6) of patients treated with alogliptin 25 mg and less than 0.1% (n=2) of patients treated with active comparator or placebo in alogliptin clinical trials. IN the EXAMINE trial, a cardiovascular (CV) outcomes trial in patients with type 2 diabetes and high CV risk, acute pancreatitis was reported in 0.4% (n=10) of patients treated with alogliptin and 0.3% (n=7) of patients receiving placebo.[Ref]
Hematologic
Pioglitazone:
Uncommon (0.1% to 1%): Elevated ALT (0.3%)
Frequency not reported: Decreased hemoglobin and hematocrit[Ref]
Hepatic
Alogliptin:
ALT elevations greater than 3 times upper limit of normal (3 x ULN) occurred in 1.3% of alogliptin treated patients compared with 1.7% of those receiving comparator or placebo during clinical trials. In the EXAMINE trial, a trial in patients with type 2 diabetes and high cardiovascular risk, ALT increases to 3 x ULN occurred in 2.4% of patients receiving alogliptin (compared with 1.8% of placebo patients).
Pioglitazone:
Hepatotoxic effects were not observed in pioglitazone clinical trials, however, postmarketing cases of fatal and nonfatal hepatic failure have been reported.[Ref]
Alogliptin:
Postmarketing reports: Hepatic enzyme elevations, fulminant hepatic failure
Pioglitazone:
Uncommon (0.1% to 1%): Elevated serum alanine aminotransferase (ALT) (0.3%)
Postmarketing reports: Fatal and non-fatal hepatic fail[Ref]
Hypersensitivity
Alogliptin:
Uncommon (0.1% to 1%): Hypersensitivity reactions (0.6%)
Postmarketing reports: Anaphylaxis, angioedema, rash, urticaria, severe cutaneous adverse reactions (Stevens-Johnson syndrome)[Ref]
Metabolic
Pioglitazone:
Frequency not reported: Weight gain, edema
Postmarketing reports: Rapid increased in weight[Ref]
Musculoskeletal
Alogliptin-Pioglitazone:
Common (1% to 10%): Back pain (4.2%)
Alogliptin:
Common (1% to 10%): Back pain (2%)
Frequency not reported: Arthralgia
Pioglitazone:
Common (1% to 10%): Myalgia (5.4%), back pain (3.4%)
Uncommon (0.1% to 1%): Elevation in serum creatine phosphokinase (CPK) (0.2%)[Ref]
Alogliptin: Between October 2006 and December 2013, thirty-three cases of severe arthralgia have been reported to the FDA Adverse Event Reporting System Database. Each case involved the use of 1 or more dipeptidyl peptidase-4 (DPP-4) inhibitor. In all cases, substantial reduction in prior activity level was reported, 10 patients were hospitalized due to disabling joint pain. In 22 cases, symptoms appeared within 1 month of starting therapy, in 23 cases symptoms resolved less than 1 month after discontinuation. A positive rechallenge was reported in 8 cases, with 6 cases involving use of a different DPP-4 inhibitor. Sitagliptin had the greatest number of cases reported (n=28) followed by saxagliptin (n=5), linagliptin (n=2), alogliptin (n=1), and vildagliptin (n=2).[Ref]
Nervous system
Alogliptin:
Common (1% to 10%): Headache (4.2%)
Pioglitazone:
Common (1% to 10%): Headache (9.1%)[Ref]
Ocular
Pioglitazone:
Postmarketing reports: Macular edema[Ref]
Oncologic
Pioglitazone:
Uncommon (0.1% to 1%): Bladder cancer (up to 0.44%)[Ref]
The US FDA has released results of its review of pioglitazone and bladder cancer and concluded that the data suggests use of this drug may be linked to an increase risk of bladder cancer. A 10-year prospective cohort study in diabetic patients performed by the manufacturer (n=158,918 never users; n=34,181 ever users) identified 1075 newly diagnosed cases of bladder cancer in never users and 186 cases in ever users. The fully adjusted hazard ratio (HR) showed pioglitazone use was not associated with an increased risk (HR 1.06 (95% confidence interval 0.89 to 1.26). And while a modest trend towards higher risk with increasing duration was observed, this trend was not statistically significant. Compared to the interim 5-year results, the 10-year results found weaker associations that were not statistically significant. However, there are studies that have shown a statistically significant association between exposure to this drug and bladder cancer and an association between cumulative dose or cumulative duration of exposure and bladder cancer. Overall, this drug may be associated with an increase in the risk of urinary bladder tumors, however there is insufficient data to determine whether this drug is a tumor promoter for urinary bladder tumors.[Ref]
Respiratory
Alogliptin-Pioglitazone:
Very common (10% or more): Nasopharyngitis (4.9%), upper respiratory tract infection (4.1%)
Alogliptin:
Common (1% to 10%): Influenza (5.5%), nasopharyngitis (4.7%), upper respiratory tract infection (4.3%)
Pioglitazone:
Common (1% to 10%): Upper respiratory tract infection (up to 13.2%), sinusitis (6.3%), nasopharyngitis (3.9%)[Ref]
Dermatologic
Dipeptidyl peptidase-4 inhibitors:
Postmarketing reports: Bullous pemphigoid
Postmarketing reports of bullous pemphigoid requiring hospitalization have been reported with dipeptidyl peptidase-4 (DPP-4) inhibitors use. These case typically recovered with topical or systemic immunosuppressive treatment and discontinuation of DPP-4 inhibitor.
More about alogliptin / pioglitazone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Dosage information
- During pregnancy
- Drug class: antidiabetic combinations
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
References
1. (2013) "Product Information. Oseni (alogliptin-pioglitazone)." Takeda Pharmaceuticals America
2. US Food and Drug Administration (2015) FDA Drug Safety Communication: FDA warns that DPP-4 inhibitors for type 2 diabetes may cause severe joint pain. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM460038.pdf
3. US Food and Drug Administration (2016) Updated FDA review concludes that use of type 2 diabetes medicine pioglitazone may be linked to an increased risk of bladder cancer. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM532691.pdf
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.