Pancreatitis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is pancreatitis?
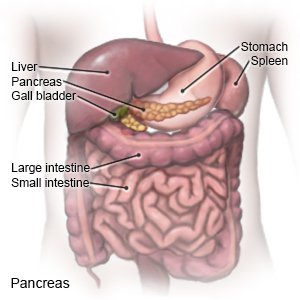
Pancreatitis is inflammation of your pancreas. The pancreas is an organ that makes insulin. It also makes enzymes (digestive juices) that help your body digest food. Pancreatitis may be an acute (short-term) problem that happens only once. It may become a chronic (long-term) problem that comes and goes over time.
 |
What causes pancreatitis?
Pancreatitis is usually caused by alcohol or gallstones. Less common causes are certain medicines, an injury to the abdomen, some procedures, and infections. High levels of triglycerides (fats) and calcium may also cause pancreatitis.
What are the signs and symptoms of pancreatitis?
- Severe burning, stabbing, or aching pain that starts in the top of your abdomen and spreads to your back
- Fever
- Nausea and vomiting
- Abdomen that is tender to the touch
- Weight loss without trying
Related medications
How is pancreatitis diagnosed?
Your healthcare provider will examine you and ask about your symptoms. You may need any of the following:
- Blood tests may show infection, pancreas function, or provide information about your overall health.
- An x-ray, ultrasound, MRI, or CT may show the cause of your pancreatitis and help healthcare providers plan your treatment. You may be given contrast liquid to help your pancreas show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious harm. Tell the healthcare provider if you have any metal in or on your body.
- Magnetic retrograde cholangiopancreatography (MRCP) uses magnetic waves to find gallstones, masses, or other problems.
- Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure used to find stones, tumors, or narrowed bile ducts. A long tube with a camera on the end is passed down your throat and into your stomach and abdomen. ERCP may also be used to open ducts blocked by pancreatic duct stones.
How is pancreatitis treated?
Treatment depends on the cause of your pancreatitis. You may need to stay in the hospital for treatment and more tests.
- Medicines:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics may be given to treat a bacterial infection.
- Surgery may be needed to open or widen blocked bile ducts or drain fluid from your pancreas. Your gallbladder may need to be removed if gallstones are causing your pancreatitis.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage my symptoms?
- Rest when you feel it is needed. Slowly start to do more each day. Return to your usual activities as directed.
- Do not drink any alcohol. If you need help to stop drinking, contact the following organization:
- Alcoholics Anonymous
Web Address: http://www.aa.org
- Alcoholics Anonymous
- Ask your healthcare provider or dietitian about the best foods to eat. You may need to eat foods that are low in fat if you have chronic pancreatitis.

- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
When should I call my doctor?
- You have severe pain in your abdomen and you are vomiting.
- You have a fever.
- You continue to lose weight without trying.
- Your skin or the whites of your eyes turn yellow.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Pancreatitis
Treatment options
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
