Epkinly Prescribing Information
Package insert / product label
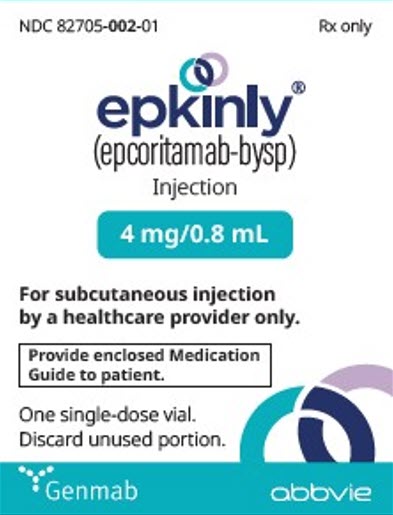
Generic name: epcoritamab-bysp
Dosage form: injection, solution
Drug class: Bispecific T-cell engagers (BiTE)
J Code (medical billing code): J9321 (0.16 mg, injection)
Medically reviewed by Drugs.com. Last updated on Jul 10, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
- Medication Guide
Highlights of Prescribing Information
EPKINLY™ (epcoritamab-bysp) injection, for subcutaneous use
Initial U.S. Approval: 2023
WARNING: CYTOKINE RELEASE SYNDROME and IMMUNE EFFECTOR CELL-ASSOCIATED NEUROTOXICITY SYNDROME
See full prescribing information for complete boxed warning.
Cytokine release syndrome (CRS), including serious or life-threatening reactions, can occur in patients receiving EPKINLY. Initiate treatment with the EPKINLY step-up dosage schedule to reduce the incidence and severity of CRS. Withhold EPKINLY until CRS resolves or permanently discontinue based on severity. (2.1, 2.2, 2.6, 5.1)
Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), including life-threatening and fatal reactions, can occur with EPKINLY. Monitor patients for neurological signs or symptoms of ICANS during treatment. Withhold EPKINLY until ICANS resolves or permanently discontinue based on severity. (2.1, 2.2, 2.6, 5.2)
Recent Major Changes
Indications and Usage for Epkinly
EPKINLY is a bispecific CD20-directed CD3 T-cell engager indicated for the treatment of:
Diffuse Large B-cell Lymphoma and High-grade B-cell Lymphoma
- adult patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL), not otherwise specified, including DLBCL arising from indolent lymphoma, and high-grade B-cell lymphoma after two or more lines of systemic therapy. (1.1)
Follicular Lymphoma
- adult patients with relapsed or refractory follicular lymphoma (FL) after two or more lines of systemic therapy. (1.2)
These indications are approved under accelerated approval based on response rate and durability of response. Continued approval for these indications may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
Epkinly Dosage and Administration
DLBCL and High-grade B-cell Lymphoma
| Cycle of treatment* | Day of treatment | Dose of EPKINLY | |
|---|---|---|---|
|
|||
| Cycle 1 | 1 | Step-up dose 1 | 0.16 mg |
| 8 | Step-up dose 2 | 0.8 mg | |
| 15 | First full dose | 48 mg | |
| 22 | 48 mg | ||
| Cycles 2 and 3 | 1, 8, 15 and 22 | 48 mg | |
| Cycles 4 to 9 | 1 and 15 | 48 mg | |
| Cycle 10 and beyond | 1 | 48 mg | |
Follicular Lymphoma
| Cycle of treatment* | Day of treatment | Dose of EPKINLY | |
|---|---|---|---|
|
|||
| Cycle 1 | 1 | Step-up dose 1 | 0.16 mg |
| 8 | Step-up dose 2 | 0.8 mg | |
| 15 | Step-up dose 3 | 3 mg | |
| 22 | First full dose | 48 mg | |
| Cycles 2 and 3 | 1, 8, 15 and 22 | 48 mg | |
| Cycles 4 to 9 | 1 and 15 | 48 mg | |
| Cycle 10 and beyond | 1 | 48 mg | |
- Monitor all patients for signs and symptoms of CRS and ICANS. (2.1)
- Patients with DLBCL or high-grade B-cell lymphoma should be hospitalized for 24 hours after administration of the Cycle 1 Day 15 dosage of 48 mg. (2.1)
- Administer premedications, post-medications, and prophylaxis as recommended. (2.4, 2.5)
- Dosages of EPKINLY 0.16 mg and 0.8 mg require dilution prior to administration. (2.7, 2.8)
- See Full Prescribing Information for instructions on preparation and administration. (2.7, 2.8, 2.9, 2.10)
Dosage Forms and Strengths
Contraindications
None. (4)
Warnings and Precautions
- Infections: Can cause serious or fatal infections. Monitor patients for signs or symptoms of infection, including opportunistic infections, and treat appropriately. (5.3)
- Cytopenias: Monitor complete blood cell counts during treatment. (5.4)
- Embryo-Fetal Toxicity: May cause fetal harm. Advise females of reproductive potential of the potential risk to the fetus and to use effective contraception. (5.5, 8.1, 8.3)
Adverse Reactions/Side Effects
LBCL: The most common (≥ 20%) adverse reactions are cytokine release syndrome, fatigue, musculoskeletal pain, injection site reactions, pyrexia, abdominal pain, nausea, and diarrhea. The most common Grade 3 to 4 laboratory abnormalities (≥ 10%) are decreased lymphocyte count, decreased neutrophil count, decreased white blood cell count, decreased hemoglobin, and decreased platelets. (6.1)
FL: The most common (≥ 20%) adverse reactions are injection site reactions, cytokine release syndrome, COVID-19, fatigue, upper respiratory tract infection, musculoskeletal pain, rash, diarrhea, pyrexia, cough, and headache. The most common Grade 3 to 4 laboratory abnormalities (≥ 10%) are decreased lymphocyte count, decreased neutrophil count, decreased white blood cell count, and decreased hemoglobin. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Genmab US, Inc. at 1-855-4GENMAB (1-855-443-6622) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2024
Related/similar drugs
Rituxan, Breyanzi, Truxima, Kymriah, Yescarta, Monjuvi, Columvi
Full Prescribing Information
WARNING: CYTOKINE RELEASE SYNDROME AND IMMUNE EFFECTOR CELL-ASSOCIATED NEUROTOXICITY SYNDROME
Cytokine release syndrome (CRS), including serious or life-threatening reactions, can occur in patients receiving EPKINLY. Initiate treatment with the EPKINLY step-up dosage schedule to reduce the incidence and severity of CRS. Withhold EPKINLY until CRS resolves or permanently discontinue based on severity [see Dosage and Administration (2.1, 2.2, 2.6) and Warnings and Precautions (5.1)].
Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), including life-threatening and fatal reactions, can occur with EPKINLY. Monitor patients for neurological signs or symptoms of ICANS during treatment. Withhold EPKINLY until ICANS resolves or permanently discontinue based on severity [see Dosage and Administration (2.1, 2.2, 2.6) and Warnings and Precautions (5.2)].
1. Indications and Usage for Epkinly
1.1 DLBCL and High-grade B-cell Lymphoma
EPKINLY is indicated for the treatment of adult patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL), not otherwise specified, including DLBCL arising from indolent lymphoma, and high-grade B-cell lymphoma after two or more lines of systemic therapy.
This indication is approved under accelerated approval based on response rate and durability of response [see Clinical Studies (14.1)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
1.2 Follicular Lymphoma
EPKINLY is indicated for the treatment of adult patients with relapsed or refractory follicular lymphoma (FL) after two or more lines of systemic therapy.
This indication is approved under accelerated approval based on response rate and durability of response [see Clinical Studies (14.2)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).
2. Epkinly Dosage and Administration
2.1 Important Dosing Information
-
Certain doses of EPKINLY require dilution prior to administration. There are 2 available methods to prepare diluted EPKINLY:
- Empty sterile vial method as described in subsection 2.7 [see Dosage and Administration (2.7)], or
- Sterile syringe method as described in subsection 2.8 [see Dosage and Administration (2.8)].
- Preparation of 3 mg and 48 mg EPKINLY doses do not require dilution. For preparation, refer to subsection 2.9 [see Dosage and Administration (2.9)].
- Administer EPKINLY to well-hydrated patients.
- Premedicate before each dose in Cycle 1 [see Dosage and Administration (2.4)].
- EPKINLY should only be administered by a qualified healthcare professional with appropriate medical support to manage severe reactions such as cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) [see Warnings and Precautions (5.1, 5.2)].
- Administer EPKINLY subcutaneously according to the step-up dosage schedule in Table 1 for patients with DLBCL or high-grade B-cell Lymphoma, or Table 2 for patients with FL to reduce the incidence and severity of CRS.
-
Due to the risk of CRS and ICANS, monitor all patients for signs and symptoms [see Dosage and Administration (2.6)].
-
For Patients with DLBCL or High-grade B-cell Lymphoma:
Patients should be hospitalized for 24 hours after administration of the Cycle 1 Day 15 dosage of 48 mg [see Dosage and Administration (2.2) and Warnings and Precautions (5.1, 5.2)].
-
For Patients with DLBCL or High-grade B-cell Lymphoma:
2.2 Recommended Dosage
EPKINLY is for subcutaneous injection only.
Administer EPKINLY in 28-day cycles until disease progression or unacceptable toxicity.
| Indication | Cycle of treatment* | Day of treatment | Dose of EPKINLY | |
|---|---|---|---|---|
|
||||
| DLBCL or High-grade B-cell Lymphoma | Cycle 1 | 1 | Step-up dose 1 | 0.16 mg |
| 8 | Step-up dose 2 | 0.8 mg | ||
| 15 | First full dose | 48 mg | ||
| 22 | 48 mg | |||
| Cycles 2 and 3 | 1, 8, 15 and 22 | 48 mg | ||
| Cycles 4 to 9 | 1 and 15 | 48 mg | ||
| Cycle 10 and beyond | 1 | 48 mg | ||
| Indication | Cycle of treatment* | Day of treatment | Dose of EPKINLY | |
|---|---|---|---|---|
|
||||
| Follicular Lymphoma | Cycle 1 | 1 | Step-up dose 1 | 0.16 mg |
| 8 | Step-up dose 2 | 0.8 mg | ||
| 15 | Step-up dose 3 | 3 mg | ||
| 22 | First full dose | 48 mg | ||
| Cycles 2 and 3 | 1, 8, 15 and 22 | 48 mg | ||
| Cycles 4 to 9 | 1 and 15 | 48 mg | ||
| Cycle 10 and beyond | 1 | 48 mg | ||
2.3 Restarting EPKINLY after Dosage Delay
If a dose of EPKINLY is delayed, restart therapy based on the recommendations made in Table 3 for patients with DLBCL or high-grade B-cell lymphoma, or Table 4 for patients with FL [see Dosage and Administration (2.2)].
| Last Dose Administered | Time Since the Last Dose Administered | Action for Next Dose(s)* |
|---|---|---|
|
||
| 0.16 mg (e.g., on Cycle 1 Day 1) | More than 8 days | Repeat Cycle 1 schedule starting at step-up dose 1 (0.16 mg). Following the repeat of Cycle 1 schedule, resume the planned treatment schedule. |
| 0.8 mg (e.g., on Cycle 1 Day 8) | 14 days or less | Administer 48 mg, then resume the planned treatment schedule. |
| More than 14 days | Repeat Cycle 1 schedule starting at step-up dose 1 (0.16 mg). Following the repeat of Cycle 1 schedule, resume the planned treatment schedule. | |
| 48 mg (e.g., on Cycle 1 Day 15 onwards) | 6 weeks or less | Administer 48 mg, then resume the planned treatment schedule. |
| More than 6 weeks | Repeat Cycle 1 schedule starting at step-up dose 1 (0.16 mg). Following the repeat of Cycle 1 schedule, resume the planned treatment schedule. | |
| Last Dose Administered | Time Since the Last Dose Administered | Action for Next Dose(s)* |
|---|---|---|
|
||
| 0.16 mg (e.g., on Cycle 1 Day 1) | More than 8 days | Repeat Cycle 1 schedule starting at step-up dose 1 (0.16 mg). Following the repeat of Cycle 1 schedule, resume the planned treatment schedule. |
| 0.8 mg (e.g., on Cycle 1 Day 8) | More than 8 days | Repeat Cycle 1 schedule starting at step-up dose 1 (0.16 mg). Following the repeat of Cycle 1 schedule, resume the planned treatment schedule. |
| 3 mg (e.g., on Cycle 1 Day 15) | 14 days or less | Administer 48 mg, then resume the planned treatment schedule. |
| More than 14 days | Repeat Cycle 1 schedule starting at step-up dose 1 (0.16 mg). Following the repeat of Cycle 1 schedule, resume the planned treatment schedule. | |
| 48 mg (e.g., on Cycle 1 Day 22 onwards) | 6 weeks or less | Administer 48 mg, then resume the planned treatment schedule. |
| More than 6 weeks | Repeat Cycle 1 schedule starting at step-up dose 1 (0.16 mg). Following the repeat of Cycle 1 schedule, resume the planned treatment schedule. | |
2.4 Recommended Pre- and Post-Administration Medications
Administer pre- and post-administration medications as outlined in Table 5 to reduce the risk of CRS [see Warnings and Precautions (5.1)].
| Cycle | Patients requiring medication | Medication | Administration |
|---|---|---|---|
| Cycle 1 | All patients |
|
|
|
|
||
| Cycle 2+ | Patients who experienced Grade 2 or 3† CRS with previous dose |
|
|
2.5 Recommended Prophylaxis
2.6 Dosage Modifications and Management of Adverse Reactions
See Tables 6 and 7 for recommended actions for adverse reactions of CRS and ICANS, respectively. See Table 8 for recommended actions for other adverse reactions following administration of EPKINLY.
Cytokine Release Syndrome (CRS)
Identify CRS based on clinical presentation [see Warnings and Precautions (5.1)]. Evaluate for and treat other causes of fever, hypotension, and hypoxia.
If CRS is suspected, withhold EPKINLY until CRS resolves. Manage according to the recommendations in Table 6 and consider further management per current practice guidelines. Administer supportive therapy for CRS, which may include intensive care for severe or life-threatening CRS.
| Grade* | Presenting Symptoms | Actions |
|---|---|---|
|
||
| Grade 1 | Temperature ≥ 100.4°F (38°C)† |
|
| Grade 2 | Temperature ≥ 100.4°F (38°C)† with: Hypotension not requiring vasopressors and/or Hypoxia requiring low-flow oxygen§ by nasal cannula or blow-by. | |
| Grade 3 | Temperature ≥ 100.4°F (38°C)† with: Hypotension requiring a vasopressor (with or without vasopressin) and/or Hypoxia requiring high-flow oxygen§ by nasal cannula, face mask, non-rebreather mask, or Venturi mask. | |
Recurrent Grade 3 CRS
|
||
| Grade 4 | Temperature ≥ 100.4°F (38°C)† with: Hypotension requiring multiple vasopressors (excluding vasopressin) and/or Hypoxia requiring oxygen by positive pressure (e.g., CPAP, BiPAP, intubation and mechanical ventilation). |
|
Immune Effector Cell-Associated Neurological Toxicity Syndrome (ICANS)
Monitor patients for signs and symptoms of ICANS [see Warnings and Precautions (5.2)]. At the first sign of ICANS, withhold EPKINLY and consider neurology evaluation. Rule out other causes of neurologic symptoms. Provide supportive therapy, which may include intensive care, for ICANS [see Warnings and Precautions (5.2)]. Manage ICANS according to the recommendations in Table 7 and consider further management per current practice guidelines.
| Grade* | Presenting Symptoms† | Actions |
|---|---|---|
|
||
| Grade 1 | ICE score 7-9‡, Or depressed level of consciousness§: awakens spontaneously. |
|
| Grade 2 | ICE score 3-6‡, Or depressed level of consciousness§: awakens to voice. |
|
| Grade 3 | ICE score 0-2‡, Or depressed level of consciousness§: awakens only to tactile stimulus, Or seizures,§ either:
| First Occurrence of Grade 3 ICANS
|
Recurrent Grade 3 ICANS
|
||
| Grade 4 | ICE score 0‡, Or depressed level of consciousness§: either:
|
|
| Adverse Reaction* | Severity* | Action |
|---|---|---|
|
||
| Infections [see Warnings and Precautions (5.3)] | Grades 1-4 |
|
| Neutropenia [see Warnings and Precautions (5.4)] | Absolute neutrophil count less than 0.5 × 109/L |
|
| Thrombocytopenia [see Warnings and Precautions (5.4)] | Platelet count less than 50 × 109/L |
|
| Other Adverse Reactions [see Adverse Reactions (6.1)] | Grade 3 or higher |
|
2.7 Preparation of Diluted EPKINLY using the Vial Method
Read this entire section carefully before preparation of EPKINLY. Certain doses of EPKINLY require dilution prior to administration. Follow the preparation instructions provided below, as improper preparation may lead to improper dose. This section describes preparation of diluted EPKINLY using empty sterile vial method. For preparation using sterile syringe method, see subsection 2.8 [see Dosage and Administration (2.8)].
EPKINLY is prepared and administered by a healthcare provider as a subcutaneous injection. The administration of EPKINLY takes place over the course of 28-day cycles, following the step-up dosage schedule in Section 2.2.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Use aseptic technique to prepare EPKINLY. Filtration of the diluted solution is not required.
0.16 mg Dose Preparation Instructions (2 dilutions required) – Empty Sterile Vial Method
Use an appropriately sized syringe, vial, and needle for each transfer step.
1. Prepare EPKINLY vial
|
2. Perform first dilution
|
3. Perform second dilution
|
4. Withdraw dose
|
5. Label syringe
|
Discard the vial containing unused EPKINLY.
0.8 mg Dose Preparation Instructions (1 dilution required) – Empty Sterile Vial Method
Use an appropriately sized syringe, vial, and needle for each transfer step.
1. Prepare EPKINLY vial
|
2. Perform dilution
|
3. Withdraw dose
|
4. Label syringe
|
Discard the vial containing unused EPKINLY.
2.8 Preparation of Diluted EPKINLY using the Syringe Method
Read this entire section carefully before preparation of EPKINLY. Certain doses of EPKINLY require dilution prior to administration. Follow the preparation instructions provided below, as improper preparation may lead to improper dose.
EPKINLY is prepared and administered by a healthcare provider as a subcutaneous injection. The administration of EPKINLY takes place over the course of 28-day cycles, following the step-up dosage schedule in Section 2.2.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Use aseptic technique to prepare EPKINLY. Filtration of the diluted solution is not required.
0.16 mg Dose Preparation Instructions (2 dilutions required) – Sterile Syringe Method
Use an appropriately sized syringe and needle for each transfer step.
1. Prepare EPKINLY vial
|
2. Perform first dilution
|
3. Perform second dilution
|
4. Withdraw dose
|
5. Label syringe
|
Discard the vial containing unused EPKINLY.
0.8 mg Dose Preparation Instructions (1 dilution required) – Sterile Syringe Method
Use an appropriately sized syringe and needle for each transfer step.
1. Prepare EPKINLY vial
|
2. Perform first dilution
|
3. Withdraw dose
|
4. Label syringe
|
Discard the vial containing unused EPKINLY.
2.9 Preparation of 3 mg and 48 mg EPKINLY Doses
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Use aseptic technique to prepare EPKINLY.
3 mg Dose Preparation Instructions (No dilution required)
EPKINLY 3 mg dose is required for patients with FL only [see Dosage and Administration (2.2)].
1. Prepare EPKINLY vial
|
| DO NOT invert, vortex, or vigorously shake the vial. |
2. Withdraw dose
|
3. Label syringe
|
Discard the vial containing unused EPKINLY.
48 mg Dose Preparation Instructions (No dilution required)
EPKINLY 48 mg/0.8 mL vial is supplied as ready-to-use solution that does not need dilution prior to administration.
1. Prepare EPKINLY vial
|
| DO NOT invert, vortex, or vigorously shake the vial. |
2. Withdraw dose
|
3. Label syringe
|
Discard the vial containing unused EPKINLY.
2.10 Storage and Administration
Storage of EPKINLY Solution in the Syringe
Use EPKINLY solution in the syringe immediately. If not used immediately, store the solution refrigerated at 2°C to 8°C (36°F to 46°F) for up to 24 hours or at room temperature at 20°C to 25°C (68°F to 77°F) for up to 12 hours. The total storage time from the start of dose preparation to administration should not exceed 24 hours. Protect from direct sunlight. Discard unused EPKINLY solution beyond the allowable storage time.
Administration of EPKINLY
To minimize injection pain, allow EPKINLY solution to equilibrate to room temperature for no more than 1 hour before administration. Inject the required volume of EPKINLY into the subcutaneous tissue of the lower part of the abdomen (preferred injection site) or the thigh.
Change of injection site from the left or right side or vice versa is recommended, especially during the weekly administrations (Cycles 1 to 3). Do not inject into tattoos or scars or areas where the skin is red, bruised, tender, hard, or not intact.
3. Dosage Forms and Strengths
EPKINLY is a clear to slightly opalescent, colorless to slightly yellow solution for subcutaneous injection:
- Injection: 4 mg/0.8 mL in a single-dose vial
- Injection: 48 mg/0.8 mL in a single-dose vial
5. Warnings and Precautions
5.1 Cytokine Release Syndrome
EPKINLY can cause CRS, including serious or life-threatening reactions [see Adverse Reactions (6.1)].
Relapsed or Refractory Large B-cell Lymphoma (LBCL)
CRS occurred in 51% of patients with LBCL receiving EPKINLY at the recommended 2-step up dosage schedule in EPCORE NHL, with Grade 1 CRS occurring in 37%, Grade 2 in 17%, and Grade 3 in 2.5% of patients. Recurrent CRS occurred in 16% of patients. Of all the CRS events, most (92%) occurred during Cycle 1. In Cycle 1, 9% of CRS events occurred after the 0.16 mg dose on Cycle 1 Day 1, 16% after the 0.8 mg dose on Cycle 1 Day 8, 61% after the 48 mg dose on Cycle 1 Day 15, and 6% after the 48 mg dose on Cycle 1 Day 22. The median time to onset of CRS from the most recent administered EPKINLY dose across all doses was 24 hours (range: 0 to 10 days). The median time to onset after the first full 48 mg dose was 21 hours (range: 0 to 7 days). CRS resolved in 98% of patients and the median duration of CRS events was 2 days (range: 1 to 27 days). Patients with DLBCL or high-grade B-cell lymphoma should be hospitalized for 24 hours following administration of the first full 48 mg dose [See Dosage and Administration (2.1, 2.2)].
Relapsed or Refractory Follicular Lymphoma (FL)
CRS occurred in 49% (42/86) of patients with FL receiving EPKINLY at the recommended 3-step up dosage schedule in EPCORE NHL-1, with Grade 1 CRS occurring in 45% and Grade 2 in 9% of patients. Recurrent CRS occurred in 23% of patients. Of all the CRS events, most (88%) occurred during Cycle 1. In Cycle 1, 14% of CRS events occurred after the 0.16 mg dose on Cycle 1 Day 1, 7% after the 0.8 mg dose on Cycle 1 Day 8, 17% after the 3 mg dose on Cycle 1 Day 15, and 49% after the 48 mg dose on Cycle 1 Day 22. The median time to onset of CRS from the most recent administered EPKINLY dose across all doses was 59 hours (range: 0.1 to 7 days). The median time to onset after the first full 48 mg dose was 61 hours (range: 0.1 to 7 days). CRS resolved in 100% of patients and the median duration of CRS events was 2 days (range: 1 to 14 days).
In both patients with LBCL and FL who experienced CRS, the signs and symptoms included pyrexia, hypotension, hypoxia, dyspnea, chills, and tachycardia. Concurrent neurological adverse reactions associated with CRS occurred in 2.5% of patients with LBCL and 4.7% of patients with FL. Concurrent neurological adverse reactions observed in patients with LBCL included headache, confusional state, tremors, dizziness, and ataxia. Concurrent neurological adverse reactions observed in patients with FL included headache and dizziness.
Initiate therapy according to EPKINLY step-up dosage schedule. Administer pretreatment medications to reduce the risk of CRS and monitor patients for potential CRS following EPKINLY accordingly [see Dosage and Administration (2.2, 2.3, 2.4)]. At the first signs or symptoms of CRS, immediately evaluate patients for hospitalization, manage per current practice guidelines, and administer supportive care as appropriate. Withhold or discontinue EPKINLY based on the severity of CRS [see Dosage and Administration (2.6)].
Patients who experience CRS (or other adverse reactions that impair consciousness) should be evaluated and advised not to drive and to refrain from operating heavy or potentially dangerous machinery until resolution.
5.2 Immune Effector Cell-Associated Neurotoxicity Syndrome
EPKINLY can cause life-threatening and fatal immune effector cell-associated neurotoxicity syndrome (ICANS) [see Adverse Reactions (6.1)].
Relapsed or Refractory Large B-cell Lymphoma (LBCL)
ICANS occurred in 6% (10/157) of patients with LBCL receiving EPKINLY at the recommended 2-step up dosage schedule in EPCORE NHL-1, with Grade 1 ICANS in 4.5% and Grade 2 ICANS in 1.3% of patients. There was one (0.6%) fatal ICANS occurrence. Of the 10 ICANS events, 9 occurred within Cycle 1 of EPKINLY treatment, with a median time to onset of ICANS of 16.5 days (range: 8 to 141 days) from the start of treatment. Relative to the most recent administration of EPKINLY, the median time to onset of ICANS was 3 days (range: 1 to 13 days). The median duration of ICANS was 4 days (range: 0 to 8 days) with ICANS resolving in 90% of patients with supportive care.
Relapsed or Refractory Follicular Lymphoma (FL)
ICANS occurred in 6% (8/127) of patients with FL receiving EPKINLY following the 2-step up dosage schedule in EPCORE NHL-1, with Grade 1 ICANS in 3.9% and Grade 2 ICANS in 2.4% of patients. The median time to onset of ICANS was 21.5 days (range: 14-66 days) from the start of treatment. Relative to the most recent administration of EPKINLY, the median time to onset of ICANS was 3 days (range: 0.4 to 7 days). The median duration of ICANS was 2 days (range: 1-7 days) with ICANS resolving in 100% of patients.
For patients with LBCL or FL, clinical manifestations of ICANS included, but were not limited to, confusional state, lethargy, tremor, dysgraphia, aphasia, and non-convulsive status epilepticus. The onset of ICANS can be concurrent with CRS, following resolution of CRS, or in the absence of CRS. Monitor patients for potential ICANS following EPKINLY. At the first signs or symptoms of ICANS, immediately evaluate patient and provide supportive therapy based on severity. Withhold or discontinue EPKINLY per recommendations and consider further management per current practice guidelines [see Dosage and Administration (2.6)].
Patients who experience signs or symptoms of ICANS or any other adverse reactions that impair cognition or consciousness should be evaluated, including potential neurology evaluation, and patients at increased risk should be advised not to drive and to refrain from operating heavy or potentially dangerous machinery until resolution.
5.3 Infections
EPKINLY can cause serious and fatal infections [see Adverse Reactions (6.1)].
Serious infections, including opportunistic infections, were reported in 15% of patients with LBCL receiving EPKINLY at the recommended 2-step up dosage schedule in EPCORE NHL-1 and were most commonly due to sepsis (4.5%) and pneumonia (3.2%). Fatal infections occurred in 1.3% of patients and included COVID-19 (1.3%).
Serious infections, including opportunistic infections, were reported in 40% of patients with FL receiving EPKINLY following the 2-step up dosage schedule in EPCORE NHL-1 and were most commonly due to COVID-19 (20%), pneumonia (13%), and urinary tract infections (3%). Fatal infections occurred in 6% of patients and included COVID-19 (5%), pneumonia (0.8%), and sepsis (0.8%).
Monitor patients for signs and symptoms of infection prior to and during treatment with EPKINLY and treat appropriately. Avoid administration of EPKINLY in patients with active infections. Provide PJP prophylaxis prior to initiating treatment with EPKINLY; consider initiating prophylaxis against herpes virus prior to starting EPKINLY [see Dosage and Administration (2.5)].
Withhold or consider permanent discontinuation of EPKINLY based on severity [see Dosage and Administration (2.6)].
5.4 Cytopenias
EPKINLY can cause serious or severe cytopenias, including neutropenia, anemia, and thrombocytopenia [see Adverse Reactions (6.1)].
Among LBCL patients who received EPKINLY at the recommended 2-step up dosage schedule in EPCORE NHL-1, Grade 3 or 4 decreased neutrophils occurred in 32%, decreased hemoglobin in 12%, and decreased platelets in 12% of patients. Febrile neutropenia occurred in 2.5%. In patients with FL who received EPKINLY following the 2-step up dosage schedule in EPCORE NHL-1, Grade 3 or 4 decreased neutrophils occurred in 30%, decreased hemoglobin in 10%, and decreased platelets in 8% of patients. Febrile neutropenia occurred in 3.1%.
Monitor complete blood counts throughout treatment. Based on the severity of cytopenias, temporarily withhold or permanently discontinue EPKINLY [see Dosage and Administration (2.6)]. Consider prophylactic granulocyte colony-stimulating factor administration as applicable.
5.5 Embryo-Fetal Toxicity
Based on its mechanism of action, EPKINLY may cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to the fetus. Advise females of reproductive potential to use effective contraception during treatment with EPKINLY and for 4 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Cytokine Release Syndrome [see Warnings and Precautions (5.1)].
- Immune Effector Cell-Associated Neurotoxicity Syndrome [see Warnings and Precautions (5.2)].
- Infections [see Warnings and Precautions (5.3)].
- Cytopenias [see Warnings and Precautions (5.4)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Relapsed or Refractory Large B-cell Lymphoma (LBCL)
EPCORE NHL-1
The safety of EPKINLY was evaluated in EPCORE NHL-1, a single-arm study of patients with relapsed or refractory LBCL after two or more lines of systemic therapy, including DLBCL not otherwise specified, DLBCL arising from indolent lymphoma, high grade B-cell lymphoma, and other B-cell lymphomas [see Clinical Studies (14.1)]. A total of 157 patients with LBCL received EPKINLY via subcutaneous injection until disease progression or unacceptable toxicities according to the following 28-day cycle schedule:
- Cycle 1: EPKINLY 0.16 mg on Day 1, 0.8 mg on Day 8, 48 mg on Days 15 and 22
- Cycles 2-3: EPKINLY 48 mg on Days 1, 8, 15, and 22
- Cycles 4-9: EPKINLY 48 mg on Days 1 and 15
- Cycles 10 and beyond: EPKINLY 48 mg on Day 1
Of the 157 patients treated, the median age was 64 years (range: 20 to 83), 60% were male, and 97% had an ECOG performance status of 0 or 1. Race was reported in 133 (85%) patients; of these patients, 61% were White, 19% were Asian, and 0.6% were Native Hawaiian or Other Pacific Islander. There were no Black or African American or Hispanic or Latino patients treated in the clinical trial as reported. The median number of prior therapies was 3 (range: 2 to 11). The study excluded patients with CNS involvement of lymphoma, allogeneic HSCT or solid organ transplant, an ongoing active infection, and any patients with known impaired T-cell immunity.
The median duration of exposure for patients receiving EPKINLY was 5 cycles (range: 1 to 20 cycles).
Serious adverse reactions occurred in 54% of patients who received EPKINLY. Serious adverse reactions in ≥ 2% of patients included CRS, infections (including sepsis, COVID-19, pneumonia, and upper respiratory tract infections), pleural effusion, febrile neutropenia, fever, and ICANS. Fatal adverse reactions occurred in 3.8% of patients who received EPKINLY, including COVID-19 (1.3%), hepatotoxicity (0.6%), ICANS (0.6%), myocardial infarction (0.6%), and pulmonary embolism (0.6%).
Permanent discontinuation of EPKINLY due to an adverse reaction occurred in 3.8% of patients. Adverse reactions which resulted in permanent discontinuation of EPKINLY included COVID-19, CRS, ICANS, pleural effusion, and fatigue.
Dosage interruptions of EPKINLY due to an adverse reaction occurred in 34% of patients who received EPKINLY. Adverse reactions which required dosage interruption in ≥ 3% of patients included CRS, neutropenia, sepsis, and thrombocytopenia.
The most common (≥ 20%) adverse reactions were CRS, fatigue, musculoskeletal pain, injection site reactions, pyrexia, abdominal pain, nausea, and diarrhea. The most common Grade 3 to 4 laboratory abnormalities (≥ 10%) were decreased lymphocyte count, decreased neutrophil count, decreased white blood cell count, decreased hemoglobin, and decreased platelets.
Table 9 summarizes the adverse reactions in EPCORE NHL-1.
| EPKINLY (N=157) |
||
|---|---|---|
| Adverse Reaction* | All Grades (%) | Grade 3 or 4 (%) |
|
||
| Immune system disorders | ||
| Cytokine release syndrome† | 51 | 2.5‡ |
| General disorders and administration site conditions | ||
| Fatigue§ | 29 | 2.5‡ |
| Injection site reactions¶ | 27 | 0 |
| Pyrexia | 24 | 0 |
| Edema# | 14 | 1.9‡ |
| Musculoskeletal and connective tissue disorders | ||
| Musculoskeletal painÞ | 28 | 1.3‡ |
| Gastrointestinal disorders | ||
| Abdominal painß | 23 | 1.9‡ |
| Diarrhea | 20 | 0 |
| Nausea | 20 | 1.3‡ |
| Vomiting | 12 | 0.6‡ |
| Skin and subcutaneous disorders | ||
| Rashà | 15 | 0.6‡ |
| Nervous system disorder | ||
| Headache | 13 | 0.6‡ |
| Metabolism and nutrition disorders | ||
| Decreased appetite | 12 | 0.6‡ |
| Cardiac disorders | ||
| Cardiac arrhythmiasè | 10 | 0.6‡ |
Clinically relevant adverse reactions in < 10% of patients who received EPKINLY included ICANS, sepsis, pleural effusion, COVID-19, pneumonia (including pneumonia and COVID-19 pneumonia), tumor flare, febrile neutropenia, upper respiratory tract infections, and tumor lysis syndrome.
Table 10 summarizes laboratory abnormalities in EPCORE NHL-1.
| Laboratory Abnormality* | EPKINLY† | |
|---|---|---|
| All Grades (%) | Grade 3 or 4 (%) | |
|
||
| Hematology | ||
| Lymphocyte count decreased | 87 | 77 |
| Hemoglobin decreased | 62 | 12 |
| White blood cells decreased | 53 | 22 |
| Neutrophils decreased | 50 | 32 |
| Platelets decreased | 48 | 12 |
| Chemistry | ||
| Sodium decreased | 56 | 2.6 |
| Phosphate decreased‡ | 56 | N/A |
| Aspartate aminotransferase increased | 48 | 4.6 |
| Alanine aminotransferase increased | 45 | 5.3 |
| Potassium decreased | 34 | 5.3 |
| Magnesium decreased | 31 | 0 |
| Creatinine increased | 24 | 3.3 |
| Potassium increased | 21 | 1.3 |
Relapsed or Refractory Follicular Lymphoma (FL)
EPCORE NHL-1
The safety of EPKINLY was evaluated in EPCORE NHL-1, a single-arm study of patients with relapsed or refractory FL after two or more lines of systemic therapy who received EPKINLY following a 2-step up dosage schedule (N=127) [see Clinical Studies (14.2)]. A separate dose optimization cohort evaluated the recommended 3-step up dosage schedule for CRS mitigation (N=86), where EPKINLY was administered via subcutaneous injection until disease progression or unacceptable toxicities according to the following 28-day cycle schedule:
- Cycle 1: EPKINLY 0.16 mg on Day 1, 0.8 mg on Day 8, 3 mg on Day 15, and 48 mg on Day 22
- Cycle 2-3: EPKINLY 48 mg on Days 1, 8, 15, and 22
- Cycles 4-9: EPKINLY 48 mg on Days 1 and 15
- Cycles 10 and beyond: EPKINLY 48 mg on Day 1
With the exception of CRS, the safety results presented below and in tables 11 and 12 represent data from patients who received the 2-step up dosage schedule. The data presented for CRS reflects the 86 patients who received the recommended 3-step up dosage schedule. The study excluded patients with CNS involvement of lymphoma, allogeneic HSCT or solid organ transplant, ongoing active infection, any patients with known impaired T-cell immunity, creatinine clearance < 45 ml/min, alanine aminotransferase > 3 times the upper limit of normal, and a cardiac ejection fraction < 45%.
Recommended 3-step up Dosage Schedule
Of the 86 patients with relapsed or refractory FL who received EPKINLY following the recommended 3-step up dosage schedule, the median age was 63.5 years (range: 33-90), 57% were male, and 100% had an ECOG performance status of 0 or 1.
The median duration of exposure was 5 cycles (range: 1 to 12 cycles). CRS occurred in 49% of patients, with Grade 1 CRS occurring in 45% and Grade 2 in 9% of patients. Serious adverse reactions due to CRS occurred in 28% of patients who received EPKINLY. Dose interruptions due to CRS occurred in 19% of patients who received EPKINLY.
2-step up Dosage Schedule
Of the 127 patients with relapsed or refractory FL who received EPKINLY following a 2-step up dosage schedule, the median age was 65 years (range: 39 to 84), 62% were male, and 95% had an ECOG performance status of 0 or 1 [see Clinical Studies (14.2)]. The median duration of exposure for patients receiving EPKINLY was 8 cycles (range: 1 to 33 cycles).
Serious adverse reactions occurred in 66% of patients who received EPKINLY. Serious adverse reactions in ≥ 5% of patients included CRS, COVID-19, pneumonia, and second primary malignancies.
Fatal adverse reactions occurred in 9% of patients who received EPKINLY, including COVID-19 (5%), pneumonitis (1.6%), cardiac failure (0.8%), pneumonia (0.8%), and sepsis (0.8%).
Permanent discontinuation of EPKINLY due to an adverse reaction occurred in 19% of patients who received EPKINLY. Adverse reactions which resulted in permanent discontinuation of EPKINLY in ≥2% of patients included COVID-19, Hepatitis E, pneumonitis, and second primary malignancy.
Dosage interruptions of EPKINLY due to an adverse reaction occurred in 59% of patients who received EPKINLY. Adverse reactions which required dosage interruption in ≥ 5% of patients included COVID-19, CRS, pneumonia, upper respiratory tract infection, and fatigue.
The most common (≥ 20%) adverse reactions were injection site reactions, CRS, COVID-19, fatigue, upper respiratory tract infection, musculoskeletal pain, rash, diarrhea, pyrexia, cough, and headache. The most common Grade 3 to 4 laboratory abnormalities (≥ 10%) were decreased lymphocyte count, decreased neutrophil count, decreased white blood cell count, and decreased hemoglobin.
Table 11 summarizes the adverse reactions in EPCORE NHL-1.
| EPKINLY | ||
|---|---|---|
| Adverse Reaction* | All Grades (%) | Grade 3 or 4 (%) |
|
||
| (N=86)† | ||
| Immune system disorders | ||
| Cytokine release syndromeठ| 49 | 0 |
| (N=127) | ||
| General disorders and administration site conditions | ||
| Injection site reactions¶ | 58 | 0 |
| Fatigue¶ | 37 | 5# |
| Pyrexia¶ | 26 | 2# |
| Edema¶ | 17 | 0 |
| Infections and Infestations | ||
| COVID-19Þ | 40 | 19 |
| Upper respiratory tract infectionß | 29 | 2# |
| Pneumoniaà | 17 | 13# |
| Urinary tract infection¶ | 13 | 5# |
| Herpesvirus infectionè | 12 | 1.6# |
| Musculoskeletal and connective tissue disorders | ||
| Musculoskeletal pain¶ | 28 | 0.8# |
| Arthralgia | 14 | 0.8# |
| Skin and subcutaneous disorders | ||
| Rash¶ | 28 | 0 |
| Gastrointestinal disorders | ||
| Diarrhea | 26 | 1.6# |
| Nausea | 17 | 0 |
| Abdominal pain¶ | 17 | 0.8# |
| Constipation | 16 | 0 |
| Mucositisð | 12 | 0 |
| Respiratory disorders | ||
| Cough¶ | 20 | 0 |
| Dyspnea¶ | 17 | 0 |
| Nervous system disorders | ||
| Headache | 20 | 0 |
| Neurological changesø | 13 | 0 |
| Peripheral neuropathy and paresthesiaý | 13 | 1.6# |
| Dizziness | 11 | 0 |
| Psychiatric disorders | ||
| Insomnia | 13 | 0 |
| Renal and urinary disorders | ||
| Renal insufficiency£ | 10 | 1.6# |
Clinically relevant adverse reactions in < 10% of patients (N=127) who received EPKINLY included vomiting, pruritis, hepatotoxicity, ICANS, lower respiratory tract infections, cardiac arrhythmias, respiratory tract infections, pneumonitis, second primary malignancy, vision changes, cellulitis, febrile neutropenia, cardiac failure, cytomegalovirus infection and sepsis.
Table 12 summarizes laboratory abnormalities in EPCORE NHL-1.
| Laboratory Abnormality* | EPKINLY†
(N=127) |
|
|---|---|---|
| All Grades | Grade 3 or 4 (%) | |
| Hematology | ||
| Lymphocytes decreased | 94 | 82 |
| Hemoglobin decreased | 59 | 10 |
| White blood cells decreased | 58 | 19 |
| Neutrophils decreased | 55 | 30 |
| Platelets decreased | 49 | 8 |
| Chemistry | ||
| Sodium decreased | 51 | 1.6 |
| ALT increased | 47 | 8 |
| AST increased | 44 | 6 |
| Creatinine increased | 36 | 0.8 |
| Alkaline phosphatase increased | 29 | 0 |
| Bilirubin increased | 28 | 1.6 |
| Potassium decreased | 20 | 3.1 |
| Magnesium decreased | 20 | 0.8 |
7. Drug Interactions
For certain CYP substrates, minimal changes in the concentration may lead to serious adverse reactions. Monitor for toxicity or drug concentrations of such CYP substrates when co-administered with EPKINLY.
Epcoritamab-bysp causes release of cytokines [see Clinical Pharmacology (12.2)] that may suppress activity of CYP enzymes, resulting in increased exposure of CYP substrates. Increased exposure of CYP substrates is more likely to occur after the first dose of EPKINLY and up to 14 days after the first 48 mg dose, and during and after CRS [see Warnings and Precautions (5.1)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Based on the mechanism of action, EPKINLY may cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data on the use of EPKINLY in pregnant women to evaluate for a drug-associated risk. No animal reproductive or developmental toxicity studies have been conducted with epcoritamab-bysp.
Epcoritamab-bysp causes T-cell activation and cytokine release; immune activation may compromise pregnancy maintenance. In addition, based on expression of CD20 on B-cells and the finding of B-cell depletion in non-pregnant animals, epcoritamab-bysp can cause B-cell lymphocytopenia in infants exposed to epcoritamab-bysp in-utero. Human immunoglobulin G (IgG) is known to cross the placenta; therefore, EPKINLY has the potential to be transmitted from the mother to the developing fetus. Advise women of the potential risk to the fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of epcoritamab-bysp in human milk, the effect on the breastfed child, or milk production. Because maternal IgG is present in human milk, and there is potential for epcoritamab-bysp absorption leading to serious adverse reactions in a breastfed child, advise women not to breastfeed during treatment with EPKINLY and for 4 months after the last dose.
8.3 Females and Males of Reproductive Potential
EPKINLY may cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
8.4 Pediatric Use
The safety and efficacy of EPKINLY in pediatric patients have not been established.
8.5 Geriatric Use
LBCL
In patients with relapsed or refractory LBCL who received EPKINLY in EPCORE NHL-1, 77 (49%) were 65 years of age and older, and 29 (19%) were 75 years of age or older. No clinically meaningful differences in safety or efficacy were observed between patients with relapsed or refractory LBCL who were 65 years of age and older compared with younger adult patients
FL
In patients with relapsed or refractory FL who received EPKINLY in EPCORE NHL-1, 66 (52%) were 65 years of age or older, and 16 (13%) were 75 years of age and older.
In patients with relapsed or refractory FL, there was a higher rate of fatal adverse reactions, primarily infections, including COVID-19, in patients older than 65 years of age compared to younger adult patients. No overall difference in efficacy was observed in patients with relapsed or refractory FL who were 65 years of age and older compared with younger adult patients.
11. Epkinly Description
Epcoritamab-bysp is a bispecific CD20-directed CD3 T-cell engager; it is a humanized bispecific IgG1 antibody. Epcoritamab-bysp is manufactured in Chinese hamster ovary (CHO) cells using recombinant DNA technology and has an approximate molecular weight of 149 kDa.
EPKINLY (epcoritamab-bysp) injection for subcutaneous use is a sterile, preservative-free, clear to slightly opalescent, colorless to slightly yellow solution, free of visible particles.
Each single-dose 4 mg/0.8 mL vial contains epcoritamab-bysp (4 mg), acetic acid (0.19 mg), polysorbate 80 (0.32 mg), sodium acetate (1.7 mg), sorbitol (21.9 mg) and Water for Injection, USP. The pH is 5.5.
Each single-dose 48 mg/0.8 mL vial contains epcoritamab-bysp (48 mg), acetic acid (0.19 mg), polysorbate 80 (0.32 mg), sodium acetate (1.7 mg), sorbitol (21.9 mg) and Water for Injection, USP. The pH is 5.5.
12. Epkinly - Clinical Pharmacology
12.1 Mechanism of Action
Epcoritamab-bysp is a T-cell engaging bispecific antibody that binds to the CD3 receptor expressed on the surface of T-cells and CD20 expressed on the surface of lymphoma cells and healthy B-lineage cells.
In vitro, epcoritamab-bysp activated T-cells, caused the release of proinflammatory cytokines, and induced lysis of B-cells.
12.2 Pharmacodynamics
Circulating B-Cell Count
Circulating B-cells decreased to undetectable levels (< 10 cells/microliter) after administration of the approved recommended dosage of EPKINLY in patients who had detectable B-cells at treatment initiation by Cycle 1 Day 15 and the depletion was sustained while patients remained on treatment.
Cytokine Concentrations
Plasma concentrations of cytokines (IL-2, IL-6, IL-10, TNF-α, and IFN-γ) were measured. Transient elevation of circulating cytokines was observed at dose levels of 0.04 mg and above. After administration of the approved recommended dosages of EPKINLY, cytokine levels increased within 24 hours after the first dose on Cycle 1 Day 1, generally reached maximum levels after the first 48 mg dose, and returned to baseline prior to the second 48 mg full dose.
12.3 Pharmacokinetics
Pharmacokinetic (PK) parameters were evaluated at the approved recommended dosage (48 mg) and are presented as geometric mean (CV%) unless otherwise specified.
Epcoritamab-bysp area under the concentration-time curve (AUC) increased more than proportionally over a full dosage range from 1.5 to 60 mg (0.03125 to 1.25 times the approved recommended dosage).
Epcoritamab-bysp maximum concentration (10.2 mcg/mL [43.2%]) is achieved after the first dose of the Q2W regimen (i.e., the first dose of Cycle 4). No clinically significant differences in pharmacokinetic parameters were observed between patients with relapsed or refractory LBCL and patients with relapsed or refractory FL. PK exposures are summarized for the recommended dosage of EPKINLY in Table 13.
| Cavg
(mcg/mL)* | Cmax
(mcg/mL)* | Ctrough
(mcg/mL)* |
|
|---|---|---|---|
| First full 48 mg dose† | 1.3 (113.3%) | 1.7 (106.7%) | 1.4 (100.9%) |
| End of weekly dosing (end of Cycle 3) | 9.1 (45.9%) | 9.9 (43.4%) | 7.8 (52.4%) |
| End of every 2-week dosing (end of Cycle 9) | 5.3 (57%) | 6.7 (49.4%) | 3.6 (81.5%) |
| Steady state‡ with every 4-week dosing | 2.4 (73.3%) | 4.2 (59.8%) | 1.1 (134.1%) |
Absorption
The median (range) Tmax of epcoritamab-bysp after the first full dose and end of the weekly dosing regimen (end of Cycle 3) treatment doses were 4 (0.3 to 7) days and 2.3 (0.3 to 3.2) days, respectively.
Elimination
The half-life of full dose epcoritamab-bysp (48 mg) was approximately 22 days (58%) at the end of Cycle 3, with apparent total clearance of approximately 0.53 L/day (40%) after the end of Cycle 3.
Specific Populations
No clinically significant differences in the PK of epcoritamab-bysp were observed based on age (20 to 89 years), sex, race (White or Asian), mild to moderate renal impairment (creatinine clearance [CLcr] 30 to < 90 mL/min as estimated by Cockcroft-Gault formula), and mild hepatic impairment (total bilirubin ≤ ULN and AST > ULN, or total bilirubin 1 to 1.5 times ULN and any AST) after accounting for differences in bodyweight.
The effects of severe renal impairment (CLcr 15 to < 30 mL/min), end-stage renal disease (CLcr < 15 mL/min), or moderate to severe hepatic impairment (total bilirubin > 1.5 times ULN and any AST) on the PK of epcoritamab-bysp are unknown.
Body Weight
In patients who received the recommended dosage of EPKINLY, geometric mean average concentration following the first full 48 mg dose was 31% lower in the higher body weight (BW) group (85 to 172 kg) and 13% higher in the lower BW group (39 to 65 kg) compared to patients with BW of 65 to less than 85 kg.
12.6 Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies (ADA) in the study described below with the incidence of ADA in other studies, including those of epcoritamab-bysp.
Anti-epcoritamab-bysp antibodies developed in 2.6% of patients (4 of 156) with LBCL and 4.2% of patients (8 of 190) with FL treated with EPKINLY in Study EPCORE NHL-1 (up to 10 cycles) [see Clinical Studies (14.1, 14.2)] using an electrochemiluminescence immunoassay (ECLIA). Because of the low occurrence of anti-drug antibodies, the effect of these antibodies on the PK, pharmacodynamics, safety, and effectiveness of epcoritamab-bysp is unknown.
14. Clinical Studies
14.1 DLBCL and High-grade B-cell Lymphoma
The efficacy of EPKINLY was evaluated in EPCORE NHL-1 (Study GCT3013-01; NCT03625037), an open-label, multi-cohort, multicenter, single-arm trial in 157 patients with relapsed or refractory large B-cell lymphoma (LBCL) after two or more lines of systemic therapy. The study excluded patients with CNS involvement of lymphoma, allogeneic HSCT or solid organ transplant, ongoing active infection, and any patients with known impaired T-cell immunity. Patients received EPKINLY monotherapy at the recommended 2-step up dosage schedule:
- Cycle 1: EPKINLY 0.16 mg on Day 1, 0.8 mg on Day 8, 48 mg on Days 15 and 22
- Cycles 2-3: EPKINLY 48 mg on Days 1, 8, 15, and 22
- Cycles 4-9: EPKINLY 48 mg on Days 1 and 15
- Cycles 10 and beyond: EPKINLY 48 mg on Day 1
Patients continued to receive EPKINLY until disease progression or unacceptable toxicity. In the setting of a suspected tumor flare reaction, continued treatment was permitted.
The efficacy population includes 148 patients with DLBCL, not otherwise specified (NOS), including DLBCL arising from indolent lymphoma, and high-grade B-cell lymphoma. Of the 148 patients, the median age was 65 years (range: 22 to 83), 62% were male, 97% had an ECOG performance status of 0 or 1, and 3% had an ECOG performance status of 2. Race was reported in 125 (84%) patients; of these patients, 61% were White, 20% were Asian, and 0.7% were Native Hawaiian or Other Pacific Islander. There were no Black or African American or Hispanic or Latino patients treated in the clinical trial as reported. The diagnosis was DLBCL NOS in 86%, including 27% with DLBCL transformed from indolent lymphoma, and high-grade B-cell lymphoma in 14%. The median number of prior therapies was 3 (range: 2 to 11), with 30% receiving 2 prior therapies, 30% receiving 3 prior therapies, and 40% receiving 4 or more prior therapies. Eighteen percent had prior autologous HSCT, and 39% had prior chimeric antigen receptor (CAR) T-cell therapy. Eighty-two percent of patients had disease refractory to last therapy and 29% of patients were refractory to CAR T-cell therapy.
Efficacy was established based on overall response rate (ORR) determined by Lugano 2014 criteria as assessed by Independent Review Committee (IRC) and duration of response. The efficacy results are summarized in Table 14.
| Endpoint* | EPKINLY (N=148) |
|---|---|
| ORR = overall response rate; CI = confidence interval; CR = complete response; PR = partial response; DOR = duration of response; NR = not reached. | |
|
|
| ORR†, n (%) | 90 (61) |
| (95% CI) | (52.5, 68.7) |
| CR, n (%) | 56 (38) |
| (95% CI) | (30.0, 46.2) |
| PR, n (%) | 34 (23) |
| (95% CI) | (16.5, 30.6) |
| DOR | |
| Median (95% CI), months | 15.6 (9.7, NR) |
| 9-month estimate‡ % (95% CI) | 63 (51.5, 72.4) |
The median time to response was 1.4 months (range: 1 to 8.4 months). Among responders, the median follow-up for DOR was 9.8 months (range: 0.0 to 17.3 months).
14.2 Follicular Lymphoma
The efficacy of EPKINLY was evaluated in EPCORE NHL-1 (Study GCT3013-01; NCT03625037), an open-label, multi-cohort, multicenter, single-arm trial that included patients with relapsed or refractory follicular lymphoma (FL) after at least 2 lines of systemic therapy. The study excluded patients with CNS involvement of lymphoma, allogeneic HSCT or solid organ transplant, ongoing active infection, any patients with known impaired T-cell immunity, creatinine clearance < 45 mL/min, alanine aminotransferase > 3 times the upper limit of normal, and a cardiac ejection fraction < 45%. Patients received EPKINLY monotherapy following a 2-step up dosage schedule:
- Cycle 1: EPKINLY 0.16 mg on Day 1, 0.8 mg on Day 8, 48 mg on Days 15 and 22
- Cycles 2-3: EPKINLY 48 mg on Days 1, 8, 15, and 22
- Cycles 4-9: EPKINLY 48 mg on Days 1 and 15
- Cycles 10 and beyond: EPKINLY 48 mg on Day 1
Patients continued to receive EPKINLY until disease progression or unacceptable toxicity.
Among the 127 patients with FL, the median age was 65 years (range: 39 to 84), 52% were 65 years of age or older, and 62% were male. Race was reported in 85 (67%) patients; of these patients, 89% were White, and 8% were Asian. A total of 85% had stage III-IV disease, 25% had bulky disease, 95% had an ECOG performance status of 0 or 1, and 6% had an ECOG performance status of 2. The median number of prior therapies was 3 (range: 2 to 9), with 36% receiving 2 prior lines of systemic therapy, 32% receiving 3 prior therapies, and 32% receiving 4 or more prior therapies.
Seventy-nine percent of patients were refractory to prior anti-CD20 monoclonal antibody therapy, 70% were refractory to both anti-CD20 monoclonal antibody and alkylator therapy, 21% had prior rituximab plus lenalidomide therapy, 19% received prior autologous HSCT, and 5% received prior chimeric antigen receptor (CAR) T-cell therapy. Fifty-two percent of patients had progression of disease within 24 months of first systemic therapy.
Efficacy was established based on overall response rate (ORR) determined by Lugano 2014 criteria as assessed by Independent Review Committee (IRC) and duration of response. The median follow-up for DOR was 14.8 months. The efficacy results are summarized in Table 15.
| Endpoint* | EPKINLY (N=127) |
|---|---|
| ORR = overall response rate; CI = confidence interval; CR = complete response; PR = partial response; DOR = duration of response; NR = not reached. | |
| ORR, n (%) | 104 (82) |
| (95% CI) | (74.1, 88.2) |
| CR, n (%) | 76 (60) |
| (95% CI) | (50.8, 68.4) |
| PR, n (%) | 28 (22) |
| (95% CI) | (15.2, 30.3) |
| DOR | |
| Median (95% CI), months | NR (13.7, NR) |
| 12-month estimate† % (95% CI) | 68.4 (57.6, 77.0) |
The median time to first response was 1.4 months (range: 1 to 3 months).
In a separate dose optimization cohort in EPCORE NHL-1, 86 patients received the recommended 3-step up dosage schedule in Cycle 1 [see Adverse Reactions (6.1)]. The efficacy results in this cohort were comparable to the primary efficacy population.
16. How is Epkinly supplied
How Supplied
EPKINLY (epcoritamab-bysp) injection is a sterile, preservative-free, clear to slightly opalescent, colorless to slightly yellow solution, free of visible particles, supplied in glass vials as follows:
| Carton contents | NDC number |
|---|---|
| One 4 mg/0.8 mL single-dose vial | NDC 82705-002-01 |
| One 48 mg/0.8 mL single-dose vial | NDC 82705-010-01 |
The vial stopper is not made with natural rubber latex.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Cytokine Release Syndrome (CRS)
Inform patients of the risk of CRS, and to immediately contact their healthcare provider should signs and symptoms associated with CRS (e.g., pyrexia, hypotension, hypoxia, chills, tachycardia, headache, and dyspnea) occur at any time. Advise patients with DLBCL or high-grade B-cell lymphoma that they should be hospitalized for 24 hours after administration of the Cycle 1 Day 15 dosage of 48 mg. Advise all patients who experience symptoms that impair consciousness not to drive and refrain from operating heavy or potentially dangerous machinery until events resolve [see Warnings and Precautions (5.1)].
Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS)
Advise patients of the risk of ICANS, to immediately contact their healthcare provider for signs and symptoms associated with ICANS, which may manifest, for example, as confusional state, lethargy, tremor, dysgraphia, aphasia, and non-convulsive status epilepticus, and that the onset of events may be delayed. Advise patients who experience symptoms of ICANS that impair consciousness to refrain from driving or operating heavy or potentially dangerous machinery until symptoms of ICANS resolve [see Warnings and Precautions (5.2)].
Infections
Advise patients of the risk of serious infections, and to contact their healthcare professional for signs or symptoms of serious infection [see Warnings and Precautions (5.3)].
Cytopenias
Discuss the signs and symptoms associated with cytopenias, including neutropenia and febrile neutropenia, anemia, and thrombocytopenia [see Warnings and Precautions (5.4)].
Embryo-Fetal Toxicity
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to inform their healthcare provider if they are pregnant or become pregnant [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with EPKINLY and for 4 months after the last dose [see Use in Specific Populations (8.3)].
Lactation
Advise women not to breastfeed during treatment with EPKINLY and for 4 months after the last dose [see Use in Specific Populations (8.2)].
Manufactured by:
Genmab US, Inc.
Plainsboro, NJ 08536, USA
1-855-4GENMAB (1-855-443-6622)
U.S. License Number: 2293
Marketed by:
Genmab US, Inc.
Plainsboro, NJ 08536
and
AbbVie Inc.
North Chicago, IL 60064
EPKINLY is a trademark owned by Genmab A/S
©2024 Genmab A/S
| MEDICATION GUIDE EPKINLY™ (ep-KIN-lee) (epcoritamab-bysp) injection, for subcutaneous use |
||||
|---|---|---|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: June 2024 | |||
| What is the most important information I should know about EPKINLY? EPKINLY can cause serious side effects, including:
|
||||
|
|
|||
Due to the risk of CRS, you will receive EPKINLY on a "step-up dosing schedule".
|
||||
|
||||
|
|
|||
| Your healthcare provider will monitor you for signs and symptoms of CRS and neurologic problems during treatment with EPKINLY, as well as other side effects and treat you if needed. Your healthcare provider may temporarily stop or completely stop your treatment with EPKINLY if you develop CRS, neurologic problems, or any other side effects that are severe. | ||||
| People with diffuse large B-cell lymphoma (DLBCL) or high-grade B-cell lymphoma should be hospitalized for 24 hours after receiving their first full dose of EPKINLY on Day 15 of Cycle 1 due to the risk of CRS and neurologic problems. See "What are the possible side effects of EPKINLY?" for more information about side effects. |
||||
| What is EPKINLY?
EPKINLY is a prescription medicine used to treat adults with certain types of DLBCL, high-grade B-cell lymphoma, or follicular lymphoma:
|
||||
| It is not known if EPKINLY is safe and effective in children. | ||||
Before receiving EPKINLY, tell your healthcare provider about all of your medical conditions, including if you:
|
||||
How will I receive EPKINLY?
|
||||
| What should I avoid while receiving EPKINLY?
Do not drive, operate heavy machinery, or do other dangerous activities if you develop dizziness, confusion, tremors, sleepiness, or any other symptoms that impair consciousness until your signs and symptoms go away. These may be signs and symptoms of CRS or neurologic problems. See "What is the most important information I should know about EPKINLY?" for more information about signs and symptoms of CRS and neurologic problems. |
||||
| What are the possible side effects of EPKINLY?
EPKINLY can cause serious side effects, including:
|
||||
|
|
|||
The most common side effects of EPKINLY in DLBCL or high-grade B-cell lymphoma include: |
||||
|
|
|
||
| The most common severe abnormal laboratory test results with EPKINLY in DLBCL or high-grade B-cell lymphoma include: decreased white blood cells, decreased red blood cells, and decreased platelets. The most common side effects of EPKINLY in follicular lymphoma include: |
||||
|
|
|
||
| The most common severe abnormal laboratory test results with EPKINLY in follicular lymphoma include: decreased white blood cells and decreased red blood cells. These are not all of the possible side effects of EPKINLY. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
| General information about safe and effective use of EPKINLY.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or healthcare provider for information about EPKINLY that is written for health professionals. |
||||
| What are the ingredients in EPKINLY?
Active ingredient: epcoritamab-bysp Inactive ingredients: acetic acid, polysorbate 80, sodium acetate, sorbitol and Water for Injection. Manufactured by: Genmab US, Inc., Plainsboro, NJ 08536 U.S. License Number: 2293 Marketed by: Genmab US, Inc., Plainsboro, NJ 08536 and AbbVie Inc., North Chicago, IL 60064 EPKINLY is a trademark owned by Genmab A/S ©2024 Genmab A/S For more information, go to www.EPKINLY.com or call 1-855-4GENMAB (1-855-443-6622) |
||||
| EPKINLY
epcoritamab-bysp injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| EPKINLY
epcoritamab-bysp injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Genmab US, Inc. (014190016) |
Frequently asked questions
More about Epkinly (epcoritamab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: bispecific T-cell engagers (BiTE)
- En español