Brexucabtagene Autoleucel
Medically reviewed by Drugs.com. Last updated on Nov 14, 2024.
Index Terms
- Anti-CD19/CD28/CD3zeta CAR Gammaretroviral Vector-transduced Autologous T Lymphocytes KTE-X19
- Autologous Anti-CD19 CAR-positive T lymphocytes KTE-X19
- KTE-X19
- KTE-X19 CAR
- KTEX19
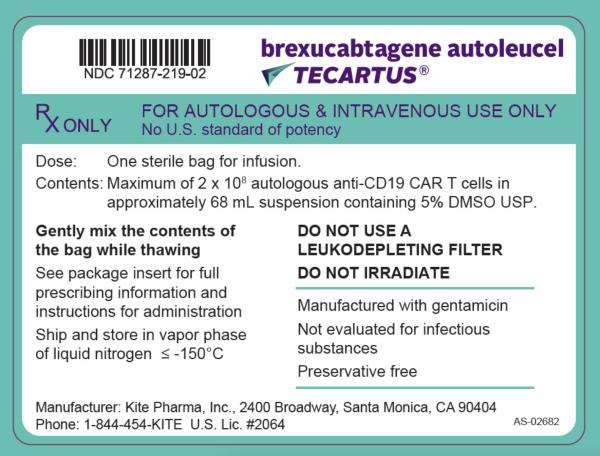
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Intravenous:
Tecartus: (1 ea) [contains albumin human]
Brand Names: U.S.
- Tecartus
Pharmacologic Category
- Antineoplastic Agent, Anti-CD19
- Antineoplastic Agent, CAR-T Immunotherapy
- CAR-T Cell Immunotherapy
- Cellular Immunotherapy, Autologous
- Chimeric Antigen Receptor T-Cell Immunotherapy
Pharmacology
Brexucabtagene autoleucel is a CD19-directed genetically modified autologous T-cell immunotherapy in which a patient's T cells are reprogrammed with a transgene encoding a chimeric antigen receptor (CAR) to identify and eliminate CD19-expressing malignant and normal cells. The CAR is comprised of a murine single-chain antibody fragment which recognizes CD19 and is fused to CD28 and CD3 zeta. CD3 zeta is a critical component for initiating T-cell activation and antitumor activity. After binding to CD19-expressing cells, the CD28 and CD3-zeta costimulatory domains activate downstream signaling cascades, which results in T-cell activation, proliferation, acquisition of effector functions, and secretion of inflammatory cytokines and chemokines, leading to destruction of CD19-expressing cells. Brexucabtagene autoleucel is prepared from the patient's peripheral blood cells obtained via leukapheresis.
Onset of Action
Median time to initial response: 1 month (range: 0.8 to 3.1 months); median time to complete response: 3 months (range: 0.9 to 9.3 months) (Wang 2020).
Time to Peak
Peak levels of anti-CD19 chimeric antigen receptor T cells occurred within the first 7 to 14 days after infusion.
Duration of Action
Anti-CD19 chimeric antigen receptor T cells displayed an initial rapid expansion followed by a decline to near baseline levels by 3 months post-brexucabtagene autoleucel infusion.
Use: Labeled Indications
Mantle cell lymphoma, relapsed or refractory: Treatment of relapsed or refractory mantle cell lymphoma (MCL) in adults.
Contraindications
There are no contraindications listed in the manufacturer's labeling.
Dosing: Adult
For autologous use only; confirm patient identity matches cassette and infusion bag prior to infusion.
Mantle cell lymphoma, relapsed or refractory: Note: A treatment course consists of lymphodepleting chemotherapy (with fludarabine and cyclophosphamide) on the fifth, fourth, and third day prior to brexucabtagene autoleucel infusion (confirm availability of autologous brexucabtagene autoleucel prior to initiating lymphodepleting chemotherapy). Ensure tocilizumab and emergency equipment are available prior to brexucabtagene autoleucel infusion and during recovery period.
Premedicate with acetaminophen and diphenhydramine (or another H1-antagonist) ~30 to 60 minutes prior to brexucabtagene autoleucel infusion. Avoid prophylactic systemic corticosteroids because they may interfere with the brexucabtagene autoleucel activity.
IV: Target dose: 2 × 106 chimeric antigen receptor (CAR)-positive viable T cells per kg body weight (Wang 2020); maximum dose: 2 × 108 CAR-positive viable T cells.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Cytokine release syndrome: Note: Monitor patients with ≥ grade 2 cytokine release syndrome (CRS) with continuous cardiac telemetry and pulse oximetry. Consider obtaining an echocardiogram in patients with severe CRS; severe or life-threatening CRS may require intensive care supportive therapy.
CRS Grade | Tocilizumab | Corticosteroids |
|---|---|---|
Grade 1: Symptoms require symptomatic treatment only (eg, fever, nausea, fatigue, headache, myalgia, malaise). | If not improving after 24 hours, administer tocilizumab 8 mg/kg IV over 1 hour (maximum 800 mg/dose). | Not indicated. |
Grade 2: Symptoms require and respond to moderate intervention. Oxygen requirement <40% FiO2 or hypotension responsive to fluids or low-dose of one vasopressor or grade 2 organ toxicity. | Administer tocilizumab 8 mg/kg IV over 1 hour (maximum 800 mg/dose); may repeat every 8 hours as needed if not responsive to IV fluids or requiring increased supplemental oxygen. Maximum tocilizumab: 3 doses in 24 hours, maximum total of 4 doses if no clinical improvement in CRS signs/symptoms. If improving, discontinue tocilizumab. | If no improvement within 24 hours after initiating tocilizumab, manage as grade 3. If improving, taper corticosteroids. |
Grade 3: Symptoms require and respond to aggressive intervention. Oxygen requirement ≥40% FiO2 or hypotension requiring high-dose or multiple vasopressors or grade 3 organ toxicity or grade 4 transaminitis. | Administer tocilizumab as per grade 2. If improving, discontinue tocilizumab. | Administer methylprednisolone 1 mg/kg IV twice daily or equivalent dexamethasone (eg, 10 mg IV every 6 hours) until grade 1, then taper corticosteroids. If improving, manage as grade 2. If not improving, manage as grade 4. |
Grade 4: Life-threatening symptoms. Requirements for ventilator support, CVVHD or grade 4 organ toxicity (excluding transaminitis). | Administer tocilizumab as per grade 2. If improving, discontinue tocilizumab. | Administer methylprednisolone 1 g IV daily for 3 days; if improving, taper corticosteroids, and manage as grade 3. If not improving, consider alternate immunosuppressants. |
Neurologic toxicity: Note: Monitor patients with ≥ grade 2 neurologic toxicity with continuous cardiac telemetry and pulse oximetry. Severe or life-threatening neurologic toxicity may require intensive care supportive therapy. Consider nonsedating antiseizure medication (eg, levetiracetam) for seizure prophylaxis for any ≥ grade 2 neurologic toxicity.
Neurologic Event | Concurrent CRS | No Concurrent CRS |
|---|---|---|
aADLs = activities of daily living. | ||
Grade 1: Somnolence – mild drowsiness or sleepiness. Confusion – mild disorientation. Encephalopathy – mild limiting of ADLsa. Dysphasia – not impairing ability to communicate. | Administer tocilizumab per previous (CRS) table for management of grade 1 CRS. | Supportive care. |
Grade 2: Somnolence – moderate limiting of instrumental ADLs. Confusion – moderate disorientation. Encephalopathy – limiting instrumental ADLs. Dysphasia – moderate, impairing ability to communicate spontaneously. Seizure(s). | Administer tocilizumab per previous (CRS) table for management of grade 2 CRS. If not improving within 24 hours of initiating tocilizumab, administer dexamethasone 10 mg IV every 6 hours until ≤ grade 1, then taper corticosteroids. If improving, discontinue tocilizumab. If still not improving, manage as grade 3. | Administer dexamethasone 10 mg IV every 6 hours until ≤ grade 1. If improving, taper corticosteroids. |
Consider nonsedating antiseizure medication (eg, levetiracetam) for seizure prophylaxis. | ||
Grade 3: Somnolence – obtundation or stupor. Confusion – severe disorientation. Encephalopathy – limiting self-care ADLs. Dysphasia – severe receptive or expressive characteristics, impairing ability to read, write, or communicate intelligibly. | Administer tocilizumab per previous (CRS) table for management of grade 2 CRS. In addition, administer dexamethasone 10 mg IV every 6 hours (administer the first dose with the first dose of tocilizumab); continue until ≤ grade 1, then taper corticosteroids. If improving, discontinue tocilizumab and manage as grade 2. If still not improving, manage as grade 4. | Administer dexamethasone 10 mg IV every 6 hours; continue until ≤ grade 1, then taper corticosteroids. If not improving, manage as grade 4. |
Consider nonsedating antiseizure medication (eg, levetiracetam) for seizure prophylaxis. | ||
Grade 4: Life-threatening consequences. Urgent intervention indicated. Requirement for mechanical ventilation. Consider cerebral edema. | Administer tocilizumab per previous (CRS) table for management of grade 2 CRS. Administer methylprednisolone 1 g IV daily for 3 days (administer the first dose with the first dose of tocilizumab). If improving, then manage as grade 3. If not improving, consider alternate immunosuppressants. | Administer methylprednisolone 1 g IV daily for 3 days. If improving, then manage as grade 3. If not improving, consider alternate immunosuppressants. |
Consider nonsedating antiseizure medication (eg, levetiracetam) for seizure prophylaxis. | ||
Reconstitution
Do not remove the infusion bag from the cassette if the information on the cassette label does not match the intended patient. Inspect patient-specific infusion bag for breaches in container integrity (such as breaks or cracks) prior to thawing (if bag is compromised, contact manufacturer). Place infusion bag inside a second sterile bag. Thaw at ~37°C (~98.6°F) using a water bath or dry thaw method until there is no visible ice in the infusion bag. Gently mix contents of the thawed infusion bag to disperse cellular material clumps; inspect for visible cell clumps; if visible cell clumps remain, gently mix the contents of the bag (small clumps of cellular material should disperse with gentle manual mixing). Do not wash, spin down, and/or re-suspend brexucabtagene autoleucel in new media prior to infusion. Brexucabtagene autoleucel contains human blood cells that are genetically modified with replication incompetent retroviral vector. Follow universal precautions and local biosafety guidelines for handling and disposal.
Administration
IV: For IV use only. Administer in a health care facility. For autologous use only. Coordinate the timing of administration with thawing (may be stored for up to 3 hours at room temperature after thawing); infusion start time may need to be adjusted based on thawing.
Prime the tubing with NS prior to infusion. Infuse entire contents of bag within 30 minutes either by gravity or a peristaltic pump (infusion bag volume is ~68 mL). A central line is preferred for infusion. Gently agitate the bag during infusion to prevent cell clumping. After completion of the infusion, rinse the tubing with NS at the same infusion rate to ensure complete cell product delivery. Do not use a leukodepleting filter.
Prior to administration: Ensure tocilizumab and emergency equipment are available prior to infusion and during recovery period. Premedicate with acetaminophen and diphenhydramine (or another H1-antagonist) ~30 to 60 minutes prior to brexucabtagene autoleucel infusion. Avoid prophylactic systemic corticosteroids because they may interfere with the brexucabtagene autoleucel activity. Confirm patient identity and match to patient identifiers on the infusion cassette and bag. Inspect the contents of the thawed infusion bag for visible cell clumps; if visible cell clumps remain, gently mix the contents of the bag (small clumps of cellular material should disperse with gentle manual mixing). Do not infuse if clumps are not dispersed, if the infusion bag is damaged or leaking, or if it otherwise appears to be compromised. Apply universal precautions for product handling. Monitor patient daily at the healthcare facility for at least 7 days after cell infusion; patient should remain within proximity of the facility for at least 4 weeks after infusion.
Storage
Store frozen suspension in the vapor phase of liquid nitrogen (-150°C or less [-238°F or less]). After thawing, may be stored for up to 3 hours at room temperature of 20°C to 25°C (68°F to 77°F).
Drug Interactions
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Management: Consider avoiding Echinacea in patients receiving therapeutic immunosuppressants. If coadministered, monitor for reduced efficacy of the immunosuppressant during concomitant use. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Inebilizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Management: Avoid use of immunosuppressants (including systemic corticosteroids) prior to initiation of nivolumab. Use of immunosuppressants after administration of nivolumab (eg, for immune-related toxicity) is unlikely to affect nivolumab efficacy. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Ozanimod: Immunosuppressants may enhance the immunosuppressive effect of Ozanimod. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Management: Consider avoiding concomitant use of roflumilast and immunosuppressants as recommended by the Canadian product monograph. Inhaled or short-term corticosteroids are unlikely to be problematic. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Talimogene Laherparepvec: Immunosuppressants may enhance the adverse/toxic effect of Talimogene Laherparepvec. Specifically, the risk for disseminated herpetic infection may be increased. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Management: Concomitant use of upadacitinib with potent immunosuppressants is not recommended. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated less than 2 weeks before starting or during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Brexucabtagene Autoleucel may enhance the adverse/toxic effect of Vaccines (Live). Brexucabtagene Autoleucel may diminish the therapeutic effect of Vaccines (Live). Avoid combination
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
>10%:
Cardiovascular: Edema (35%), hypertension (18%), hypotension (57%), tachycardia (45%), thrombosis (17%)
Dermatologic: Skin rash (9% to 22%)
Endocrine & metabolic: Hypocalcemia (grade 3/4: 21%), hyponatremia (grade 3/4: 16%), hypophosphatemia (grade 3/4: 30%), increased uric acid (grade 3/4: 17%)
Gastrointestinal: Abdominal pain (17%), constipation (29%), decreased appetite (26%), diarrhea (28%), nausea (35%), vomiting (13%)
Genitourinary: Decreased urine output (11%)
Hematologic & oncologic: Anemia (grade 3/4: 55%), hypogammaglobulinemia (16%; grade ≥3: 1%), leukopenia (grade 3/4: 95%), lymphocytopenia (grade 3/4: 86%), neutropenia (grade 3/4: 95%), thrombocytopenia (grade 3/4: 63%)
Hepatic: Increased serum alanine aminotransferase (grade 3/4: 15%), increased serum aspartate aminotransferase (grade 3/4: 15%)
Hypersensitivity: Cytokine release syndrome (91%)
Infection: Bacterial infection (13%), infection (43% to 56%; including severe infection), viral infection (18%)
Nervous system: Anxiety (16%), aphasia (20% to 23%), chills (41%), delirium (16% to 18%), dizziness (18%), encephalopathy (51%), fatigue (48%), headache (35%), insomnia (21%), motor dysfunction (17%), mouth pain (16%), neuropathy (13%), neurotoxicity (81%), pain (17%)
Neuromuscular & skeletal: Musculoskeletal pain (37%), tremor (38%)
Renal: Renal insufficiency (18%)
Respiratory: Cough (38%), dyspnea (24%), hypoxia (40%), pleural effusion (21%)
Miscellaneous: Fever (94%)
1% to 10%:
Cardiovascular: Bradycardia (10%), cardiac arrhythmia (10%; non-ventricular)
Endocrine & metabolic: Dehydration (6%), hypokalemia (grade 3/4: 10%)
Gastrointestinal: Dysphagia (10%), xerostomia (7%)
Hematologic & oncologic: Disorder of hemostatic components of blood (10%; grade ≥3: 2%), febrile neutropenia (6%), hemorrhage (7%)
Infection: Fungal infection (9%)
Nervous system: Ataxia (7%), increased intracranial pressure (2%), seizure (5%)
Respiratory: Pulmonary edema (4%), respiratory failure (6%)
Frequency not defined: Immunologic: Antibody development
Related/similar drugs
Revlimid
Revlimid is used to treat types of multiple myeloma, mantle cell lymphoma, follicular lymphoma and ...
Otrexup
Otrexup is used for polyarticular juvenile idiopathic arthritis, psoriasis, rheumatoid arthritis
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Dasatinib
Dasatinib is used to treat Philadelphia chromosome-positive chronic myelogenous leukemia (CML) ...
Lenalidomide
Lenalidomide (Revlimid) is used to treat multiple myeloma, mantle cell lymphoma, follicular ...
Doxorubicin
Doxorubicin systemic is used for acute lymphoblastic leukemia, acute myeloblastic leukemia, bladder ...
Imatinib
Imatinib is used to treat certain types of leukemia, bone marrow disorders, and skin cancer ...
Mercaptopurine
Mercaptopurine systemic is used for acute lymphoblastic leukemia, autoimmune hepatitis, crohn's ...
Gleevec
Gleevec is targeted cancer therapy for specific types of leukemia (blood cancer), bone marrow ...
ALERT: U.S. Boxed Warning
Cytokine release syndromeCytokine release syndrome (CRS), including life-threatening reactions, occurred in patients receiving brexucabtagene autoleucel. Do not administer brexucabtagene autoleucel to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids.
Neurologic toxicitiesNeurologic toxicities, including life-threatening reactions, occurred in patients receiving brexucabtagene autoleucel, including concurrently with CRS or after CRS resolution. Monitor for neurologic toxicities after treatment with brexucabtagene autoleucel. Provide supportive care and/or corticosteroids as needed.
REMS programBrexucabtagene autoleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the YESCARTA and TECARTUS REMS Program.
Warnings/Precautions
Concerns related to adverse effects:
• Cytokine release syndrome: [US Boxed Warning]: Cytokine release syndrome (CRS), including life-threatening reactions, occurred in patients receiving brexucabtagene autoleucel. Do not administer brexucabtagene autoleucel to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids. CRS occurred in the majority of patients receiving brexucabtagene autoleucel; grade 3 and higher events were reported, including a fatal CRS event. The median time to onset of CRS was 3 days (range: 1 to 13 days); the median duration of CRS was 10 days (range: 1 to 50 days). Key manifestations of CRS include fever, hypotension, hypoxia, chills, tachycardia, headache, fatigue, nausea, AST or ALT increases, and diarrhea; acute kidney injury may also occur. Ensure that tocilizumab is available (a minimum of 2 doses for each patient) on site prior to brexucabtagene autoleucel infusion. Monitor for signs or symptoms of CRS for at least 4 weeks after treatment (monitor daily at the health care facility for the first 7 days following the infusion). Patients should seek immediate medical attention if signs or symptoms of CRS occur at any time. Evaluate patients immediately at the first sign of CRS; begin supportive care, tocilizumab, and/or corticosteroids as indicated.
• Cytopenias: Prolonged cytopenias may occur for several weeks after lymphodepleting chemotherapy and brexucabtagene autoleucel infusion. Unresolved (by day 30 following brexucabtagene autoleucel treatment) grade 3 and 4 cytopenias included thrombocytopenia, neutropenia, and anemia. Monitor blood counts.
• Hepatitis B virus reactivation: Hepatitis B virus (HBV) reactivation (sometimes resulting in fulminant hepatitis, hepatic failure, and death) can occur in patients treated with medications directed against B cells. Screen for HBV, hepatitis C virus, and HIV in accordance with clinical guidelines prior to collection of cells for manufacturing.
• Hypersensitivity: Serious hypersensitivity reactions, including anaphylaxis, may occur due to the dimethyl sulfoxide or residual gentamicin in brexucabtagene autoleucel.
• Hypogammaglobulinemia: Hypogammaglobulinemia and B-cell aplasia may occur in patients receiving brexucabtagene autoleucel. Monitor immunoglobulin levels after brexucabtagene autoleucel treatment. Manage hypogammaglobulinemia with infection precautions, antibiotic prophylaxis, and immunoglobulin replacement treatment (per standard replacement guidelines).
• Infection: Serious infections (including life-threatening infections) have occurred. Infections occurred in ~50% of patients after brexucabtagene autoleucel infusion, including grades 3 and higher infections in 30% of patients. Bacterial, viral, and fungal infections were reported. Begin prophylaxis according to local guidelines prior to brexucabtagene autoleucel infusion. Monitor for signs and symptoms of infection before and following treatment and manage appropriately; do not administer to patients with clinically significant active systemic infections. Neutropenic fever has been observed after brexucabtagene autoleucel infusion and may occur concurrently with CRS. If neutropenic fever occurs, evaluate for infection and manage with broad-spectrum antibiotics, fluids, and other supportive care as clinically indicated.
• Neurologic toxicities: [US Boxed Warning]: Neurologic toxicities, including life-threatening reactions, occurred in patients receiving brexucabtagene autoleucel, including concurrently with CRS or after CRS resolution. Monitor for neurologic toxicities after treatment with brexucabtagene autoleucel. Provide supportive care and/or corticosteroids as needed. Neurologic events occurred in ~80% of patients receiving brexucabtagene autoleucel; grade 3 or higher events were observed. The median time to onset was 6 days (range: 1 to 32 days). The median duration of neurologic toxicities was 21 days (range: 2 to 454 days) in most patients; neurologic toxicity resolved in close to 80% of patients, although persisted (usually at grade 1 or 2) in some patients. Over one-half of patients experienced CRS before neurologic toxicity onset; some patients did not experience CRS with neurologic events, and others developed neurological events after CRS resolution. The majority of patients experienced the first CRS or neurological events within the first 7 days after brexucabtagene autoleucel infusion. The most common neurologic events were encephalopathy, headache, tremor, aphasia, and delirium; serious events included encephalopathy, aphasia, and seizures. Monitor for signs or symptoms of neurologic toxicities for at least 4 weeks after treatment (monitor daily at the healthcare facility for the first 7 days following the infusion). Treat promptly if neurologic toxicities occur. Due to the potential for neurologic events, including altered mental status or seizures, patients receiving brexucabtagene autoleucel are at risk for altered or decreased consciousness or coordination in the 8 weeks following administration; during this initial period, advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery.
• Secondary malignancy: Patients treated with brexucabtagene autoleucel may develop secondary malignancies. Monitor (life-long) for secondary malignancies. If a secondary malignancy occurs, contact the manufacturer (1-844-454-5483) to obtain patient sampling instructions for testing.
Concurrent drug therapy issues:
• Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
• Immunizations: Vaccination with live virus vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during brexucabtagene autoleucel treatment, and until immune recovery following treatment. The safety of immunization with live viral vaccines during or following brexucabtagene autoleucel treatment has not been studied.
Other warnings/precautions:
• Appropriate use: For autologous use only. Confirm patient identity and match to patient identifiers on the cassette and infusion bag prior to infusion. Administer in a health care facility; patients should remain within proximity of the facility for at least 4 weeks after infusion.
• REMS program: [US Boxed Warning]: Brexucabtagene autoleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the YESCARTA and TECARTUS REMS. Information is available at https://www.YescartaTecartusREMS.com or 1-844-454-5483.
Monitoring Parameters
Screen for hepatitis B virus, hepatitis C virus, and HIV (prior to collection of cells for manufacturing). Monitor immunoglobulin levels and blood counts (after treatment). Evaluate pregnancy status prior to use in females of reproductive potential.
Monitor for signs/symptoms of cytokine release syndrome (CRS) and neurological toxicities for at least 4 weeks after treatment (monitor daily for the first 7 days after infusion at the health care facility; patients with ≥ grade 2 CRS or ≥ grade 2 neurologic toxicity should be monitored with continuous cardiac telemetry and pulse oximetry), monitor for hypersensitivity reactions and for signs/symptoms of infection or neutropenic fever. Monitor (life-long) for secondary malignancies.
Reproductive Considerations
Evaluate pregnancy status prior to use in females of reproductive potential. Females of reproductive potential who are sexually active should have a negative pregnancy test prior to initiating brexucabtagene autoleucel therapy. Consider contraception recommendations of concomitant therapy; the duration of effective contraception specific to brexucabtagene autoleucel treatment is not known.
Pregnancy Considerations
Based on the mechanism of action, in utero exposure to brexucabtagene autoleucel may cause fetal harm.
Patient Education
What is this drug used for?
• It is used to treat a type of lymphoma.
• This drug may be used with other drugs to treat your health condition. If you are also taking other drugs, talk with your doctor about the risks and side effects that may happen.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Headache
• Constipation, diarrhea, stomach pain, upset stomach, throwing up, or feeling less hungry.
• Feeling dizzy, tired, or weak
• Pain in arms or legs
• Back, muscle, or joint pain
• Muscle spasm
• Muscle weakness
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Cytokine release syndrome like chills, dizziness, feeling tired or weak, fever, headache, passing out, rash, swelling of the face, trouble breathing, upset stomach, throwing up, or wheezing
• Nervous system problems like agitation, confusion, restlessness, anxiety, change in eyesight, dizziness or passing out, hallucinations (seeing or hearing things that are not there), headaches, seizures, shakiness, trouble speaking, or new or worse behavior or mood changes
• Infection
• Bleeding like throwing up or coughing up blood; vomit that looks like coffee grounds; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a cause or that get bigger; or bleeding you cannot stop
• Kidney problems like unable to pass urine, change in how much urine is passed, blood in the urine, or a big weight gain
• High or low blood pressure like very bad headache, dizziness, passing out, or change in eyesight
• Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, a heartbeat that does not feel normal, very bad dizziness or passing out, fast heartbeat, more thirst, seizures, feeling very tired or weak, not hungry, unable to pass urine or change in the amount of urine produced, dry mouth, dry eyes, or very bad upset stomach or throwing up
• Feeling very tired or weak
• Fast, slow, or abnormal heartbeat
• Trouble sleeping
• Feeling very sleepy
• Not able to focus
• Memory problems or loss
• Swelling
• Trouble moving around
• Burning, numbness, or tingling feeling that is not normal
• Blood clot like chest pain or pressure; coughing up blood; shortness of breath; swelling, warmth, numbness, change of color, or pain in a leg or arm; or trouble speaking or swallowing
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine’s uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
More about brexucabtagene autoleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.