Brexucabtagene Autoleucel Dosage
Medically reviewed by Drugs.com. Last updated on Mar 5, 2025.
Usual Adult Dose for:
Additional dosage information:
Usual Adult Dose for Lymphoma
PRETREATMENT: Administer a lymphodepleting chemotherapy regimen of cyclophosphamide 500 mg/m2 IV and fludarabine 30 mg/m2 IV on each of the fifth, fourth, and third days before infusing this drug.
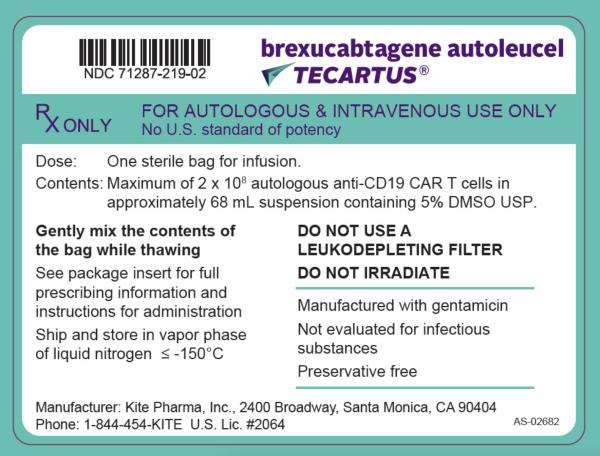
Each single infusion bag contains a suspension of chimeric antigen receptor (CAR)-positive T cells in approximately 68 mL; the dose is 2 x 10(6) CAR-positive viable T cells/kg, with a maximum of 2 x 10(8) CAR-positive viable T cells
Comments:
- Premedicate with acetaminophen and diphenhydramine or another H1-antihistamine approximately 30 to 60 minutes prior to infusing this drug.
- Avoid prophylactic use of systemic corticosteroids as it may interfere with the activity of this drug.
Use: For the treatment of adult patients with relapsed or refractory mantle cell lymphoma (MCL)
Renal Dose Adjustments
Data not available
Liver Dose Adjustments
Data not available
Dose Adjustments
Management of Severe Adverse Reactions Cytokine Release Syndrome:
- Identify CRS based on clinical presentation.
- Evaluate for and treat other causes of fever, hypoxia, and hypotension.
- If CRS is suspected, manage according to recommendations.
- Patients who experience Grade 2 or higher CRS (e.g., hypotension, not responsive to fluids, or hypoxia requiring supplemental oxygenation) should be monitored with continuous cardiac telemetry and pulse oximetry. For patients experiencing severe CRS, consider performing an echocardiogram to assess cardiac function. For severe or life-threatening CRS, consider intensive care supportive therapy.
CRS GRADING AND MANAGEMENT GUIDANCE:
- GRADE 1 (symptoms require symptomatic treatment only (e.g., fever, nausea, fatigue, headache, myalgia, malaise): If not improving after 24 hours, administer tocilizumab at 8 mg/kg IV over 1 hour (not to exceed 800 mg); do not administer corticosteroids.
- GRADE 2 (symptoms require and respond to moderate intervention; oxygen requirement less than 40% FiO2 or hypotension responsive to fluids or low dose of one vasopressor or Grade 2 organ toxicity: Administer tocilizumab at 8 mg/kg IV over 1 hour (not to exceed 800 mg; repeat every 8 hours as needed if not responsive to IV fluids or increasing supplemental oxygen; limit to a maximum of 3 doses in 24 hours; maximum total of 4 doses if no improvement in CRS; if improving discontinue tocilizumab; corticosteroids: Manage per Grade 3 if no improvement within 24 hours after starting tocilizumab; if improving, taper corticosteroids.
- GRADE 4 (life-threatening symptoms; requirements for ventilator support or continuous venovenous hemodialysis [CVVHD], or Grade 4 organ toxicity (excluding transaminitis): Administer tocilizumab at 8 mg/kg IV over 1 hour (not to exceed 800 mg; repeat every 8 hours as needed if not responsive to IV fluids or increasing supplemental oxygen; limit to a maximum of 3 doses in 24 hours; maximum total of 4 doses if no improvement in CRS; if improving discontinue tocilizumab; corticosteroids: Administer methylprednisolone 1000 mg IV daily for 3 days; if improving, taper corticosteroids and manage as Gr manage as Grade 3; if not improving, consider alternate immunosuppressants.
TABLE 2:
NEUROLOGIC TOXICITY:
- Monitor patients for neurologic toxicities.
- Rule out other causes of neurologic symptoms.
- Patients who experience Grade 2 or higher neurologic toxicities should be monitored with continuous cardiac telemetry and pulse oximetry.
- Provide intensive care supportive therapy for severe or life-threatening neurologic toxicities.
- Consider non-sedating antiseizure medicines (e.g., levetiracetam) for seizure prophylaxis for any Grade 2 or higher neurologic toxicities.
GRADE 1 (e.g., mild somnolence, confusion, encephalopathy [mild limiting of ADLs], dysphasia [not impairing ability to communicate]):
- With concurrent CRS: Administer tocilizumab per Table 1 for management of Grade 1 CRS.
- No concurrent CRS: Initiate supportive care.
- With concurrent CRS: Administer tocilizumab per Table 1 for management of Grade 2 CRS; if not improving within 24 hours after starting tocilizumab, administer dexamethasone 10 mg IV every 6 hours until the event is Grade 1 or less, then taper corticosteroids; if improving, discontinue tocilizumab; if still not improving, manage as Grade 3; consider non-sedating, antiseizure medicines (e.g., levetiracetam) for seizure prophylaxis.
- No concurrent CRS: Administer dexamethasone 10 mg IV every 6 hours until Grade 1 or less; if improving taper corticosteroids; consider non-sedating, antiseizure medicines (e.g., levetiracetam) for seizure prophylaxis.
- With concurrent CRS: Administer tocilizumab per Table 1 for management of Grade 2 CRS; administer dexamethasone 10 mg IV with the first dose of tocilizumab and repeat dose every 6 hours; continue dexamethasone use until the event is Grade 1 or less, then taper corticosteroids; if improving, discontinue tocilizumab and manage as Grade 2; if still not improving, manage as Grade 4; consider non-sedating, antiseizure medicines (e.g., levetiracetam) for seizure prophylaxis.
- No concurrent CRS: Administer dexamethasone 10 mg IV every 6 hours; continue dexamethasone use until the event is Grade 1 or less, then taper corticosteroids; if not improving, manage as Grade 4; consider non-sedating, antiseizure medicines (e.g., levetiracetam) for seizure prophylaxis.
- With concurrent CRS: Administer tocilizumab per Table 1 for management of Grade 2 CRS; administer methylprednisolone 1000 mg IV daily with first dose of tocilizumab and continue methylprednisolone 1000 mg IV daily for 2 more days; if improving, then manage as Grade 3; if not improving, consider alternate immunosuppressants; consider non-sedating, antiseizure medicines (e.g., levetiracetam) for seizure prophylaxis.
- No concurrent CRS: Administer methylprednisolone 1000 mg IV daily for 3 days; if improving, then manage as Grade 3; if not improving, consider alternate immunosuppressants; consider non-sedating, antiseizure medicines (e.g., levetiracetam) for seizure prophylaxis.
Precautions
The US FDA requires a Risk Evaluation and Mitigation Strategy (REMS) for Tecartus called the YESCARTA and TECARTUS REMS Program. Further information is available at www.YescartaTecartusREMS.com or 1-844-454-KITE (5483).
US BOXED WARNINGS:
CYTOKINE RELEASE SYNDROME (CRS):
- CRS, sometimes fatal, has been reported.
- Do not administer this drug to patients with active infection or inflammatory disorders.
- Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids
- Neurologic toxicities, sometimes fatal, have been reported, including concurrently with CRS or after CRS resolution.
- Monitor for neurologic toxicities.
- Provide supportive care and/or corticosteroids as needed.
- The US FDA requires a REMS for this drug. The required components of the YESCARTA and TECARTUS REMS Program are:
- Healthcare facilities that dispense and administer this drug must be enrolled and comply with the REMS requirements. Certified healthcare facilities must have on-site, immediate access to tocilizumab, and ensure that a minimum of two doses of tocilizumab are available for each patient for infusion within two hours after TECARTUS infusion, if needed for treatment of CRS.
- Certified healthcare facilities must ensure that healthcare providers who prescribe, dispense, or administer this drug are trained in the management of CRS and neurologic toxicities.
- Further information is available at www.YescartaTecartusREMS.com or 1-844-454-KITE (5483).
CONTRAINDICATIONS:
- None
Safety and efficacy have not been established in patients younger than 18 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
PREPARATION FOR INFUSION:
- Verify that the patient's identity (ID) matches the patient identifiers on the metal cassette.
- The infusion bag should not be removed from the metal cassette if the information on the patient-specific label does not match the intended patient.
- When the patient ID is confirmed, remove the infusion bag from the metal cassette.
- Check that the patient information on the metal cassette label matches that on the bag label.
- Inspect the infusion bag for any breaches of container integrity before thawing; if the bag is compromised, follow the local guidelines for handling of waste of human-derived material.
- Place the infusion bag inside a second bag.
- Thaw drug at approximately 37C using either a water bath or dry thaw method until there is no visible ice in the infusion bag. Gently mix the contents of the bag to disperse clumps of cellular material. If visible cell clumps remain, continue to gently mix the contents of the bag. Small clumps of cellular material should disperse with gentle manual mixing. This drug should not be washed, spun down, and/or resuspended in new media prior to infusion. Thawing should take approximately 3 to 5 minutes.
- When thawed, this drug is stable at room temperature (20°C to 25°C) for up to 3 hours; however, the infusion should begin within 30 minutes of thaw completion.
- For autologous single use only.
- Tocilizumab and emergency equipment should be available prior to infusion and during the monitoring period.
- A leukodepleting filter must not be used.
- Central venous access is recommended for the administration.
- Verify the patient ID again to match the patient identifiers on the bag.
- Prime the tubing with sodium chloride 9 mg/mL (0.9%) solution for injection (0.154 mmol sodium per mL) prior to infusion.
- Infuse the entire content of the bag within 30 minutes by either gravity or a peristaltic pump.
- Gently agitate the bag during infusion to prevent cell clumping.
- After the entire content of the bag is infused, rinse the tubing at the same infusion rate with sodium chloride 9 mg/mL (0.9%) solution for injection (0.154 mmol sodium per mL) to ensure all the treatment is delivered.
Storage requirements:
- This drug should be stored in the vapor phase of liquid nitrogen (-150C or lower) and must remain frozen until the patient is ready for treatment to ensure viable live autologous cells are available for patient administration.
IV compatibility:
- Compatible with sodium chloride 0.9%.
General:
- This drug product contains genetically modified human blood cells. Healthcare professionals handling this drug should take appropriate precautions (wearing gloves and glasses) to avoid potential transmission of infectious diseases.
- To ensure traceability the name of the product, the batch number and the name of the treated patient should be kept for 30 years.
- Warnings and precautions of lymphodepleting chemotherapy should be considered.
Reasons to Delay Therapy:
- Due to the risks associated with this drug, therapy should be delayed if a patient has any of the following conditions:
- Unresolved serious adverse reactions (e.g., pulmonary reactions, cardiac reactions, hypotension) including from preceding chemotherapies.
- Active uncontrolled infection or inflammatory disease.
- Active graft-versus-host disease (GvHD).
- In some cases, therapy may be delayed after administration of the lymphodepleting chemotherapy regimen.
- If the infusion is delayed for more than 2 weeks after the patient has received the lymphodepleting chemotherapy, lymphodepleting chemotherapy regimen should be administered again.
Monitoring:
- Screening for HBV, HCV, and HIV should be performed before collection of cells for manufacturing of the final product.
Frequently asked questions
More about brexucabtagene autoleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (3)
- Side effects
- During pregnancy
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.