Vemurafenib (Monograph)
Brand name: Zelboraf
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; an inhibitor of b-Raf serine-threonine kinase with V600E mutation (BRAF V600E).
Uses for Vemurafenib
Melanoma
Treatment of unresectable or metastatic melanoma with BRAF V600E mutation (designated an orphan drug by FDA for this use).
FDA-approved in vitro diagnostic test (e.g., cobas 4800 BRAF V600 Mutation Test) required to confirm presence of BRAF V600E mutation prior to initiation of therapy.
Not indicated for use in patients with wild-type BRAF melanoma; safety and efficacy not established.
American Society of Clinical Oncology (ASCO) states that ipilimumab plus nivolumab, nivolumab alone, pembrolizumab alone, or combination BRAF/MEK inhibitor therapy (e.g., dabrafenib-trametinib, encorafenib-binimetinib, vemurafenib-cobimetinib) may be offered to patients with BRAF V600 mutation-positive cutaneous melanoma. For patients who progress on first-line programmed-death receptor-1 (PD-1) inhibitor therapy, combination BRAF/MEK inhibitor therapy may be offered. For patients who progress on first-line combination BRAF/MEK inhibitor therapy, PD-1 inhibitor therapy may be offered. Patients with mucosal melanoma may be offered the same treatment regimens as those recommended for cutaneous melanoma.
Erdheim-Chester Disease
Treatment of Erdheim-Chester disease with BRAF V600 mutation (designated an orphan drug by FDA for this use).
BRAF or MEK inhibitors have been used in the first-line setting in patients with life-threatening cases (e.g., CNS or cardiac involvement) of Erdheim-Chester disease. The most frequent second-line systemic therapy or salvage therapy for Erdheim-Chester disease includes BRAF or MEK inhibitors.
Hairy Cell Leukemia
Based on current evidence, vemurafenib, either as monotherapy or in combination with rituximab, as a treatment for relapsed/refractory hairy cell leukemia in patients with a confirmed BRAF V600E kinase-activating mutation† [off-label] has Level 2 (moderate strength/quality) evidence supporting its use. Vemurafenib therapy results in an improvement in response in these patients with a tolerable safety profile.
Vemurafenib Dosage and Administration
General
Pretreatment Screening
-
Presence of the BRAF V600E mutation must be confirmed prior to initiation of therapy.
-
Obtain ECGs and serum electrolyte concentrations (i.e., potassium, magnesium, calcium) prior to initiation of therapy.
-
Evaluate liver enzymes and bilirubin concentrations prior to initiation of therapy.
-
Evaluate Scr concentrations at baseline.
-
Perform a dermatologic evaluation prior to initiation of therapy.
Patient Monitoring
-
Perform a dermatologic evaluation every 2 months during therapy. Consider continuing monitoring for 6 months following discontinuance of vemurafenib. Closely monitor for signs and symptoms of development of new non-cutaneous squamous cell carcinoma or of other primary malignancies.
-
Evaluate Scr concentrations periodically during therapy.
-
Closely monitor patients receiving vemurafenib concomitantly or sequentially with radiation therapy for signs and symptoms of radiation sensitization or recall.
-
Monitor CBC in patients with Erdheim-Chester disease and coexisting myeloid malignancies.
-
Monitor for signs and symptoms of uveitis.
-
Monitor ECG and serum electrolytes (i.e., potassium, magnesium, calcium) 15 days following initiation of therapy or dosage modification for QT interval prolongation, monthly during the first 3 months of therapy, and then every 3 months thereafter or more often as clinically indicated.
-
Monitor liver enzymes and bilirubin monthly during treatment.
Other General Considerations
-
Advise patients to avoid sun exposure.
Administration
Oral Administration
Administer orally twice daily without regard to meals.
Do not crush or chew tablets.
If a dose is missed, it may be taken up to 4 hours prior to next dose. Do not take 2 doses at the same time.
If vomiting occurs following administration, do not take a replacement dose. Administer next dose at regularly scheduled time.
Dosage
Adults
Melanoma
Oral
960 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
If concomitant use with potent inducers of CYP3A4 cannot be avoided, increase vemurafenib dosage.
If concomitant use with potent inhibitor of CYP3A4 cannot be avoided, consider reducing vemurafenib dosage, if clinically indicated.
Erdheim-Chester Disease
Oral
960 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
In the principal efficacy study, dosage reductions to 480 or 720 mg twice daily required in 64 or 36% of patients, respectively.
If concomitant use with potent inducers of CYP3A4 cannot be avoided, increase vemurafenib dosage.
If concomitant use with potent inhibitor of CYP3A4 cannot be avoided, consider reducing vemurafenib dosage, if clinically indicated.
Hairy Cell Leukemia† [off-label]
Oral
960 mg orally twice daily for a minimum of 8 weeks, and if a complete response does not occur, a maximum of 24 weeks.
Dosage Modification for General Toxicity
Oral
If intolerable grade 2 or 3 toxicity occurs, temporarily interrupt vemurafenib therapy. When toxicity resolves or improves to grade 1 or less, resume therapy at a reduced dosage of 720 mg twice daily.
If toxicity recurs at a dosage of 720 mg twice daily, temporarily interrupt therapy again until toxicity resolves to grade 1 or less, and resume therapy at a reduced dosage of 480 mg twice daily.
If grade 4 toxicity occurs, permanently discontinue or temporarily interrupt therapy until toxicity resolves to grade 1 or less, and resume therapy at a reduced dosage of 480 mg twice daily if clinically appropriate.
If toxicity recurs at a reduced dosage of 480 mg twice daily, permanently discontinue vemurafenib. Dosages <480 mg twice daily not recommended.
Dosage Modification for Prolongation of QT Interval
Oral
If the corrected QT interval (QTc) is >500 msec, temporarily interrupt vemurafenib therapy.
When QTc interval returns to ≤500 msec, resume therapy at a reduced dosage.
If QTc interval >500 msec and increases >60 msec from baseline despite correction of electrolyte abnormalities and control of other risk factors (e.g., CHF, bradyarrhythmias), permanently discontinue vemurafenib.
Dosage Modification for Development of New Primary Cutaneous Malignancies
Oral
No dosage adjustment necessary.
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment: No initial dosage adjustment required.
Renal Impairment
Mild or moderate renal impairment: No initial dosage adjustment required.
Geriatric Patients
No specific dosage adjustment recommendations at this time.
Cautions for Vemurafenib
Contraindications
-
None.
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Serious hypersensitivity reactions (e.g., anaphylaxis, generalized rash, erythema, hypotension, drug reaction with eosinophilia and systemic symptoms [DRESS syndrome]) reported during and upon reinitiation of therapy. Permanently discontinue vemurafenib in patients who experience a severe hypersensitivity reaction.
Photosensitivity Reactions
Risk of photosensitivity reactions. Reduce dosage of vemurafenib in patients who experience intolerable grade 2 or greater reaction.
Other Warnings and Precautions
Development of New Primary Malignancies
Cutaneous squamous cell carcinoma, keratoacanthoma, and melanoma reported. First appearance of cutaneous squamous cell carcinoma occurred within 7–8 weeks after initiating vemurafenib in patients with unresectable or metastatic melanoma; patients with more than one occurrence reported time between occurrences of approximately 6 weeks. Median time to first appearance of cutaneous squamous cell carcinoma was 12.1 weeks after initiating vemurafenib in patients with Erdheim-Chester disease. Possible risk factors include advanced age (i.e., ≥65 years of age), history of skin cancer, and chronic sun exposure.
Non-cutaneous squamous cell carcinoma of the head and neck (e.g., oropharyngeal area) reported. Progression of a preexisting chronic myelomonocytic leukemia with NRAS mutation also reported during postmarketing experience.
Perform dermatologic evaluation at baseline and every 2 months during therapy. May consider monitoring for 6 months following discontinuance of vemurafenib. Initiate appropriate therapy and excise suspicious cutaneous lesions for pathologic evaluation. Closely monitor for signs and symptoms of development of new non-cutaneous squamous cell carcinoma or other primary malignancies.
Myeloid neoplasms reported in patients with Erdheim-Chester disease receiving vemurafenib therapy. Monitor CBC in patients with Erdheim-Chester disease and coexisting myeloid malignancies.
Tumor Promotion in BRAF Wild-Type Melanoma
In vitro, paradoxical activation of mitogen-activated protein kinase (MAPK) signaling and increased cell proliferation observed in wild-type BRAF cells exposed to BRAF inhibitors. Confirm presence of BRAF V600E mutation prior to initiation of therapy.
Dermatologic Effects
Severe skin reactions (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis) reported. Permanently discontinue vemurafenib in patients who experience severe skin reactions.
Prolongation of QT Interval
QT prolongation reported.
Do not use in patients with congenital long QT syndrome, electrolyte disturbances unresponsive to corrective measures, or QTc intervals >500 msec.
Avoid concomitant use with drugs known to prolong QT interval (e.g., class Ia and III antiarrhythmic agents).
Obtain ECG and serum electrolytes at baseline or following dosage modification for QT prolongation; monitor at 15 days after initiating vemurafenib, then monthly for the first 3 months, and every 3 months thereafter or more often as clinically indicated.
Interruption or discontinuance of vemurafenib may be necessary if increases in the QTc interval occur.
Hepatic Effects
Hepatic injury may occur resulting in functional hepatic impairment, including coagulopathy or other organ dysfunction. Elevations in ALT, AST, bilirubin, and alkaline phosphatase concentrations of grade 3 or 4 severity reported in 0.9–2.9% of patients.
Monitor serum aminotransferase, bilirubin, and alkaline phosphatase concentrations at baseline and then monthly thereafter.
If laboratory abnormalities occur, reduce dosage, temporarily interrupt, or discontinue vemurafenib therapy.
Safety and efficacy of vemurafenib used concomitantly with ipilimumab not established; however, grade 3 elevations in aminotransferase and bilirubin concentrations reported in patients receiving vemurafenib (720 or 960 mg twice daily) concurrently with ipilimumab (3 mg/kg).
Ocular Effects
Uveitis (including iritis), blurry vision, and photophobia reported. Monitor patients for signs and symptoms of uveitis. If uveitis occurs, treatment with ophthalmic corticosteroid and mydriatic preparations may be required.
Retinal vein occlusion also reported.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm.
Vemurafenib crossed the placenta in animal studies.
Advise women of childbearing potential to use effective contraception during therapy and for 2 weeks after the last dose. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Radiation Sensitization and Recall
Radiation sensitization and recall, sometimes severe or fatal, reported in patients receiving vemurafenib prior to, during, or subsequent to radiation therapy. May involve cutaneous and visceral organs; fatal cases reported in patients with radiation sensitization or recall involving visceral organs.
Closely monitor patients receiving vemurafenib concomitantly or sequentially with radiation therapy for signs and symptoms of radiation sensitization or recall.
Renal Effects
Renal failure, including acute interstitial nephritis and acute tubular necrosis, reported.
Evaluate Scr concentrations at baseline and periodically during therapy.
Dupuytren Contracture and Plantar Fascial Fibromatosis
Dupuytren contracture and plantar fascial fibromatosis reported. Severity is usually mild to moderate, but severe and disabling cases have occurred.
Specific Populations
Pregnancy
May cause fetal harm.
Lactation
Not known whether vemurafenib is distributed into human milk. Effects on breast-fed infants and milk production also unknown. Discontinue nursing during therapy and for 2 weeks after the last dose.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Limited data indicate similar steady-state exposures of vemurafenib in pediatric patients (range: 15–17 years of age) and adults. Maximum tolerated dosage not established; however, no new adverse effects observed in pediatric patients receiving a vemurafenib dosage up to 960 mg twice daily.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults.
Hepatic Impairment
Not studied in patients with severe hepatic impairment; use with caution.
Renal Impairment
Not studied in patients with severe renal impairment; use with caution.
Common Adverse Effects
Melanoma (≥10%): Arthralgia, rash, alopecia, fatigue, photosensitivity reaction, nausea, pruritus, cutaneous squamous cell carcinoma, skin papilloma.
Erdheim-Chester Disease (≥20%): Arthralgia, maculopapular rash, alopecia, fatigue, QT interval prolongation, skin papilloma, diarrhea, hyperkeratosis, dry skin, palmar-plantar erythrodysesthesia syndrome, photosensitivity reaction, seborrheic keratosis, cough, cutaneous squamous cell carcinoma, hypertension, pruritus, peripheral sensory neuropathy, actinic keratosis, keratosis pilaris, nausea, melanocytic nevus, sunburn, papular rash, vomiting.
Drug Interactions
Vemurafenib is a moderate inhibitor of CYP1A2, and a weak inhibitor of 2D6 in vivo. Vemurafenib inhibits CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, and 3A4/5 in vitro. The drug also is an inhibitor and substrate of CYP3A4.
Vemurafenib is a substrate and inhibitor of P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP).
Drugs and Foods Affecting Hepatic Microsomal Enzymes
Potent CYP3A4 inhibitors: Possible pharmacokinetic interaction (increased plasma concentrations of vemurafenib and increased incidence of adverse effects). Avoid concomitant use. If coadministration of a potent CYP3A4 inhibitor cannot be avoided, consider reducing the dosage of vemurafenib, if clinically indicated.
Potent CYP3A4 inducers: Possible pharmacokinetic interaction (decreased plasma concentrations of vemurafenib and reduced vemurafenib efficacy). Avoid concomitant use; selection of alternative drug with no or minimal CYP3A4 induction potential recommended. If concomitant therapy cannot be avoided, increase vemurafenib dosage by 240 mg twice daily (e.g., from 960 mg twice daily to 1.2 g twice daily).
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP1A2: Possible pharmacokinetic interaction (increased plasma concentrations of CYP1A2 substrate and possible toxicity). Avoid concomitant use of vemurafenib and CYP1A2 substrates with a narrow therapeutic index. If concomitant use cannot be avoided, consider dosage reduction of the CYP1A2 substrate and closely monitor for adverse effects.
Substrates of CYP2D6: Possible pharmacokinetic interaction (increased plasma concentrations of CYP2D6 substrate and possible toxicity).
Substrates of CYP3A4: Possible pharmacokinetic interaction (decreased plasma concentrations of CYP3A4 substrate and possible decreased efficacy).
Substrates of CYP2C9: Possible pharmacokinetic interaction (increased plasma concentrations of CYP2C9 substrate and possible toxicity).
Substrates of CYP2C19: No clinically important interaction reported.
Drugs Affected by Efflux Transport Systems
Substrates of P-gp: Possible pharmacokinetic interaction (increased plasma concentrations of P-gp substrate). Avoid concomitant use of vemurafenib and P-gp substrates with a narrow therapeutic index. If concomitant use cannot be avoided, consider dosage reduction of the P-gp substrate.
Drugs that Prolong QT Interval
Potential pharmacologic interaction (additive effect on QT prolongation). Avoid concomitant use.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antiarrhythmics (class Ia and III; e.g., amiodarone, procainamide, quinidine, sotalol) |
Increased risk of QT-interval prolongation |
Avoid concomitant use |
|
Antifungals, azoles (e.g., itraconazole, ketoconazole, voriconazole) |
Potent CYP3A4 inhibitors: Possible increased vemurafenib concentrations and increased adverse effects Itraconazole: Systemic exposure of vemurafenib increased by approximately 40% at steady state; magnitude of effect on peak plasma concentration was similar |
Potent CYP3A4 inhibitors: Avoid concomitant use; if coadministration cannot be avoided, consider reducing the dosage of vemurafenib, if clinically indicated |
|
Antimycobacterials, rifamycins (e.g., rifampin) |
Potent CYP3A4 inducers: Possible decreased vemurafenib concentrations and reduced vemurafenib efficacy Rifampin decreased AUC of vemurafenib by 40%; no effect on peak plasma concentrations |
Potent CYP3A4 inducers: Avoid concomitant use; select alternative agent with no or minimal enzyme induction potential If concomitant use with potent CYP3A4 inducer cannot be avoided, increase vemurafenib dosage by 240 mg twice daily (e.g., from 960 mg twice daily to 1.2 g twice daily) |
|
Antipsychotic agents that prolong QT interval (e.g., asenapine, chlorpromazine, haloperidol, olanzapine, paliperidone, pimozide, quetiapine, thioridazine, ziprasidone) |
Increased risk of QT-interval prolongation |
Avoid concomitant use |
|
Caffeine |
Increased AUC of caffeine |
CYP1A2 substrates with a narrow therapeutic index: Concomitant use not recommended; if concomitant use cannot be avoided, consider dosage reduction of CYP1A2 substrate and closely monitor patient for adverse effects |
|
Carbamazepine |
Possible decreased vemurafenib concentrations and reduced vemurafenib efficacy |
Avoid concomitant use; select alternative agent with no or minimal enzyme induction potential If concomitant use cannot be avoided, increase vemurafenib dosage by 240 mg twice daily (e.g., from 960 mg twice daily to 1.2 g twice daily) |
|
Dextromethorphan |
Increased AUC of dextromethorphan |
|
|
Digoxin |
Vemurafenib increased AUC and peak plasma concentrations of digoxin by 1.8- and 1.5-fold, respectively |
Avoid concomitant use; if concomitant use cannot be avoided, consider dosage reduction of digoxin |
|
Gatifloxacin |
Increased risk of QT-interval prolongation |
Avoid concomitant use |
|
HIV protease inhibitors (e.g., indinavir, nelfinavir, ritonavir, saquinavir) |
Potent CYP3A4 inhibitors: Possible increased vemurafenib concentrations and increased adverse effects |
Potent CYP3A4 inhibitors: Avoid concomitant use; if coadministration cannot be avoided, consider reducing the dosage of vemurafenib, if clinically indicated |
|
Ipilimumab |
Increased aminotransferase and bilirubin concentrations |
|
|
Macrolides (e.g., clarithromycin) |
Potent CYP3A4 inhibitors: Possible increased vemurafenib concentrations and increased adverse effects |
Potent CYP3A4 inhibitors: Avoid concomitant use; if coadministration cannot be avoided, consider reducing the dosage of vemurafenib, if clinically indicated |
|
Midazolam |
Decreased AUC of midazolam |
|
|
Moxifloxacin |
Increased risk of QT-interval prolongation |
Avoid concomitant use |
|
Omeprazole |
No change in systemic exposure of omeprazole |
|
|
Phenytoin |
Possible decreased vemurafenib concentrations and reduced vemurafenib efficacy |
Avoid concomitant use; select alternative agent with no or minimal enzyme induction potential If concomitant use cannot be avoided, increase vemurafenib dosage by 240 mg twice daily (e.g., from 960 mg twice daily to 1.2 g twice daily) |
|
Tetrabenazine |
Increased risk of QT-interval prolongation |
Avoid concomitant use |
|
Tizanidine |
Vemurafenib increased AUC and peak plasma concentrations of tizanidine by 4.7- and 2.2-fold, respectively |
CYP1A2 substrates with a narrow therapeutic index: Avoid concomitant use; if concomitant use cannot be avoided, consider dosage reduction of CYP1A2 substrate and closely monitor for adverse effects |
|
Warfarin |
Increased AUC of S-warfarin |
Vemurafenib Pharmacokinetics
Absorption
Bioavailability
64% at steady state.
Food
Food increases systemic exposure. Administration of a single dose of vemurafenib with a high-fat meal increases AUC by approximately fivefold and increases peak concentrations by approximately 2.5-fold.
Distribution
Extent
Fetal plasma concentrations of vemurafenib were 3–5% of maternal plasma concentrations in animals.
Not known whether vemurafenib is distributed into human milk.
Plasma Protein Binding
>99% (mainly albumin and α1-acid glycoprotein).
Elimination
Elimination Route
Excreted in feces (94%) and urine (1%).
Half-life
Approximately 57 hours.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Actions
-
Potent inhibitor of the b-Raf serine-threonine kinase with V600E mutation (BRAF V600E).
-
Approximately 40–60% of cutaneous melanomas carry a BRAF mutation. Most common BRAF mutation is the substitution of glutamic acid for valine at codon 600 in exon 15 (BRAF V600E); mutation involving substitution of lysine for valine at codon 600 in exon 15 (BRAF V600K) occurs less frequently.
-
Mutation of BRAF V600E activates the mitogen-activated protein kinase (MAPK) and extracellular-signal regulated kinase (ERK) signal transduction pathway, which enhances cell proliferation and tumor progression (e.g., metastasis).
-
Combination therapy with a BRAF inhibitor (i.e., dabrafenib, encorafenib, vemurafenib) and an MEK inhibitor (i.e., binimetinib, cobimetinib, trametinib) results in complete inhibition of the MAPK/ERK pathway.
-
Inhibits c-Raf, a-Raf, wild-type b-RaF, SRMS, ACK1, MAP4K5, and FGR at similar concentrations in which inhibition of BRAF V600E occurs.
Advice to Patients
-
Importance of advising patient to read the manufacturer’s medication guide before beginning treatment and each time the prescription is refilled.
-
Instruct patients to take a missed dose as soon as it is remembered, but only if it can be taken at least 4 hours before the next scheduled dose.
-
If vomiting occurs following administration, take the next dose at the regularly scheduled time. Do not take an additional dose.
-
Importance of women informing clinicians if they are or plan to become pregnant. Vemurafenib may cause fetal harm. Necessity of advising women of childbearing potential to use effective contraception during therapy and for 2 weeks after the last dose.
-
Importance of women informing clinicians if they plan to breast-feed. Necessity of advising women not to breast-feed during therapy and for 2 weeks after the last dose.
-
Importance of confirming that patients have melanomas testing positive for the BRAF V600E mutation using the cobas 4800 BRAF V600 Mutation Test or other FDA-approved diagnostic test prior to initiation of therapy.
-
Risk of new primary cutaneous malignancies. Importance of contacting clinician promptly if dermatologic changes (e.g., new wart, skin sore or reddish bump that bleeds or does not heal, or mole that changes in size or color) occur.
-
Risk of mild to severe photosensitivity reactions. Importance of using sunscreen and lip balm (minimum SPF >30), wearing protective clothing, and avoiding sun exposure during therapy.
-
Risk of severe adverse dermatologic effects. Importance of contacting clinician promptly if skin rash occurs with symptoms such as redness or swelling of face, hands, or soles of feet; blisters on skin or in mouth; peeling of skin; fever.
-
Risk of QT-interval prolongation, which may result in ventricular arrhythmias. Importance of contacting clinician promptly if an abnormal heartbeat or feelings of dizziness or faintness occur.
-
Risk of new primary malignant melanoma. Importance of contacting clinician promptly if skin changes occur.
-
Risk of anaphylaxis or other serious hypersensitivity reactions during or upon reinitiation of therapy. Importance of advising patients to promptly notify their clinician if they develop any signs or symptoms of an allergic reaction during therapy (e.g., rash, angioedema, difficulty breathing, tachycardia, throat tightness, hoarseness).
-
Risk of hepatic injury resulting in functional hepatic impairment. Importance of advising patients to schedule periodic laboratory monitoring for hepatotoxicity and to report clinically relevant symptoms to their clinician.
-
Risk of adverse ocular effects. Importance of monitoring and contacting clinician promptly if ocular pain, swelling, redness, or blurred vision occurs.
-
Risk of radiation sensitization and recall in patients receiving vemurafenib prior to, during, or subsequent to radiation therapy. Importance of informing clinician of previous or planned radiation therapy.
-
Risk of renal failure. Importance of monitoring Scr concentrations prior to and periodically during therapy.
-
Risk of Dupuytren contracture or plantar fascial fibromatosis. Importance of informing clinician if unusual thickening of palms or soles or inward tightening of the fingers occurs.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses (e.g., hepatic, renal, or cardiovascular diseases, electrolyte abnormalities) or planned surgical, dental, or other medical procedures.
-
Importance of informing patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care. For further information on the handling of antineoplastic agents, see the ASHP Guidelines on Handling Hazardous Drugs at [Web].
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Vemurafenib is available only from a designated specialty pharmacies. The manufacturer should be contacted for additional information.
|
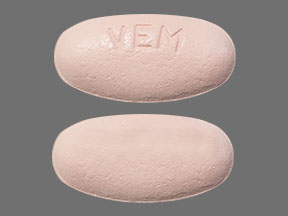
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
240 mg |
Zelboraf |
Genentech |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Zelboraf
Zelboraf (vemurafenib) is used to treat skin cancer (metastatic melanoma). Includes Zelboraf side ...
Alecensa
Alecensa (alectinib) is an oral kinase inhibitor that may be used to treat certain types of ...
Botox
Botox is used for cosmetic purposes and to treat overactive bladder symptoms, urinary incontinence ...
Alunbrig
Alunbrig (brigatinib) is used to treat anaplastic lymphoma kinase-positive (ALK+) metastatic ...
Augtyro
Augtyro (repotrectinib) is a next-generation TKI (Tyrosine Kinase Inhibitor) cancer medicine used ...
Ayvakit
Ayvakit (avapritinib) is a prescription medicine used for the treatment of gastrointestinal stromal ...
Balversa
Balversa (erdafitinib) is an oral kinase inhibitor that may be used to treat adults with locally ...
Braftovi
Braftovi is a targeted cancer treatment used in combination with Mektovi, mFOLFOX6, or Erbitux, to ...
Cabometyx
Cabometyx is used to treat advanced kidney cancer, liver cancer, thyroid cancer, and pancreatic and ...
More about vemurafenib
- Check interactions
- Compare alternatives
- Reviews (4)
- Side effects
- Dosage information
- During pregnancy
- Drug class: multikinase inhibitors
- Breastfeeding
- En español