Sotalol (Monograph)
Brand names: Betapace, Betapace AF, Sorine, Sotylize
Drug class: beta-Adrenergic Blocking Agents
Warning
-
Risk of life-threatening ventricular tachycardia associated with QT interval prolongation.
-
Initiate or reinitiate therapy (or perform conversion from IV to oral therapy) in a facility that can provide cardiac resuscitation, continuous ECG monitoring, and Clcr calculations. (See Proarrhythmic Effects under Cautions.)
-
Do not initiate sotalol if baseline QTc >450 msec. If prolongation of QT interval to ≥500 msec occurs during therapy, reduce dose, increase dosing interval, or discontinue therapy.
-
Calculate Clcr and adjust dosing interval accordingly. (See General under Dosage and Administration.)
Introduction
Nonselective β-adrenergic blocking agent; exhibits antiarrhythmic activity characteristic of class II antiarrhythmic agents and electrophysiologic effects characteristic of class III antiarrhythmic agents.
Uses for Sotalol
Ventricular Arrhythmias
Used to suppress and prevent recurrence of documented life-threatening ventricular arrhythmias (e.g., sustained ventricular tachycardia); designated an orphan drug by FDA for such use.
Shown to be effective in patients with life-threatening ventricular arrhythmias (e.g., sustained ventricular tachycardia or fibrillation) as well as those with less severe arrhythmias (e.g., premature ventricular complexes [PVCs], paired PVCs, nonsustained ventricular tachycardia)
Although antiarrhythmic drugs, including sotalol, may suppress the recurrence of arrhythmias and improve symptoms, there is no evidence from randomized controlled studies indicating that these drugs have a beneficial effect on mortality or sudden death.
Because of arrhythmogenic potential, lack of evidence for improved survival, and risk of serious adverse effects (see Proarrhythmic Effects under Cautions), use in patients with less severe arrhythmias, even if symptomatic, generally notrecommended.
Avoid treatment of asymptomatic PVCs.
Not a first-line drug of choice during cardiac arrest, but may be used for treatment of hemodynamically stable sustained monomorphic ventricular tachycardia; included in current ACLS guidelines for adult tachycardia.
Supraventricular Arrhythmias
Used to maintain normal sinus rhythm in patients with symptomatic atrial fibrillation or flutter who are currently in sinus rhythm.
Because of potential for life-threatening ventricular arrhythmias, reserve use for highly symptomatic atrial fibrillation/flutter. (See Proarrhythmic Effects under Cautions.) Do not use in patients with easily reversible (e.g., with Valsalva maneuver) paroxysmal atrial fibrillation.
Efficacy in preventing atrial fibrillation or flutter recurrences is comparable to that of quinidine or propafenone and less than that of amiodarone.
Also has been used for treatment of other supraventricular tachycardias (SVTs), including paroxysmal supraventricular tachycardia (PSVT)† [off-label] due to AV nodal reentry tachycardia (AVNRT) or AV reentry tachycardia (AVRT).
Sotalol Dosage and Administration
General
-
Initiate or reinitiate therapy and adjust dosage (or perform conversion from IV to oral therapy) in an institutional setting where patient can be monitored by personnel trained in the management of serious arrhythmias. (See Boxed Warning.)
-
Closely monitor patient for ≥3 days (or until steady-state plasma concentrations are achieved) whenever treatment is initiated, reinitiated, or dosage is increased.
-
Prior to treatment, calculate Clcr and determine QTc interval. (See Contraindications under Cautions.) When titrating dosage, monitor QT interval 2–4 hours after each dose increase (if given orally) or after completion of each IV infusion.
-
Individualize dosage according to Clcr and QTc. Discontinue therapy, reduce dose, or increase dosing interval if QTc ≥500 msec.
-
Measure serum potassium and magnesium concentrations prior to initiating therapy and correct any imbalances.
-
Ensure adequate anticoagulation in patients with atrial fibrillation/flutter.
Conversion from Other Antiarrhythmic Agents
-
A transition period is recommended for patients converting from another antiarrhythmic agent to sotalol.
-
In general, delay initiation of sotalol for a period of at least 2–3 elimination half-lives of the previously administered antiarrhythmic drug; monitor patients carefully during transition. (See Specific Drugs under Interactions.)
Administration
Administer orally or by IV infusion (when oral administration not feasible).
Oral Administration
Administer orally as a tablet or oral solution (using the commercially available oral solution or an extemporaneously prepared solution).
Administer oral solution using appropriate measuring device (e.g., oral dosing syringe); use of a teaspoon or tablespoon may result in dosing errors and is not recommended.
Do not administer aluminum oxide and magnesium hydroxide-containing antacids within 2 hours of administration of sotalol. (See Specific Drugs under Interactions.)
Extemporaneous Oral Solution
To prepare extemporaneous oral solution, add 5 tablets (120 mg each) to a 180-mL polyethylene terephthalate (PET) prescription bottle containing 120 mL of simple syrup with 0.1% sodium benzoate (syrup NF); an oversized bottle is used to allow more effective shaking of the mixture.
May add tablets intact to syrup, add syrup to tablets, or crush tablets (making sure to add entire quantity of tablet powder to syrup).
Shake mixture to wet tablets, allow to hydrate for ≥2 hours, then shake intermittently over another 2 hours until dispersion of fine particles is obtained; may hydrate overnight to simplify disintegration process.
If tablets are crushed, shake until a dispersion of fine particles is obtained.
Resulting preparation contains 5 mg/mL of sotalol hydrochloride in solution with suspended inactive solid particles (water-insoluble tablet ingredients). (See Storage under Stability.)
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Administer by IV infusion over 5 hours. Use a volumetric pump to ensure that drug is delivered at a constant rate.
Must dilute commercially available injection concentrate with a suitable diluent (i.e., 0.9% sodium chloride injection, 5% dextrose injection, lactated Ringer’s injection) prior to administration. Manufacturer recommends that the volume of injection concentrate used to prepare the infusion solution and the final infusion solution volume exceed those required for the intended dose to account for dead space in infusion set. Preparation of a final volume of 120 or 300 mL is recommended; however, actual volume that should be infused is 100 or 250 mL, respectively. (See Table 1.)
|
Target IV Dose |
Amount of Injection Concentrate (mL) |
Amount of Diluent (mL) |
Total Volume Prepared (mL) |
Volume to Infuse (mL) |
|---|---|---|---|---|
|
75 mg |
6 |
114 |
120 |
100 |
|
6 |
294 |
300 |
250 |
|
|
112.5 mg |
9 |
111 |
120 |
100 |
|
9 |
291 |
300 |
250 |
|
|
150 mg |
12 |
108 |
120 |
100 |
|
12 |
288 |
300 |
250 |
Dosage
Available as sotalol hydrochloride; dosage expressed in terms of the salt. Adjust dosage carefully according to individual requirements and response, patient tolerance, renal function, and QT interval.
If a dose is missed, skip dose and take next dose at regularly scheduled time. Do not take a double dose or increase dosing frequency to compensate for missed dose.
Pediatric Patients
Life-threatening Ventricular Arrhythmias or Atrial Fibrillation/Flutter
Dosage in pediatric patients is based on pharmacokinetic data; safety and efficacy not evaluated in this population. Take the same precautions as in adults. Individualize dosage based on clinical response, heart rate, and QTc.
There are no studies of IV sotalol in pediatric patients.
Oral
Children ≥2 years of age with normal renal function: Initially, 30 mg/m2 3 times daily (total daily dose of 90 mg/m2). May titrate dosage to maximum of 60 mg/m2 3 times daily (equivalent to total daily dose of 360 mg in adults). Allow ≥36 hours to elapse between dosage escalations to achieve steady-state concentrations.
Children ≤2 years of age: Calculate dosage by multiplying the recommended initial dosage for children ≥2 years of age (i.e., 30 mg/m2 3 times daily) by an age-dependent factor obtained from manufacturer’s prescribing information. The age-dependent factor is approximately 0.3 in neonates 1 week old, 0.68 in infants 1 month of age, and 0.97 in infants 20 months of age. (See Table 2.) Use similar calculations for dosage increases.
To obtain dosages for ages not mentioned in this table, see age/factor graph in manufacturer’s prescribing information
See age/factor graph in manufacturer’s prescribing information for age-dependent factor
|
Age |
Initial Dosage Calculation (dosage for children ≥2 years of age [30 mg/m2 3 times daily] multiplied by an age-dependent factor) |
|---|---|
|
Neonates about 1 week of age |
30 mg/m2 × 0.3 = 9 mg/m2 administered 3 times daily |
|
Infants 1 month of age |
30 mg/m2 × 0.68 = 20 mg/m2 administered 3 times daily |
|
Infants 20 months of age |
30 mg/m2 × 0.97 = 29.1 mg/m2 administered 3 times daily |
Adults
Life-threatening Ventricular Arrhythmias
Oral
Initially, 80 mg twice daily in adults with normal renal function (Clcr >60 mL/minute). May increase dosage in increments of 80 mg per day every 3 days if QTc <500 msec.
Usual maintenance dosage: 160–320 mg daily in 2 or 3 divided doses; dosing >2 times a day usually not necessary.
Dosages as high as 480–640 mg daily have been used in patients with refractory life-threatening arrhythmias; however, risk of arrhythmic events increases with increasing dosage. (See Proarrhythmic Effects under Cautions.)
IV
Equivalent IV doses of sotalol hydrochloride are lower than oral doses; corresponding IV doses are as follows: 75 mg for an oral dose of 80 mg, 112.5 mg for an oral dose of 120 mg, and 150 mg for an oral dose of 160 mg.
Initially, 75 mg once or twice daily (depending on Clcr) by IV infusion over 5 hours. (See Renal Impairment under Dosage and Administration.) If desired response not achieved and drug is well tolerated without excessive QT interval prolongation, may increase dosage to 112.5 mg once or twice daily (depending on Clcr); manufacturer recommends that dosage be increased in increments of 75 mg daily every 3 days. Closely monitor ECG and QT interval during dose increases.
Based on experience with oral sotalol hydrochloride, the usual therapeutic effect should be observed with IV dosages of 75–150 mg once or twice daily; however, patients with life-threatening refractory ventricular arrhythmias have received higher dosages (e.g., oral dosages of 240–320 mg once or twice daily corresponding to IV dosages of 225–300 mg once or twice daily).
Atrial Fibrillation or Flutter
Oral
For maintenance of normal sinus rhythm in adults with atrial fibrillation or flutter who have normal renal function (Clcr >60 mL/minute): Initially, 80 mg twice daily. May increase dosage in increments of 80 mg per day every 3 days if QTc <500 msec.
In a dose-response study, the most effective dosage was 120 mg once or twice daily. Some clinicians state that dosage may be increased up to a maximum of 160 mg twice daily (provided drug is well tolerated and QTc <500 msec).
IV
Equivalent IV doses of sotalol hydrochloride are lower than oral doses; corresponding IV doses are as follows: 75 mg for an oral dose of 80 mg, 112.5 mg for an oral dose of 120 mg, and 150 mg for an oral dose of 160 mg.
For maintenance of normal sinus rhythm in adults with atrial fibrillation or flutter: Initially, 75 mg once or twice daily (depending on Clcr) by IV infusion over 5 hours. (See Renal Impairment under Dosage and Administration.)
If desired response not achieved and drug is well tolerated without excessive QT interval prolongation, may increase dosage after at least 3 days to 112.5 mg once or twice daily (depending on Clcr). Closely monitor ECG and QT interval during dose increases.
Based on experience with oral sotalol hydrochloride, the usual therapeutic effect should be observed with an IV dosage of 112.5 mg once or twice daily; however, manufacturer states that dosage may be increased up to 150 mg once or twice daily if necessary provided drug is well tolerated.
Prescribing Limits
Pediatric Patients
Life-threatening Ventricular Arrhythmias or Atrial Fibrillation/Flutter
Oral
Children ≥2 years of age: Maximum of 60 mg/m2 3 times daily.
Children ≤2 years of age: Reduce maximum dosage in children ≥2 years of age (i.e., 60 mg/m2 3 times daily) by an age-dependent factor obtained from manufacturer’s prescribing information. (See Dosage: Pediatric Patients, under Dosage and Administration.)
Adults
Atrial Fibrillation or Flutter
Oral
Some clinicians recommend maximum of 320 mg daily (160 mg twice daily); increased incidence of torsades de pointes with higher dosages. (See Proarrhythmic Effects under Cautions.)
Special Populations
Hepatic Impairment
Manufacturers make no specific dosage recommendations.
Renal Impairment
Reduce dose or dosing frequency to minimize risk of proarrhythmia; as in patients with normal renal function, closely monitor QT interval and heart rate. (See Proarrhythmic Effects under Cautions.)
Modify dosing interval according to Clcr. In general, administer the initial oral adult dose of 80 mg and subsequent doses twice daily in adults with Clcr>60 mL/minute and once daily in adults with Clcr 40–60 mL/minute. Generally contraindicated in patients with Clcr<40 mL/minute. In patients with ventricular arrhythmias, some manufacturers recommend a dosing interval of 36–48 hours in adults with Clcr 10–29 mL/minute and individualized dosing in those with Clcr<10 mL/minute.
Since elimination half-life is prolonged in patients with renal impairment, dosage increases generally should be made after administration of at least 5 doses at appropriate intervals.
Dosage in children with renal impairment not established. However, reduced doses and increased dosing intervals recommended for all age groups with renal impairment.
Sotalol is partially removed by dialysis; however, manufacturers make no dosing recommendations for patients undergoing dialysis.
Geriatric Patients
Modification of dosage based on age alone is not necessary.
Because geriatric patients may have decreased renal function and because patients with renal impairment may be at increased risk of sotalol-induced toxicity, monitor closely and adjust dosage accordingly. (See Renal Impairment under Dosage and Administration.)
Cautions for Sotalol
Contraindications
-
Bronchial asthma or related bronchospastic conditions.
-
Sinus bradycardia (<50 bpm while awake).
-
Sick sinus syndrome or second or third degree AV block unless a functioning pacemaker is present.
-
Congenital or acquired long QT interval syndromes.
-
Baseline QT interval >450 msec (some manufacturers state this is a contraindication only in patients being treated for atrial fibrillation or flutter).
-
Cardiogenic shock.
-
Decompensated heart failure.
-
Hypokalemia (serum potassium <4 mEq/L).
-
Clcr <40 mL/minute (some manufacturers state this is a contraindication only in patients being treated for atrial fibrillation or flutter).
-
Known hypersensitivity to sotalol or any ingredient in the formulation.
Warnings/Precautions
Warnings
Proarrhythmic Effects
Can cause serious ventricular arrhythmias, principally torsades de pointes, associated with prolonged QT interval; risk increases progressively with QT interval prolongation. (See Boxed Warning.)
Arrhythmogenic events occur not only when initiating therapy, but with every upward dosage adjustment.
QT interval prolongation is dose related.
Risk of torsades de pointes increases with decreased Clcr, female gender, larger doses, reduction of heart rate, hypokalemia, presence of sustained ventricular tachycardia, excessive QTc interval prolongation, history of cardiomegaly or heart failure. Decrease risk by adjusting dosage based on Clcr and monitoring ECG for excessive QT interval prolongation. Take appropriate precautions during administration. (See General under Dosage and Administration.)
Heart Failure
New onset or worsening heart failure may occur. Use contraindicated in patients with decompensated heart failure. (See Contraindications under Cautions.)
Monitor for signs and symptoms of heart failure and discontinue therapy if symptoms occur.
Electrolyte Disturbances
Electrolyte abnormalities (e.g., hypokalemia or hypomagnesemia) may exaggerate the degree of QT interval prolongation and increase the risk of torsades de pointes. Use not recommended until these imbalances are corrected.
Carefully monitor electrolyte and acid-base balance in patients with severe or prolonged diarrhea and in patients receiving diuretics concomitantly.
Bradycardia
Potential bradycardia in patients treated for supraventricular arrhythmias; associated with increased risk of torsades de pointes.
Abrupt Withdrawal of Therapy
Abrupt withdrawal may exacerbate angina symptoms and/or precipitate MI, particularly in patients with ischemic heart disease, or may precipitate thyroid storm in patients with thyroid disease.
Avoid abrupt discontinuance. If possible, gradually decrease dosage over a period of 1–2 weeks when discontinuing therapy, particularly in patients with ischemic heart disease; monitor patients.
If exacerbation of angina occurs or acute coronary insufficiency develops, initiate appropriate treatment (e.g., temporary use of another β-blocker).
Bronchospastic Disease
Use contraindicated in patients with bronchial asthma or related bronchospastic conditions. (See Contraindications under Cautions.)
Use not recommended in patients with nonallergic bronchospasm (e.g., chronic bronchitis, emphysema); use smallest effective dosage to minimize inhibition of bronchodilation produced by endogenous or exogenous catecholamine stimulation of β2-adrenergic receptors.
History of Anaphylactic Reactions
Possible increased reactivity to a variety of allergens; patients may be unresponsive to usual doses of epinephrine used to treat anaphylactic reactions.
Surgery
Some controversy exists regarding use of β-blockers during surgery. Hypotension, bradycardia, and stroke have occurred; in addition, it is unclear whether such use confers mortality benefits or risks.
Generally continue β-blockers during surgery in patients who are already receiving these drugs for a chronic condition. Consider risks versus benefits in individual patients.
Hypotension
Hypotension reported; monitor BP in patients with marginal cardiac compensation.
Diabetes Mellitus
Possible decreased signs and symptoms of acute hypoglycemia (e.g., tachycardia). May increase blood glucose concentrations and insulin requirements in diabetic patients.
Sick Sinus Syndrome
Possible increased risk of torsades de pointes in patients with atrial fibrillation and sinus node dysfunction, especially after cardioversion. Use contraindicated in patients with sick sinus syndrome unless a functioning pacemaker is present due to risk of sinus bradycardia, sinus pause, or sinus arrest. (See Contraindications under Cautions.)
Thyroid Abnormalities
Signs of hyperthyroidism (e.g., tachycardia) may be masked.
Possible thyroid storm if therapy is abruptly withdrawn. (See Abrupt Withdrawal of Therapy under Cautions.)
General Precautions
Other Precautions
Shares the toxic potentials of other nonselective β-adrenergic blocking agents; observe usual precautions of these agents.
Specific Populations
Pregnancy
Category B.
Lactation
Distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Class III electrophysiologic and β-blocking effects, pharmacokinetics and the relationship between plasma concentrations and effects (e.g., QTc intervals, resting heart rate) have been evaluated in children 3 days to 12 years of age.
Has been effective in a limited number of infants <3 months of age and children <18 years of age for supraventricular arrhythmias; less effective for ventricular arrhythmias. Mild sinus bradycardia occurred in most infants; fatigue occurred in several children and required discontinuance in a few.
Similar to adults, serious adverse events including death, torsades de pointes, other proarrhythmias, AV block, and bradycardia have been reported in infants and children; usual precautions in adults should also be observed in pediatric patients.
Geriatric Use
Insufficient experience in geriatric patients to determine whether safety and efficacy in geriatric patients differ from safety and efficacy in younger adults; however clinical trials of sotalol included many patients >50 years of age.
Overall risk of cardiac death was associated with increasing age in clinical trials.
Monitor closely and adjust dosage accordingly due to greater frequency of decreased renal function and increased risk of toxicity observed in the elderly.
Hepatic Impairment
Clearance of sotalol not altered by hepatic impairment.
Renal Impairment
Clearance is decreased depending on degree of renal impairment. (See Special Populations under Pharmacokinetics.)
Dosage adjustments necessary based on degree of renal impairment. (See Renal Impairment under Dosage and Administration.)
Partially removed by dialysis; monitor closely for efficacy of arrhythmia control and adverse effects (changes in heart rate and/or QT interval).
Common Adverse Effects
Common adverse effects based on use of oral sotalol: Sinus bradycardia (heart rate <50 bpm), arrhythmogenic effects, chest pain, palpitation, hypotension, fatigue, dizziness, asthenia, hyperhidrosis, lightheadedness, upper respiratory tract problems, visual problems, sleep problems, weakness, dyspnea, headache, cough, nausea, vomiting, diarrhea, abdominal pain, edema, extremity pain.
Drug Interactions
Drugs metabolized by CYP isoenzymes do not alter the pharmacokinetics of sotalol; sotalol does not induce or inhibit any CYP isoenzymes.
Specific Drugs
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum- or magnesium-containing) |
Decreased absorption of sotalol and reduced bradycardic effect |
Do not administer within 2 hours of sotalol; no effects on sotalol pharmacokinetics or pharmacodynamics observed when administered 2 hours after sotalol |
|
Antiarrhythmics, class Ia (e.g., disopyramide, quinidine, procainamide) |
May prolong refractoriness and increase risk of QT interval prolongation |
Concomitant use not recommended; withhold for at least 3 half-lives before initiating sotalol |
|
Antiarrhythmics, class Ib or Ic |
Limited experience with concomitant use |
Withhold for at least 3 half-lives before initiating sotalol |
|
Antiarrhythmics, class II (β-blockers) |
Possible additive class II (β-adrenergic receptor blocking) effects |
|
|
Antiarrhythmics, class III (e.g., amiodarone) |
May prolong refractoriness and increase risk of QT interval prolongation |
Concomitant use not recommended; withhold for at least 3 half-lives before initiating sotalol |
|
Antidepressants, tricyclics |
Prolongs QT interval |
Concomitant use not recommended |
|
Antidiabetic agents (oral) |
May cause hyperglycemia |
May require antidiabetic agent dosage adjustment |
|
Calcium-channel blocking agents |
Possible additive effects on AV conduction or ventricular function; also potential for additive bradycardia and hypotensive effects |
Use concomitantly with caution |
|
Clonidine |
Increased risk of bradycardia; in addition, β-blockers may potentiate rebound hypertension that occasionally occurs after discontinuance of clonidine |
To reduce risk of rebound hypertension, withdraw sotalol several days before the gradual withdrawal of clonidine |
|
Digoxin |
Possible increased proarrhythmic events Concomitant use increases risk of bradycardia |
Unclear if proarrhythmias are the result of interaction or presence of heart failure (known proarrhythmia risk factor) |
|
Hydrochlorothiazide |
No pharmacokinetic interaction observed |
|
|
Insulin |
May cause hyperglycemia; may mask hypoglycemic symptoms |
Adjust insulin dosage, if necessary |
|
Macrolides (e.g., azithromycin, clarithromycin) |
Possible prolonged QT interval |
Concomitant use not recommended |
|
Phenothiazines |
May prolong QT interval |
Concomitant use not recommended |
|
Quinolone antibiotics (e.g., ciprofloxacin, levofloxacin) |
May prolong QT interval |
Concomitant use not recommended |
|
β2-Receptor agonists (e.g., albuterol, terbutaline, isoproterenol) |
Increased dosages of β2-receptor agonists may be required |
|
|
Reserpine |
Concomitant use may cause excessive decrease in resting sympathetic tone |
Monitor closely for evidence of hypotension or marked bradycardia that may produce syncope |
|
Warfarin |
No pharmacokinetic interaction observed |
Sotalol Pharmacokinetics
Absorption
Bioavailability
90–100%.
Peak plasma concentrations are reached in 2.5–4 hours following oral administration.
Steady-state plasma concentrations are reached in 2–3 days following twice-daily oral administration.
Food
Food reduces oral bioavailability by about 20%.
Distribution
Extent
Crosses the placenta; found in amniotic fluid.
Does not readily cross blood-brain barrier.
Plasma Protein Binding
Does not bind to plasma proteins.
Elimination
Metabolism
Not metabolized.
Elimination Route
Eliminated principally by glomerular filtration and tubular secretion; excreted principally unchanged in urine.
Half-life
12 hours.
Special Populations
Renal impairment may reduce clearance. Elimination half-life in anuric patients may be prolonged (up to 69 hours). (See Renal Impairment under Dosage and Administration.)
In pediatric patients, half-life decreases with decreasing age <2 years of age.
Stability
Storage
Oral
Solution
Commercially available oral solution: 20–25°C (may be exposed to 15–30°C).
Extemporaneous oral solution: 15–30°C at ambient humidity; stable for ≤3 months after preparation.
Tablets
Tight, light-resistant container at 20–25°C (may be exposed to 15–30°C).
Parenteral
Injection
20–25°C. Protect from freezing and light.
Compatibility
Parenteral
Solution Compatibility402
|
Compatible |
|---|
|
Dextrose 5% |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.9% |
Actions
-
Inhibits response to adrenergic stimuli by competitively blocking β1-adrenergic receptors within the myocardium and β2-adrenergic receptors within bronchial and vascular smooth muscle.
-
Exhibits antiarrhythmic activity characteristic of class II antiarrhythmic agents.
-
Does not exhibit membrane-stabilizing activity, but exhibits electrophysiologic effects characteristic of class III antiarrhythmic agents (e.g., prolongs repolarization and refractoriness without affecting conduction).
-
Does not exhibit intrinsic sympathomimetic activity.
-
Selectively inhibits the rapidly activating component of the potassium channel involved in repolarization of cardiac cells (i.e., the rapidly activated inward component of the delayed rectifier potassium current IKr) in vitro.
-
Does not appear to block sodium channels at usual doses (although it may at relatively high doses).
-
Racemic mixture of 2 optical isomers that both exhibit class III antiarrhythmic activity, but only the l-isomer exhibits β-blocking activity.
Advice to Patients
-
If a dose is missed, importance of taking next scheduled dose at the usual time and not doubling the dose to make up for missed dose.
-
Importance of patients immediately contacting their clinician if syncope, pre-syncopal symptoms, or cardiac palpitations occur.
-
Importance of advising patients that their electrolytes and ECG will be monitored during treatment.
-
Importance of informing patients (especially those with ischemic heart disease) not to interrupt or discontinue therapy without consulting clinician and to fill their prescriptions on time to avoid treatment interruption.
-
Importance of informing patients not to take sotalol tablets or oral solution 2 hours before or after administration of an antacid containing aluminum oxide or magnesium hydroxide (e.g., Maalox, Mylanta).
-
Importance of immediately reporting to their clinician any conditions, concomitant therapy (e.g., diuretics), and/or manifestations associated with altered electrolyte balance (e.g., severe or prolonged diarrhea, unusual sweating, vomiting, loss of appetite, excessive thirst).
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
25 mg/5 mL |
Sotylize |
Arbor |
|
Tablets |
80 mg* |
Betapace (scored) |
Covis |
|
|
Betapace AF (scored) |
Covis |
|||
|
Sorine (scored) |
Upsher-Smith |
|||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
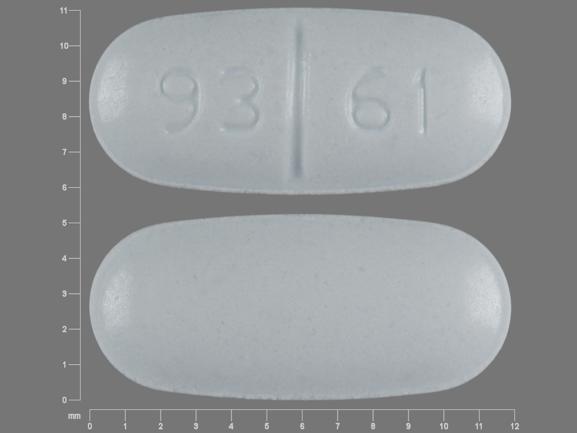
120 mg* |
Betapace (scored) |
Covis |
||
|
Betapace AF (scored) |
Covis |
|||
|
Sorine (scored) |
Upsher-Smith |
|||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
160 mg* |
Betapace (scored) |
Covis |
||
|
Betapace AF (scored) |
Covis |
|||
|
Sorine (scored) |
Upsher-Smith |
|||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
240 mg* |
Sorine (scored) |
Upsher-Smith |
||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
Parenteral |
Injection concentrate, for IV infusion |
15 mg/mL* |
Sotalol Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about sotalol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (59)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
- En español