Sotalol (Oral)
Generic name: sotalol [ SOE-ta-lol ]
Brand names: Betapace, Betapace AF, Sorine, Sotylize
Drug classes: Group III antiarrhythmics, Non-cardioselective beta blockers
Medically reviewed by Drugs.com. Last updated on May 28, 2025.
To minimize the risk of induced arrhythmia, patients initiated or reinitiated on oral sotalol or converted from IV sotalol to oral administration should be placed in a facility that can provide cardiac resuscitation, continuous electrocardiographic monitoring and calculations of creatinine clearance. Sotalol can cause life threatening ventricular tachycardia associated with QT interval prolongation. Do not initiate sotalol therapy if the baseline QTc is longer than 450 ms. If the QT interval prolongs to 500 ms or greater, the dose must be reduced, the interval between doses prolonged, or the drug discontinued. Adjust the dosing interval based on creatinine clearance .
Oral route(Tablet)To minimize the risk of drug-induced arrhythmia, initiate or reinitiate oral sotalol in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring. Sotalol can cause life threatening ventricular tachycardia associated with QT interval prolongation. If the QT interval prolongs to 500 msec or greater, reduce the dose, lengthen the dosing interval, or discontinue the drug. Calculate creatinine clearance to determine appropriate dosing .
Uses for sotalol
Sotalol is used to a treat life-threatening heart rhythm problem called ventricular arrhythmia. It is also used to treat heart rhythm problems called atrial fibrillation or atrial flutter.
Sotalol is a beta-blocker. It works by affecting the response to nerve impulses in certain parts of the body, like the heart. As a result, the heart beats slower and at a regular rhythm.
This medicine is available only with your doctor's prescription.
Before using sotalol
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of sotalol in the pediatric population. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of sotalol oral solution or Betapace® and Betapace® AF tablets in the elderly. However, elderly patients are more likely to have age-related kidney problems, which may require caution and an adjustment in the dose for patients receiving this medicine.
No information is available on the relationship of age to the effects of sotalol tablets in geriatric patients.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Bepridil
- Cisapride
- Dronedarone
- Fingolimod
- Grepafloxacin
- Levoketoconazole
- Levomethadyl
- Mesoridazine
- Pimozide
- Piperaquine
- Saquinavir
- Sparfloxacin
- Terfenadine
- Thioridazine
- Vernakalant
- Ziprasidone
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acecainide
- Acetazolamide
- Adagrasib
- Albuterol
- Alfuzosin
- Amiloride
- Amiodarone
- Amisulpride
- Amitriptyline
- Amoxapine
- Anagrelide
- Apomorphine
- Arformoterol
- Aripiprazole
- Aripiprazole Lauroxil
- Arsenic Trioxide
- Artemether
- Asenapine
- Astemizole
- Atazanavir
- Azithromycin
- Azosemide
- Bambuterol
- Bedaquiline
- Bemetizide
- Bendroflumethiazide
- Benzthiazide
- Bitolterol
- Broxaterol
- Bumetanide
- Buprenorphine
- Buserelin
- Canrenoate
- Ceritinib
- Chloral Hydrate
- Chloroquine
- Chlorpromazine
- Chlorthalidone
- Ciprofloxacin
- Citalopram
- Clarithromycin
- Clenbuterol
- Clofazimine
- Clomipramine
- Clonidine
- Clopamide
- Clothiapine
- Clozapine
- Colterol
- Crizotinib
- Cyclobenzaprine
- Cyclothiazide
- Dabrafenib
- Darunavir
- Dasatinib
- Degarelix
- Delamanid
- Desipramine
- Deslorelin
- Deutetrabenazine
- Dexmedetomidine
- Dibenzepin
- Digoxin
- Diltiazem
- Disopyramide
- Dofetilide
- Dolasetron
- Domperidone
- Donepezil
- Doxepin
- Droperidol
- Ebastine
- Efavirenz
- Eliglustat
- Encainide
- Encorafenib
- Enflurane
- Entrectinib
- Epinephrine
- Eribulin
- Erythromycin
- Escitalopram
- Ethacrynic Acid
- Etozolin
- Etrasimod
- Famotidine
- Felbamate
- Fenoldopam
- Fenoterol
- Fenquizone
- Fexinidazole
- Flecainide
- Fluconazole
- Fluoxetine
- Formoterol
- Foscarnet
- Fosphenytoin
- Fostemsavir
- Furosemide
- Galantamine
- Gatifloxacin
- Gemifloxacin
- Gepirone
- Glasdegib
- Gonadorelin
- Goserelin
- Granisetron
- Halofantrine
- Haloperidol
- Halothane
- Hexoprenaline
- Histrelin
- Hydrochlorothiazide
- Hydroflumethiazide
- Hydroquinidine
- Hydroxychloroquine
- Hydroxyzine
- Ibutilide
- Iloperidone
- Imipramine
- Indacaterol
- Indapamide
- Indecainide
- Inotuzumab Ozogamicin
- Iobenguane I 131
- Iohexol
- Isoetharine
- Isoflurane
- Isradipine
- Itraconazole
- Ivabradine
- Ivosidenib
- Ketoconazole
- Lacosamide
- Lapatinib
- Lefamulin
- Lenvatinib
- Leuprolide
- Levalbuterol
- Levofloxacin
- Lidocaine
- Lidoflazine
- Lofexidine
- Lopinavir
- Lumefantrine
- Macimorelin
- Mannitol
- Mefloquine
- Metaproterenol
- Methadone
- Methotrimeprazine
- Metolazone
- Metronidazole
- Mexiletine
- Mifepristone
- Mirtazapine
- Mizolastine
- Moricizine
- Moxifloxacin
- Nafarelin
- Nelfinavir
- Nilotinib
- Norfloxacin
- Nortriptyline
- Octreotide
- Ofloxacin
- Olanzapine
- Olodaterol
- Ondansetron
- Osilodrostat
- Osimertinib
- Oxaliplatin
- Oxymetazoline
- Ozanimod
- Pacritinib
- Paliperidone
- Panobinostat
- Papaverine
- Paroxetine
- Pasireotide
- Pazopanib
- Pentamidine
- Perphenazine
- Phenobarbital
- Pimavanserin
- Pipamperone
- Pirbuterol
- Piretanide
- Pitolisant
- Polythiazide
- Ponesimod
- Posaconazole
- Prilocaine
- Primidone
- Probucol
- Procainamide
- Procaterol
- Prochlorperazine
- Promethazine
- Propafenone
- Protriptyline
- Quetiapine
- Quinethazone
- Quinidine
- Quinine
- Quizartinib
- Ranolazine
- Relugolix
- Reproterol
- Ribociclib
- Rimiterol
- Risperidone
- Ritodrine
- Ritonavir
- Rivastigmine
- Salmeterol
- Selpercatinib
- Sertindole
- Sertraline
- Sevoflurane
- Siponimod
- Sodium Phosphate
- Sodium Phosphate, Dibasic
- Sodium Phosphate, Monobasic
- Solifenacin
- Sorafenib
- Spiramycin
- Spironolactone
- Sulfamethoxazole
- Sulpiride
- Sultopride
- Sunitinib
- Tacrolimus
- Tamoxifen
- Telaprevir
- Telavancin
- Telithromycin
- Terbutaline
- Tetrabenazine
- Ticrynafen
- Tocainide
- Tolterodine
- Toremifene
- Torsemide
- Trazodone
- Tretoquinol
- Triamterene
- Trichlormethiazide
- Triclabendazole
- Trifluoperazine
- Trimethoprim
- Trimipramine
- Triptorelin
- Tulobuterol
- Vandetanib
- Vardenafil
- Vemurafenib
- Venlafaxine
- Verapamil
- Vilanterol
- Vinflunine
- Voclosporin
- Voriconazole
- Vorinostat
- Xipamide
- Zolmitriptan
- Zotepine
- Zuclopenthixol
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abarelix
- Acarbose
- Aceclofenac
- Acemetacin
- Albiglutide
- Alogliptin
- Aluminum Carbonate, Basic
- Aluminum Hydroxide
- Aluminum Phosphate
- Amtolmetin Guacil
- Aspirin
- Bromfenac
- Bufexamac
- Bunazosin
- Canagliflozin
- Celecoxib
- Chlorpropamide
- Choline Salicylate
- Clonixin
- Dapagliflozin
- Dexibuprofen
- Dexketoprofen
- Diclofenac
- Diflunisal
- Dihydroxyaluminum Aminoacetate
- Dihydroxyaluminum Sodium Carbonate
- Dipyrone
- Doxazosin
- Droxicam
- Dulaglutide
- Empagliflozin
- Ertugliflozin
- Etodolac
- Etofenamate
- Etoricoxib
- Exenatide
- Felbinac
- Fenoprofen
- Fepradinol
- Feprazone
- Floctafenine
- Flufenamic Acid
- Flurbiprofen
- Glimepiride
- Glipizide
- Glyburide
- Ibuprofen
- Indomethacin
- Insulin Aspart, Recombinant
- Insulin Degludec
- Insulin Detemir
- Insulin Glargine, Recombinant
- Insulin Glulisine
- Insulin Human Inhaled
- Insulin Human Isophane (NPH)
- Insulin Human Regular
- Insulin Lispro, Recombinant
- Ketoprofen
- Ketorolac
- Linagliptin
- Liraglutide
- Lixisenatide
- Lornoxicam
- Loxoprofen
- Lumiracoxib
- Magaldrate
- Magnesium Carbonate
- Magnesium Hydroxide
- Magnesium Oxide
- Magnesium Peroxide
- Magnesium Trisilicate
- Meclofenamate
- Mefenamic Acid
- Meloxicam
- Metformin
- Methyldopa
- Miglitol
- Morniflumate
- Moxisylyte
- Nabumetone
- Naproxen
- Nateglinide
- Nepafenac
- Niflumic Acid
- Nimesulide
- Nimesulide Beta Cyclodextrin
- Oxaprozin
- Oxyphenbutazone
- Parecoxib
- Phenoxybenzamine
- Phentolamine
- Phenylbutazone
- Piketoprofen
- Pioglitazone
- Piroxicam
- Pramlintide
- Pranoprofen
- Prazosin
- Proglumetacin
- Propyphenazone
- Proquazone
- Repaglinide
- Rofecoxib
- Rosiglitazone
- Salicylic Acid
- Salsalate
- Saxagliptin
- Sitagliptin
- Sodium Salicylate
- St John's Wort
- Sulindac
- Tamsulosin
- Tenoxicam
- Terazosin
- Tiaprofenic Acid
- Tolazamide
- Tolbutamide
- Tolfenamic Acid
- Tolmetin
- Trimazosin
- Urapidil
- Valdecoxib
- Vildagliptin
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Angina or
- Bronchospasm or
- Heart attack, recent or
- Heart disease (eg, coronary insufficiency, heart failure, ischemic heart disease) or
- Heart rhythm problem (eg, QT prolongation) or
- Hypomagnesemia (low magnesium levels in the blood) or
- Hypotension (low blood pressure)—Use with caution. May make these conditions worse.
- Asthma or
- Bradycardia (slow heartbeat), without a pacemaker or
- Cardiogenic shock (shock caused by heart attack) or
- Heart block, without a pacemaker or
- Heart failure, uncontrolled or
- Heart rhythm problem (eg, long QT syndrome) or
- Hypokalemia (low potassium levels in the blood) or
- Kidney disease, severe or
- Sick sinus syndrome (type of abnormal heart rhythm), without a pacemaker or—Should not be used in patients with these conditions.
- Diabetes or
- Hyperthyroidism (overactive thyroid) or
- Hypoglycemia (low blood sugar)—May cover up some of the signs and symptoms of these diseases, such as a fast heartbeat.
- Kidney disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Lung disease (eg, bronchitis, emphysema)—May cause difficulty with breathing in patients with this condition.
Proper use of sotalol
Take this medicine only as directed by your doctor. Do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered. When your supply of this medicine is running low, contact your doctor or pharmacist ahead of time. Do not allow yourself to run out of this medicine.
This medicine should come with a patient information leaflet. Read and follow these instructions carefully. Ask your doctor if you have any questions.
For the first three days, you will receive this medicine in a hospital where your heart rhythm can be monitored.
Your pharmacist may prepare the tablets to make an oral liquid. Talk with your doctor or pharmacist if you have any concerns about this.
Measure the oral liquid with a marked measuring spoon, oral syringe, or medicine cup. The average household teaspoon may not hold the right amount of liquid.
If you are also taking an antacid aluminum or magnesium hydroxide, take it 2 hours before or 2 hours after taking sotalol.
Use only the brand of this medicine that your doctor prescribed. Different brands may not work the same way.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For abnormal heart rhythms:
- For oral dosage forms (solution or tablets):
- Adults—At first, 80 milligrams (mg) once or 2 times a day. Your doctor may adjust your dose every 3 days as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage forms (Betapace® and Betapace® AF tablets):
- Adults—At first, 80 milligrams (mg) 2 times a day. Your doctor may adjust your dose every 3 days as needed.
- Children 2 years of age and older—Dose is based on body weight and must be determined by your doctor. At first, the dose is usually 1.2 mg per kilogram (kg) of body weight 3 times a day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 2.4 mg per kg of body weight 3 times a day.
- Children younger than 2 years of age—Use and dose must be determined by your doctor.
- For oral dosage forms (solution or tablets):
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Precautions while using sotalol
It is very important that your doctor check your progress at regular visits to make sure this medicine is working properly. Blood, urine, and ECG tests will be needed to check for unwanted effects.
Contact your doctor right away if you have any changes to your heart rhythm. You might feel dizzy or faint, or you might have a fast, pounding, or uneven heartbeat. Make sure your doctor knows if you or anyone in your family has ever had a heart rhythm problem such as QT prolongation.
This medicine may make you dizzy. Do not drive or do anything else that could be dangerous until you know how this medicine affects you. Stand up slowly if you feel dizzy or lightheaded.
Do not interrupt or stop taking this medicine without first checking with your doctor. Your doctor may want you to gradually reduce the amount you are taking before stopping it completely. Some conditions may become worse when the medicine is stopped suddenly, which can be dangerous.
Sotalol may cause heart failure in some patients. Check with your doctor right away if you are having chest pain or discomfort, dilated neck veins, extreme fatigue, irregular breathing, an irregular heartbeat, swelling of the face, fingers, feet, or lower legs, or weight gain.
This medicine may cause changes in your blood sugar levels. Also, this medicine may cover up signs of low blood sugar in patients who have diabetes or are fasting (eg, surgery, not eating regularly, vomiting), such as a rapid pulse rate. Check with your doctor if you have these problems or if you notice a change in the results of your blood or urine sugar tests.
Before having any kind of surgery (including dental surgery) or emergency treatment, tell the medical doctor or dentist in charge that you are using this medicine. You may need to stop using this medicine several days before having surgery or medical tests.
This medicine may cause serious allergic reaction, including anaphylaxis, which can be life-threatening and requires immediate medical attention. Call your doctor right away if you have a rash, itching, hoarseness, trouble breathing, trouble swallowing, or any swelling of your hands, face, or mouth while you are using this medicine.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Side Effects of sotalol
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Blurred vision
- chest pain, tightness, or discomfort
- confusion
- difficult or labored breathing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fast, slow, irregular, pounding, or racing heartbeat or pulse
- lightheadedness, dizziness, or fainting
- nausea and vomiting
- sweating
- swelling of the face, fingers, feet, or lower legs
- unusual tiredness or weakness
Less common
- Body aches or pain
- burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feelings
- cough or hoarseness
- decreased alertness
- difficulty with speaking
- dilated neck veins
- double vision
- feeling of warmth or heat
- fever or chills
- flushing or redness of the skin, especially on the face and neck
- headache
- inability to move the arms, legs, or facial muscles
- inability to speak
- irregular breathing
- joint pain or swelling
- loss of voice
- lower back or side pain
- nervousness
- noisy breathing
- painful, burning, or difficult urination
- pounding in the ears
- slow speech
- stomach pain or swelling
- weight gain
Rare
- Fast breathing
- pinpoint red spots on the skin
Incidence not known
- Black, tarry stools
- bleeding gums
- blood in the urine or stools
- blue lips and fingernails
- coughing that sometimes produces a pink frothy sputum
- crying
- delusions of persecution, mistrust, suspiciousness, or combativeness
- false or unusual sense of well-being
- feeling of unreality
- mental depression
- not able to move
- pale skin
- pinpoint red spots on the skin
- quick to react or overreact emotionally
- rapidly changing moods
- sense of detachment from self or body
- sore throat
- sores, ulcers, or white spots on the lips or in the mouth
- swelling in the legs and ankles
- swollen glands
- unusual bleeding or bruising
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of overdose
- Anxiety
- blurred vision
- chest pain or discomfort
- cold sweats
- confusion
- cool, pale skin
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- depression
- fast, pounding, or irregular heartbeat or pulse
- increased hunger
- nightmares
- seizures
- shakiness
- slow or irregular heartbeat
- slurred speech
- sweating
- unusual tiredness or weakness
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Acid or sour stomach
- difficulty with sleeping
- heartburn or indigestion
- pain in the arms or legs
Less common
- Changes in vision
- decreased sexual performance or desire
- loss of appetite
- mood changes
- night blindness
- passing gas
- skin rash
- weight changes
Rare
- Feeling of constant movement of self or surroundings
- hair loss or thinning of the hair
- itching skin
- muscle aches, cramps, pains, or stiffness
- quick to react or overreact emotionally
- sensation of spinning
- severe sunburn
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Commonly used brand name(s)
In the U.S.
- Betapace
- Betapace AF
- Sorine
- Sotylize
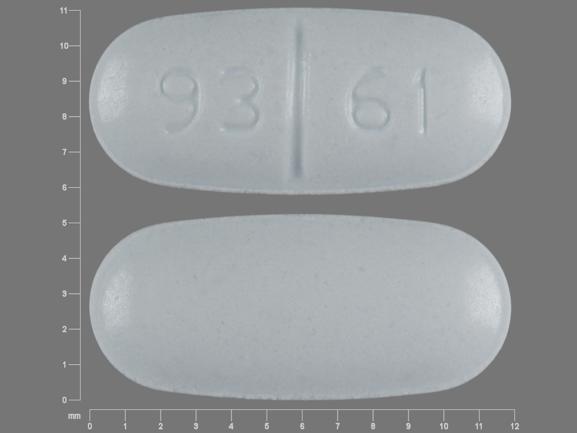
Available Dosage Forms:
- Tablet
- Solution
Therapeutic Class: Cardiovascular Agent
Pharmacologic Class: Beta-Adrenergic Blocker, Nonselective
Frequently asked questions
More about sotalol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (59)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.