Solriamfetol (Monograph)
Brand name: Sunosi
Drug class: Wakefulness-promoting Agents
- Dopamine- and Norepinephrine-reuptake Inhibitors
Chemical name: [(2R)-2-amino-3-phenylpropyl] carbamate, monohydrochloride
Molecular formula: C10H14N2O2•HCl
CAS number: 178429-65-7
Introduction
Dopamine- and norepinephrine-reuptake inhibitor (DNRI); a wakefulness-promoting agent.1 2 3 4
Uses for Solriamfetol
Obstructive Sleep Apnea
Symptomatic treatment of obstructive sleep apnea to improve wakefulness in patients with excessive daytime sleepiness.1 3 9 10 11 Use as an adjunct to standard treatment(s) for the underlying obstruction (e.g., nasal continuous positive airway pressure [CPAP]).1 Not indicated to treat the underlying airway obstruction, and not a substitute for standard treatments for airway obstruction.1 Provide standard treatments for ≥1 month prior to initiating solriamfetol and continue such treatments during solriamfetol therapy.1
Narcolepsy
Symptomatic treatment of narcolepsy to improve wakefulness in patients with excessive daytime sleepiness1 2 9 10 (designated an orphan drug by FDA for treatment of narcolepsy).13
Solriamfetol Dosage and Administration
General
-
Ensure BP is adequately controlled before initiating solriamfetol.1 (See Cardiovascular Effects under Cautions.)
Administration
Oral Administration
Administer orally once daily upon awakening.1 Avoid administration within 9 hours of planned bedtime because of the potential for sleep interference.1
Administer without regard to food.1 6
Dosage
Available as solriamfetol hydrochloride; dosage expressed in terms of solriamfetol.1
Adults
Obstructive Sleep Apnea
Oral
Initially, 37.5 mg once daily.1 Based on efficacy and tolerability, may double dosage at intervals of at least 3 days up to a maximum of 150 mg once daily.1 Recommended dosage range is 37.5–150 mg once daily.1 (See Prescribing Limits under Dosage and Administration.)
Narcolepsy
Oral
Initially, 75 mg once daily.1 Based on efficacy and tolerability, may double dosage at intervals of at least 3 days up to a maximum of 150 mg once daily.1 Recommended dosage range is 75–150 mg once daily.1 (See Prescribing Limits under Dosage and Administration.)
Prescribing Limits
Adults
Obstructive Sleep Apnea
Oral
Maximum 150 mg once daily.1 Dosages >150 mg daily do not provide sufficient additional clinical benefit to outweigh dose-related adverse effects.1 (See Cardiovascular Effects and also see Common Adverse Effects under Cautions.)
Narcolepsy
Oral
Maximum 150 mg once daily.1 Dosages >150 mg daily do not provide sufficient additional clinical benefit to outweigh dose-related adverse effects.1 (See Cardiovascular Effects and also see Common Adverse Effects under Cautions.)
Special Populations
Hepatic Impairment
Manufacturer makes no specific dosage recommendations for patients with hepatic impairment.1 (See Hepatic Impairment under Cautions.)
Renal Impairment
Mild renal impairment (eGFR 60–89 mL/minute per 1.73 m2): Dosage adjustment not required.1
Moderate renal impairment (eGFR 30–59 mL/minute per 1.73 m2): Initially, 37.5 mg once daily; based on efficacy and tolerability, may increase dosage after at least 7 days to a maximum of 75 mg once daily.1
Severe renal impairment (eGFR 15–29 mL/minute per 1.73 m2): 37.5 mg once daily; maximum recommended dosage is 37.5 mg daily.1
End-stage renal disease (eGFR <15 mL/minute per 1.73 m2): Use not recommended.1 (See Pharmacokinetics and also see Renal Impairment under Cautions.)
Geriatric Patients
Dosage adjustments based on eGFR may be required.1 Consider lower dosages and close monitoring.1 (See Geriatric Use under Cautions.)
Related/similar drugs
Provigil, Nuvigil, Wakix, Xyrem, Xywav, Adderall, methylphenidate
Cautions for Solriamfetol
Contraindications
-
Current or recent (within 14 days) therapy with a monoamine oxidase (MAO) inhibitor.1 (See Cardiovascular Effects under Cautions and also see Specific Drugs under Interactions.)
Warnings/Precautions
Cardiovascular Effects
Produces dose-dependent increases in systolic and diastolic BP and heart rate.1
Chronically elevated BP increases the risk of major adverse cardiovascular events (e.g., stroke, MI, cardiovascular death).1 The magnitude of the increase in absolute risk is dependent on the increase in BP and underlying cardiovascular risk.1 Many patients with obstructive sleep apnea or narcolepsy have multiple cardiovascular risk factors (e.g., hypertension, diabetes mellitus, hyperlipidemia, high body mass index [BMI]).1
Assess BP and control hypertension prior to initiating solriamfetol.1 Regularly monitor BP during therapy and appropriately manage new or exacerbated hypertension.1
Caution advised in patients at higher risk of major adverse cardiovascular events, particularly older patients and those with known cardiovascular and cerebrovascular disease or preexisting hypertension.1 Caution also advised in patients receiving concomitant therapy with drugs known to increase BP and heart rate.1
Patients with moderate or severe renal impairment may be at increased risk for elevations in BP and heart rate because the drug's half-life is prolonged in such patients.1
Periodically reassess the need for continued solriamfetol therapy.1 If increases in BP or heart rate occur and cannot be managed by solriamfetol dosage reduction or other appropriate medical intervention, consider drug discontinuance.1
Psychiatric Effects
Adverse psychiatric effects (e.g., anxiety, insomnia, irritability) reported.1
Not evaluated in patients with psychosis or bipolar disorders; caution advised in patients with a history of such disorders.1
Patients with moderate or severe renal impairment may be at higher risk for psychiatric symptoms because the drug's half-life is prolonged in such patients.1
Monitor patients for the possible emergence or exacerbation of psychiatric symptoms.1 If psychiatric symptoms develop, consider dosage reduction or drug discontinuance.1
Abuse, Misuse, and Dependence Potential
Classified as Schedule IV (C-IV) drug.1 Abuse potential of solriamfetol (200, 600, and 1200 mg) similar to or lower than that of the Schedule IV drug phentermine hydrochloride (45 and 90 mg) in individuals with a history of recreational stimulant use.1 8
Efficacy and safety studies in patients with obstructive sleep apnea or narcolepsy provided no evidence that abrupt discontinuance produced a consistent pattern of adverse events suggestive of physical dependence or withdrawal in individual patients.1
Carefully evaluate patients for a history of recent drug abuse, particularly alcohol or stimulant (e.g., amphetamine, cocaine, methylphenidate) abuse; closely monitor patients with such history for possible signs of misuse or abuse (e.g., incrementation of doses, drug-seeking behavior).1
Specific Populations
Pregnancy
Available data from case reports are not sufficient to determine solriamfetol-associated risks of major birth defects, spontaneous abortion, or adverse maternal or fetal outcomes.1 Teratogenicity, fetal toxicity, and developmental toxicity observed in animal studies.1
Pregnancy registry available ([Web] or 877-283-6220).1
Lactation
Not known whether solriamfetol or its metabolites are distributed into human milk; solriamfetol distributes into milk in rats.1 Also not known whether the drug affects breast-fed infants or affects milk production.1
Consider the developmental and health benefits of breast-feeding along with the mother’s clinical need for solriamfetol and any potential adverse effects on the breast-fed child from the drug or from the underlying maternal condition.1 Monitor nursing infants for adverse effects (e.g., agitation, insomnia, anorexia, reduced weight gain) potentially resulting from exposure to the drug through breast milk.1
Pediatric Use
Safety and efficacy in pediatric patients not established.1
Geriatric Use
No clinically important differences in safety or efficacy observed between geriatric patients and younger adults.1
Age does not appear to substantially affect pharmacokinetics of solriamfetol; no dosage adjustments made in clinical trials that included patients ≥65 of age.1 However, dosage adjustment may be necessary because geriatric patients are more likely to have decreased renal function and solriamfetol is eliminated mainly by the kidneys; consider use of lower dosages and close monitoring.1
Hepatic Impairment
Hepatic impairment is not expected to affect the pharmacokinetics of solriamfetol; the drug undergoes minimal metabolism.5
Renal Impairment
Solriamfetol clearance decreases with worsening renal function.1 7 (See Pharmacokinetics.) Adjust dosage in patients with moderate to severe renal impairment.1 7 (See Renal Impairment under Dosage and Administration.) Use not recommended in those with end-stage renal disease.1 7
Patients with moderate or severe renal impairment may be at increased risk for elevations in BP and heart rate because the drug's half-life is prolonged in such patients.1
Common Adverse Effects
Headache, nausea, decreased appetite, insomnia, anxiety.1 In clinical trials, headache, nausea, decreased appetite, anxiety, diarrhea, and dry mouth were dose related.1
Drug Interactions
Undergoes minimal metabolism in vitro.1 Does not inhibit CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A4 in vitro; does not induce CYP isoenzyme 1A2, 2B6, or 3A4, or uridine-diphosphate glucuronosyltransferase (UGT) 1A1 at clinically relevant concentrations.1
Low-avidity substrate of organic cation transporter (OCT) 2, multidrug and toxin extrusion transporter (MATE) 1, and organic cation transporters novel (OCTN) 1 and 2.1 Weakly inhibits OCT2 and MATE1; does not inhibit OCT1, MATE2-K, OCTN1, or OCTN2.1 Does not appear to be a substrate or inhibitor of P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), organic anion transport polypeptide (OATP) 1B1 or 1B3, or organic anion transporter (OAT) 1 or 3.1
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Clinically important interactions involving major CYP isoenzymes not expected.1
Drugs Affecting or Affected by Transport Systems
Clinically important interactions involving major transport systems not expected.1
Drugs that Increase BP or Heart Rate
Concomitant use of solriamfetol with other drugs that increase BP and/or heart rate not evaluated; use such combination therapy with caution.1 (See Cardiovascular Effects under Cautions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Dopaminergic drugs |
Possible pharmacodynamic interaction with drugs that increase dopamine concentrations or bind to dopaminergic receptors1 |
Interactions with dopaminergic drugs not evaluated to date; use concomitantly with caution1 |
|
MAO inhibitors |
Possible increased risk of hypertensive reactions, potentially resulting in death, stroke, MI, aortic dissection, ophthalmologic complications, eclampsia, pulmonary edema, and renal failure1 |
Solriamfetol is contraindicated in patients who are currently receiving or have recently (within 14 days) received an MAO inhibitor1 |
Solriamfetol Pharmacokinetics
Absorption
Bioavailability
Exhibits linear pharmacokinetics over a dose range of 42–1008 mg; once-daily administration is expected to result in minimal accumulation.1
Readily (95%) absorbed following oral administration.1 Under fasted conditions, peak plasma concentration is achieved at a median of 2 hours (range: 1.25–3 hours).1
Food
Administration with a high-fat meal delays peak plasma concentration by approximately 1 hour, but results in minimal change in peak concentration or AUC.1 6
Special Populations
Mild, moderate, or severe renal impairment (eGFR 60–89, 30–59, or <30 mL/minute per 1.73 m2, respectively): AUC increased by 53, 129, or 339%, respectively, compared with individuals with normal renal function.1 7 Renal impairment does not appreciably alter peak plasma concentration or time to peak plasma concentration.1 7
End-stage renal disease (eGFR <15 mL/minute per 1.73 m2): AUC increased by approximately fourfold (with hemodialysis) or fivefold (without hemodialysis) compared with individuals with normal renal function.7
Distribution
Extent
Not known whether distributed into human milk.1
Plasma Protein Binding
Approximately 13–19%.1
Elimination
Metabolism
Undergoes minimal metabolism.1
Elimination Route
Eliminated mainly (95%) in urine as unchanged drug; ≤1% of administered dose recovered as the minor inactive metabolite N-acetylsolriamfetol.1 Active tubular secretion is likely involved in renal clearance of the parent drug.1
Half-life
Exhibits first-order elimination with mean apparent elimination half-life of about 7.1 hours.1
Special Populations
Age, sex, and race do not have clinically important effects on the pharmacokinetics of solriamfetol.1
Mild, moderate, or severe renal impairment (eGFR 60–89, 30–59, or <30 mL/minute per 1.73 m2, respectively): Half-life is increased by approximately 1.2-, 1.9-, or 3.9-fold, respectively.1 7
End-stage renal disease (eGFR <15 mL/minute per 1.73 m2): Half-life is >100 hours.7 A 4-hour hemodialysis session removes approximately 21% of a solriamfetol dose.1 7
Stability
Storage
Oral
Tablets
20–25°C (may be exposed to 15–30°C).1
Actions
-
Binds to dopamine and norepinephrine transporters with low affinity; inhibits reuptake of dopamine and norepinephrine with low potency.1 4
-
Has no appreciable binding affinity for serotonin transporter; does not inhibit serotonin reuptake.1 4 Also has no appreciable binding affinity for dopamine, serotonin, norepinephrine, GABA, adenosine, histamine, orexin, benzodiazepine, muscarinic acetylcholine, or nicotinic acetylcholine receptors.1 4
-
Exact mechanism by which solriamfetol promotes wakefulness in patients with excessive daytime sleepiness associated with obstructive sleep apnea or narcolepsy is not known but may involve inhibition of dopamine and norepinephrine reuptake resulting from binding of the drug to dopamine and norepinephrine transporters in the brainstem arousal systems.1 4 9
Advice to Patients
-
Advise patients to read the manufacturer's patient information (medication guide).1
-
Advise patients that solriamfetol is a controlled substance and has the potential to be abused.1 Advise patients to keep their medication in a secure place and to dispose of unused solriamfetol as recommended in the medication guide.1
-
Inform patients with obstructive sleep apnea that solriamfetol is not indicated to treat the underlying airway obstruction and that they should use standard treatments (e.g., CPAP) as prescribed.1 Solriamfetol is not a substitute for such therapy.1
-
Advise patients that solriamfetol can increase BP and pulse rate and that they should be monitored for such effects.1
-
Instruct patients to contact their clinician if they experience anxiety, insomnia, irritability, agitation, or symptoms of psychosis or bipolar disorders.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 Advise women who are breast-feeding to monitor their infants for adverse effects such as agitation, insomnia, anorexia, and reduced weight gain.1 Encourage pregnant women who have been exposed to solriamfetol to enroll in the manufacturer's pregnancy registry.1 (See Pregnancy under Cautions.)
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as a schedule IV (C-IV) drug.1
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
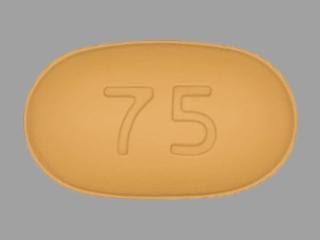
Oral |
Tablets, film-coated |
75 mg (of solriamfetol) |
Sunosi (C-IV; scored) |
Jazz |
|
150 mg (of solriamfetol) |
Sunosi (C-IV) |
Jazz |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions November 16, 2020. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Jazz Pharmaceuticals. Sunosi (solriamfetol hydrochloride) tablets prescribing information. Palo Alto, CA; 2019 Jun.
2. Thorpy MJ, Shapiro C, Mayer G et al. A randomized study of solriamfetol for excessive sleepiness in narcolepsy. Ann Neurol. 2019; 85:359-370. http://www.ncbi.nlm.nih.gov/pubmed/30694576?dopt=AbstractPlus http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=PMC6593450&blobtype=pdf
3. Schweitzer PK, Rosenberg R, Zammit GK et al. Solriamfetol for Excessive Sleepiness in Obstructive Sleep Apnea (TONES 3). A Randomized Controlled Trial. Am J Respir Crit Care Med. 2019; 199:1421-1431. http://www.ncbi.nlm.nih.gov/pubmed/30521757?dopt=AbstractPlus http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=PMC6835071&blobtype=pdf
4. Baladi MG, Forster MJ, Gatch MB et al. Characterization of the Neurochemical and Behavioral Effects of Solriamfetol (JZP-110), a Selective Dopamine and Norepinephrine Reuptake Inhibitor. J Pharmacol Exp Ther. 2018; 366:367-376. http://www.ncbi.nlm.nih.gov/pubmed/29891587?dopt=AbstractPlus
5. Thorpy MJ. Recently Approved and Upcoming Treatments for Narcolepsy. CNS Drugs. 2020; 34:9-27. http://www.ncbi.nlm.nih.gov/pubmed/31953791?dopt=AbstractPlus http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=PMC6982634&blobtype=pdf
6. Zomorodi K, Kankam M, Lu Y. A Phase I, Randomized, Crossover, Open-label Study of the Pharmacokinetics of Solriamfetol (JZP-110) in Healthy Adult Subjects With and Without Food. Clin Ther. 2019; 41:196-204. http://www.ncbi.nlm.nih.gov/pubmed/30598342?dopt=AbstractPlus
7. Zomorodi K, Chen D, Lee L et al. Single-Dose Pharmacokinetics and Safety of Solriamfetol in Participants With Normal or Impaired Renal Function and With End-Stage Renal Disease Requiring Hemodialysis. J Clin Pharmacol. 2019; 59:1120-1129. http://www.ncbi.nlm.nih.gov/pubmed/30865315?dopt=AbstractPlus http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=PMC6618134&blobtype=pdf
8. Carter LP, Henningfield JE, Wang YG et al. A randomized, double-blind, placebo-controlled, crossover study to evaluate the human abuse liability of solriamfetol, a selective dopamine and norepinephrine reuptake inhibitor. J Psychopharmacol. 2018; 32:1351-1361. http://www.ncbi.nlm.nih.gov/pubmed/30269642?dopt=AbstractPlus http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=PMC6247449&blobtype=pdf
9. US Food and Drug Administration. Center for Drug Evaluation and Research. Application numbers 211230Orig1s000 and 211230Orig2s000: Summary review. From FDA website. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/211230Orig1Orig2s000SumR.pdf
10. Malhotra A, Shapiro C, Pepin JL et al. Long-term study of the safety and maintenance of efficacy of solriamfetol (JZP-110) in the treatment of excessive sleepiness in participants with narcolepsy or obstructive sleep apnea. Sleep. 2020; 43 http://www.ncbi.nlm.nih.gov/pubmed/31691827?dopt=AbstractPlus
11. Strollo PJ Jr, Hedner J, Collop N et al. Solriamfetol for the Treatment of Excessive Sleepiness in OSA: A Placebo-Controlled Randomized Withdrawal Study. Chest. 2019; 155:364-374. http://www.ncbi.nlm.nih.gov/pubmed/30471270?dopt=AbstractPlus
12. Sahni AS, Carlucci M, Malik M et al. Management Of Excessive Sleepiness In Patients With Narcolepsy And OSA: Current Challenges And Future Prospects. Nat Sci Sleep. 2019; 11:241-252. http://www.ncbi.nlm.nih.gov/pubmed/31695533?dopt=AbstractPlus http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=PMC6815780&blobtype=pdf
13. Food and Drug Administration. FDA Application: Search Orphan Drug Designations and Approvals. Silver Spring, MD/scripts/opdlisting/oopd/index.cfm). Accessed 2020 Jul 10. https://www.accessdata.fda.gov/scripts/opdlisting/oopd/index.cfm)
Frequently asked questions
More about solriamfetol
- Check interactions
- Compare alternatives
- Reviews (77)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous central nervous system agents
- Breastfeeding
- En español