Rufinamide (Monograph)
Brand name: Banzel
Drug class: Ion Channel Inhibition Agents
- Anticonvulsant, triazole derivative
Introduction
Anticonvulsant; a triazole derivative.1 6 7 9 10 11 12 13 14 15 17 18
Uses for Rufinamide
Seizure Disorders
Adjunctive therapy (i.e., in combination with other anticonvulsants) of seizures associated with Lennox-Gastaut syndrome in adults and pediatric patients ≥1 year of age.1 5 6 8 9 10 11 28 35 Designated an orphan drug by FDA for use in this condition.5 8 10
Has been studied with some success in the adjunctive management of refractory or inadequately controlled partial seizures† [off-label] in adolescents and adults;6 7 10 11 12 13 16 17 18 19 21 22 24 25 29 30 further study needed to establish role in therapy.11 19
Rufinamide Dosage and Administration
General
-
Withdraw rufinamide gradually when discontinuing therapy to minimize the potential for increased seizure frequency or status epilepticus.1 (See Discontinuance of Therapy under Cautions.) If abrupt discontinuance is necessary, closely supervise transition to another anticonvulsant.1
-
Closely monitor for notable changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression.1 2 4 20 (See Suicidality Risk under Cautions.)
Administration
Oral Administration
Administer orally as tablets or oral suspension twice daily in equally divided doses with food.1
Tablets
Administer scored tablets whole, as half tablets, or crushed.1 21
Scored tablets may not provide the exact mg/kg dosage that has been calculated for use in children; manufacturer’s recommended dosages in children are therefore designated as approximate.1 21
Oral Suspension
Shake well prior to administration of each dose.1
Administer using bottle adapter and calibrated oral dosing syringe supplied by manufacturer.1
Firmly insert bottle adapter into neck of bottle before first use; allow adapter to remain in place as long as bottle is in use (up to 90 days).1
Dosage
Pediatric Patients
Seizure Disorders
Adjunctive Therapy in Lennox-Gastaut Syndrome
OralChildren and adolescents 1 to <17 years of age: Initially, approximately 10 mg/kg daily administered in 2 equally divided doses.1 Increase dosage in increments of approximately 10 mg/kg every other day up to a maximum dosage of 45 mg/kg (not to exceed 3.2 g) daily.1 Efficacy of dosages lower than the target dosage has not been established.1
Initiate therapy at a dosage lower than 10 mg/kg daily in patients receiving valproic acid.1 11 (See Specific Drugs under Interactions.)
Reduce dosage gradually if discontinuing therapy.1 In clinical trials, rufinamide dosage was tapered by approximately 25% every other day.1
Adults
Seizure Disorders
Adjunctive Therapy in Lennox-Gastaut Syndrome
OralAdults ≥17 years of age: Initially, 400–800 mg daily administered in 2 equally divided doses.1 Increase dosage in increments of 400–800 mg daily every other day until a maximum dosage of 3.2 g daily is reached.1 Efficacy of dosages lower than 3.2 g daily has not been established.1
Initiate therapy at a dosage lower than 400 mg daily in patients receiving valproic acid.1 11 (See Specific Drugs under Interactions.)
Reduce dosage gradually if discontinuing therapy.1 In clinical trials, rufinamide dosage was tapered by approximately 25% every other day.1
Prescribing Limits
Pediatric Patients
Seizure Disorders
Adjunctive Therapy in Lennox-Gastaut Syndrome
OralChildren and adolescents 1 to <17 years of age: Maximum 3.2 g daily.1
Adults
Seizure Disorders
Adjunctive Therapy in Lennox-Gastaut Syndrome
OralMaximum 3.2 g daily.1
Special Populations
Hepatic Impairment
Not studied in patients with hepatic impairment.1 21 (See Hepatic Impairment under Cautions.)
Renal Impairment
Consider dosage adjustment in hemodialysis patients; hemodialysis within 3 hours after a dose may reduce drug exposure to a limited extent (by about 30%).1 11 21
Geriatric Patients
Select dosage carefully, usually initiating therapy at lower end of usual dosage range, because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.1 10 (See Geriatric Use under Cautions.)
Cautions for Rufinamide
Contraindications
Warnings/Precautions
Sensitivity Reactions
Multi-organ Hypersensitivity Reactions
Multi-organ hypersensitivity (also known as drug reaction with eosinophilia and systemic symptoms [DRESS]) reported; can be fatal or life-threatening.1 32 Clinical presentation is variable but typically includes fever, rash, and/or lymphadenopathy associated with other organ system involvement (e.g., eosinophilia, hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis).1
In clinical studies, reported in children <12 years of age within 4 weeks of treatment initiation; resolved or improved following drug discontinuance.1 Also reported in adults and older pediatric patients during postmarketing experience.1
If manifestations of multi-organ hypersensitivity occur, evaluate patient immediately.1 Discontinue rufinamide and initiate alternative treatment.1 21
Serious Dermatologic Reactions
Serious dermatologic reactions, including Stevens-Johnson syndrome and other serious rashes, reported during postmarketing experience.1
Suicidality Risk
Increased risk of suicidality (suicidal behavior or ideation) observed in an analysis of studies using various anticonvulsants in patients with epilepsy, psychiatric disorders (e.g., bipolar disorder, depression, anxiety), and other conditions (e.g., migraine, neuropathic pain); risk in patients receiving anticonvulsants (0.43%) was approximately twice that in patients receiving placebo (0.24%).1 2 4 20 Increased suicidality risk was observed ≥1 week after initiation of anticonvulsant therapy and continued through 24 weeks.1 2 4 Risk was higher for patients with epilepsy compared with those receiving anticonvulsants for other conditions.1 2 4
Closely monitor all patients currently receiving or beginning anticonvulsant therapy for changes in behavior that may indicate emergence or worsening of suicidal thoughts or behavior or depression.1 2 4 20
Balance risk of suicidality with risk of untreated illness.1 2 Epilepsy and other illnesses treated with anticonvulsants are themselves associated with morbidity and mortality and an increased risk of suicidality.1 20 If suicidal thoughts or behavior emerges during anticonvulsant therapy, consider whether these symptoms may be related to the illness itself.1 20 (See Advice to Patients.)
CNS Effects
Two general categories of adverse CNS effects reported: 1) somnolence or fatigue, and 2) coordination abnormalities, dizziness, gait disturbances, and ataxia.1 (See Advice to Patients.)
Shortening of QT Interval
Shortening of QT interval reported;1 reported degree of shortening (mean of 20 msec at dosages ≥2.4 mg twice daily) is without known clinical risk.1 11
Familial short QT syndrome is associated with increased risk of sudden death and ventricular arrhythmias, particularly ventricular fibrillation, primarily when the corrected QT (QTc) interval is <300 msec.1 Nonclinical data indicate QT-interval shortening is associated with ventricular fibrillation.1
Manufacturer and some clinicians state that patients with familial short QT syndrome should not receive rufinamide; caution advised when administering rufinamide with other drugs that shorten the QT interval.1 11 21 28 Some clinicians recommend using rufinamide with caution in patients with a history of an abnormal ECG demonstrating QT-interval shortening or a family history of unexplained cardiac arrhythmia or sudden death.28 (See Contraindications under Cautions and also see Drugs that Shorten QT Interval under Interactions.)
Discontinuance of Therapy
Abrupt withdrawal of anticonvulsants may result in increased seizure frequency or status epilepticus in patients with seizure disorders.1 If discontinuing therapy, withdraw rufinamide gradually (see Dosage under Dosage and Administration).1 If abrupt discontinuance is necessary, closely supervise transition to another anticonvulsant.1
Status Epilepticus
Seizure episodes that could be described as status epilepticus reported.1 However, incidence of treatment-emergent status epilepticus not known.1 9
Hematologic Effects
Leukopenia reported in patients receiving rufinamide in clinical studies.1
Specific Populations
Pregnancy
Category C.1 No adequate and well-controlled studies in pregnant women; developmental toxicity observed in animal studies.1
North American Antiepileptic Drug (NAAED) Pregnancy Registry at 888-233-2334 (for patients); NAAED registry information also available on the website [Web].1
Lactation
Likely to be distributed into milk.1 21 Discontinue nursing or the drug.1 21
Pediatric Use
Safety and efficacy not established in children <1 year of age.1
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger patients.1 No clinically important differences in pharmacokinetics between healthy geriatric individuals and younger healthy adults.1 (See Geriatric Patients under Dosage and Administration.)
Hepatic Impairment
Not studied in hepatic impairment.1 Use with caution in patients with mild to moderate hepatic impairment.1 Use in severe hepatic impairment not recommended.1
Renal Impairment
Renal impairment (Clcr <30 mL/minute) does not substantially alter pharmacokinetics; hemodialysis may reduce exposure.1 (See Renal Impairment under Dosage and Administration and also see Absorption: Special Populations and Elimination: Special Populations, under Pharmacokinetics.)
Common Adverse Effects
Adjunctive therapy in pediatric patients: Somnolence, headache, fatigue, dizziness, influenza, nasopharyngitis, nausea, vomiting, decreased appetite, constipation, stomach pain, decreased weight, cough, sinusitis, bronchitis, pneumonia, otitis media, rash, pruritus, ataxia, diplopia, aggression, hyperactivity, disturbance in attention.1 6 9 10 11 13 14 15 21 35
Adjunctive therapy in adults: Headache, dizziness, fatigue, somnolence, diplopia, tremor, nystagmus, blurred vision, nausea, vomiting, stomach pain, constipation, dyspepsia, ataxia, anxiety, back pain, gait disturbance, vertigo.1 6 9 10 11 13 14 15 21
Drug Interactions
Metabolized by carboxylesterases.1
Demonstrates little or no inhibition of most CYP isoenzymes.1 8 Weak inhibitor of CYP2E1;1 21 weak inducer of CYP3A4.1 11 14 21
Unlikely to be involved in clinically important pharmacokinetic interactions.1
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP2E1: Potential pharmacokinetic interaction (increased plasma substrate concentrations).1 21 (See Specific Drugs under Interactions.)
Substrates of CYP3A4: Potential pharmacokinetic interaction (decreased exposure of substrates).1 11 14 21 (See Specific Drugs under Interactions.)
Inducers of carboxylesterases: Potential pharmacokinetic interaction (increased rufinamide clearance); broad-spectrum inducers may have minor effects on rufinamide metabolism via this mechanism.1 (See Specific Drugs under Interactions.)
Inhibitors of carboxylesterases: Potential pharmacokinetic interaction (decreased rufinamide metabolism).1 8
Anticonvulsants
Typical average steady-state plasma rufinamide concentrations generally have little effect on the pharmacokinetics of other anticonvulsants.1 Effects, when present, are more marked in pediatric patients.1 (See Specific Drugs under Interactions.)
Clinical importance of drug interactions between rufinamide and potentially interacting anticonvulsants is unknown; some clinicians recommend monitoring plasma concentrations of other anticonvulsants and rufinamide following initiation or withdrawal of anticonvulsant therapy if clinically warranted.28
Drugs that Shorten QT Interval
Potential pharmacologic interaction; use concomitantly with caution.1 21 23 (See Specific Drugs under Interactions and see Shortening of QT Interval under Cautions.)
Protein-bound Drugs
Pharmacokinetic interaction unlikely; not highly bound to plasma proteins.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Benzodiazepines |
Clinically important pharmacokinetic interactions unlikely; however, possible additive CNS effects1 13 21 24 Clonazepam: Pharmacokinetic interaction unlikely6 13 24 Triazolam: Decreased triazolam AUC (by 37%) and peak plasma concentrations (by 23%)1 11 12 |
|
|
Carbamazepine |
Decreased plasma carbamazepine concentrations (by 7–13%)1 Decreased plasma rufinamide concentrations (by 19–26% depending on carbamazepine dosage)1 |
|
|
Chlorzoxazone |
||
|
CNS agents (e.g., alcohol, benzodiazepines) |
||
|
Contraceptives, oral |
Decreased AUC and peak plasma concentrations of ethinyl estradiol (by 22 and 31%, respectively) and norethindrone (by 14 and 18%, respectively)1 8 10 11 12 14 15 18 23 |
Additional nonhormonal contraceptive methods recommended1 10 21 |
|
Digoxin |
||
|
Lamotrigine |
Decreased plasma lamotrigine concentrations (by 7–13%)1 |
|
|
Magnesium |
||
|
Mexiletine |
||
|
Oxcarbazepine |
||
|
Phenobarbital |
Increased plasma phenobarbital concentrations (by 8–13%)1 Decreased plasma rufinamide concentrations (by 25–46% independent of phenobarbital dosage or concentration)1 |
|
|
Phenytoin |
Increased plasma phenytoin concentrations (by 7–21%)1 Decreased plasma rufinamide concentrations (by 25–46% independent of phenytoin dosage or concentration)1 |
|
|
Primidone |
Decreased plasma rufinamide concentrations (by 25–46% independent of primidone dosage or concentration)1 |
|
|
Ranolazine |
||
|
Topiramate |
Pharmacokinetic interaction unlikely1 |
|
|
Valproate |
Increased plasma rufinamide concentrations (by <16 to 70% depending on valproate concentration); may be more pronounced in pediatric patients1 10 11 12 13 14 16 18 21 23 24 26 27 |
In patients stabilized on rufinamide, initiate valproic acid at low dosage and titrate to clinically effective dosage1 In patients receiving valproic acid, initiate rufinamide at dosage <400 mg daily in adults and <10 mg/kg daily in children1 11 |
Rufinamide Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration; peak plasma concentrations occur 4–6 hours after a dose.1 Extent of absorption decreases with increasing doses.1
Food
Food increased the extent of absorption and peak exposure of a single 400-mg dose by 34 and 56%, respectively.1
Under fed conditions, ≥85% of a single 600-mg dose was absorbed.1
Special Populations
Peak plasma concentrations and AUC are decreased by 16 and 29%, respectively, at 3 hours after a hemodialysis session.1
Distribution
Plasma Protein Binding
Elimination
Metabolism
Extensively metabolized, primarily via carboxylesterase-mediated hydrolysis of the carboxylamide group to an inactive acid derivative (CGP 47292).1 6 8 10 11 12 13 14 15 16 17 18 21 Metabolic pathways do not involve CYP isoenzymes and glutathione.1 6 8 10 12 16 18
Elimination Route
Eliminated principally in urine (85%), mostly as metabolites (≥66% as CGP 47292); only 2% of dose is excreted as unchanged drug.1 6 8 10 11 12 13 15 16 17 18 21
Half-life
Special Populations
Effect of hepatic impairment on pharmacokinetics not evaluated.1
Renal impairment (Clcr <30 mL/minute) does not substantially alter pharmacokinetics; hemodialysis may reduce exposure (see Absorption: Special Populations under Pharmacokinetics).1
No clinically important pharmacokinetic differences between healthy geriatric individuals and younger adults.1
Stability
Storage
Oral
Suspension
25°C (may be exposed to 15–30°C).1
Tablets
25°C (may be exposed to 15–30°).1 Protect from moisture.1
Actions
-
Triazole-derivative anticonvulsant; structurally unrelated to other currently available anticonvulsants.1 6 7 9 10 11 12 13 14 15 16 17 18 21 28
-
Exact mechanism(s) of anticonvulsant action is unknown, but may involve modulation of sodium channel activity and, in particular, prolongation of the inactive state of the channel.1 6 7 9 10 11 12 13 14 15 16 17 18 21
-
Does not appear to substantially interact with monoaminergic, cholinergic, histaminergic, glycine, GABA, or glutamate receptors or systems.6 7 10 13 14 17 18
Advice to Patients
-
Importance of providing copy of written patient information (medication guide) each time rufinamide is dispensed.1 20 Importance of patients reading this information prior to taking the drug.1
-
Risk of suicidality (anticonvulsants, including rufinamide, may increase risk of suicidal thoughts or actions in about 1 in 500 people).1 2 20 Importance of patients, family members, and caregivers being alert to day-to-day changes in mood, behavior, and actions and immediately informing clinician of any new or worrisome behaviors (e.g., talking or thinking about wanting to hurt oneself or end ones life, withdrawing from friends and family, becoming depressed or experiencing worsening of existing depression, becoming preoccupied with death and dying, giving away prized possessions).1 2
-
Risk of multi-organ hypersensitivity.1 Importance of notifying clinician if rash (with or without fever) occurs.1
-
Importance of taking rufinamide only as prescribed.1
-
Importance of taking rufinamide with food.1 Importance of informing patients that rufinamide scored tablets may be swallowed whole, broken in half, or crushed.1 Importance of instructing patients in proper techniques for administration of the oral suspension, including use of the bottle adapter and oral dosing syringe.1
-
When applicable, advise patients that rufinamide oral suspension does not contain lactose, gluten, or carbohydrates and is dye-free.1
-
Risk of sleepiness, difficulty with coordination, and dizziness; importance of advising patients to avoid driving or operating machinery until they gain experience with the drug’s effects.1 21 Risk of additive CNS effects (e.g., sedation) if used with alcohol or other drugs that affect the CNS.1 21
-
Importance of informing patients not to stop taking rufinamide without first talking to their clinician since stopping the drug suddenly can cause serious problems, including seizures.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 Importance of clinicians informing women about the existence of and encouraging enrollment in pregnancy registries (see Pregnancy under Cautions).1 Potential increased risk of pregnancy in women taking hormonal contraceptives; importance of discussing use of additional contraceptive methods.1 10 21
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses (e.g., hepatic disease, depression, bipolar disorder), family history of suicidality or bipolar disorder, or current diagnosis or history of familial short QT syndrome.1
-
Importance of advising patients of other important precautionary information.1 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Suspension |
40 mg/mL |
Banzel |
Eisai |
|
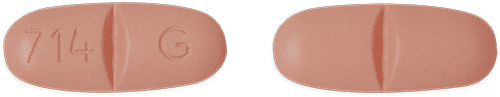
Tablets, film-coated |
200 mg* |
Banzel (scored) |
Eisai |
|
|
Rufinamide Tablets (scored) |
||||
|
400 mg* |
Banzel (scored) |
Eisai |
||
|
Rufinamide Tablets (scored) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Eisai Co., Ltd. Banzel (rufinamide) tablets prescribing information. Woodcliff Lake, NJ; 2015 Jun.
2. Food and Drug Administration. FDA Alert: Information for healthcare professionals: suicidality and antiepileptic drugs. Rockville, MD; 2008 Jan 31. From the FDA website.
4. Food and Drug Administration. FDA Alert: Suicidality and antiepileptic drugs. Rockville, MD; 2008 Jan 31. From the FDA website.
5. Food and Drug Administration. Orphan designations pursuant to Section 526 of the Federal Food and Cosmetic Act as amended by the Orphan Drug Act (P.L. 97 414). Rockville, MD. From FDA website. Accessed 2009 Apr 22. http://www.accessdata.fda.gov/scripts/opdlisting/oopd/index.cfm
6. Heaney D, Walker MC. Rufinamide. Drugs Today (Barc). 2007; 43:455-60. https://pubmed.ncbi.nlm.nih.gov/17728846
7. Rogawski MA. Diverse mechanisms of antiepileptic drugs in the development pipeline. Epilepsy Res. 2006; 69:273-94. https://pubmed.ncbi.nlm.nih.gov/16621450 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1562526/
8. Perucca E, Cloyd J, Critchley D et al. Rufinamide: clinical pharmacokinetics and concentration-response relationships in patients with epilepsy. Epilepsia. 2008; 49:1123-41. https://pubmed.ncbi.nlm.nih.gov/18503564
9. Glauser T, Kluger G, Sachdeo R et al. Rufinamide for generalized seizures associated with Lennox-Gastaut syndrome. Neurology. 2008; 70:1950-8. https://pubmed.ncbi.nlm.nih.gov/18401024
10. Cheng-Hakimian A, Anderson GD, Miller JW. Rufinamide: pharmacology, clinical trials, and role in clinical practice. Int J Clin Pract. 2006; 60:1497-501. https://pubmed.ncbi.nlm.nih.gov/17073844
11. . Rufinamide (Banzel) for epilepsy. Med Lett Drugs Ther. 2009; 51:18-20. https://pubmed.ncbi.nlm.nih.gov/19265777
12. Deeks ED, Scott LJ. Rufinamide. CNS Drugs. 2006; 20:751-60; discussion 761. https://pubmed.ncbi.nlm.nih.gov/16953653
13. Hakimian S, Cheng-Hakimian A, Anderson GD et al. Rufinamide: a new anti-epileptic medication. Expert Opin Pharmacother. 2007; 8:1931-40. https://pubmed.ncbi.nlm.nih.gov/17696794
14. Johannessen Landmark C, Johannessen SI. Pharmacological management of epilepsy: recent advances and future prospects. Drugs. 2008; 68:1925-39. https://pubmed.ncbi.nlm.nih.gov/18778117
15. Chung AM, Eiland LS. Use of second-generation antiepileptic drugs in the pediatric population. Paediatr Drugs. 2008; 10:217-54. https://pubmed.ncbi.nlm.nih.gov/18590343
16. Bialer M, Johannessen SI, Kupferberg HJ et al. Progress report on new antiepileptic drugs: a summary of the Eighth Eilat Conference (EILAT VIII). Epilepsy Res. 2007; 73:1-52. https://pubmed.ncbi.nlm.nih.gov/17158031
17. Bialer M, Johannessen SI, Kupferberg HJ et al. Progress report on new antiepileptic drugs: a summary of the Fifth Eilat Conference (EILAT V). Epilepsy Res. 2001; 43:11-58. https://pubmed.ncbi.nlm.nih.gov/11137386
18. Arroyo S. Rufinamide. Neurotherapeutics. 2007; 4:155-62. https://pubmed.ncbi.nlm.nih.gov/17199032
19. Pålhagen S, Canger R, Henriksen O et al. Rufinamide: a double-blind, placebo-controlled proof of principle trial in patients with epilepsy. Epilepsy Res. 2001; 43:115-24. https://pubmed.ncbi.nlm.nih.gov/11164700
20. Food and Drug Administration. Suicidal behavior and ideation and antiepileptic drugs: update 5/5/2009. Rockville, MD; 2009 May 5. From the FDA website.
21. Hussar DA, Bilbow C. New drugs: Febuxostat, lacosamide, and rufinamide. J Am Pharm Assoc. 2009; 49:460-3.
22. Glauser T, Kluger G, Sachdeo R et al. Open-label study of the efficacy and safety of rufinamide adjunctive therapy in patients with Lennox-Gastaut syndrome. Epilepsia. 2005; 46 (Suppl. 6):408. Abstr. p1356.
23. Eisai Inc., Woodcliff Lake, NJ: Personal communication.
24. Luszczki JJ. Third-generation antiepileptic drugs: mechanisms of action, pharmacokinetics and interactions. Pharmacol Rep. 2009 Mar-Apr; 61:197-216.
25. Herman ST. Adopting an orphan drug: rufinamide for lennox-gastaut syndrome. Epilepsy Curr. 2009 May-Jun; 9:72-4.
26. Kluger G, Bauer B. Role of rufinamide in the management of Lennox-Gastaut syndrome (childhood epileptic encephalopathy). Neuropsychiatr Dis Treat. 2007; 3:3-11. https://pubmed.ncbi.nlm.nih.gov/19300535 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2654531/
27. Ferrie CD, Patel A. Treatment of Lennox-Gastaut Syndrome (LGS). Eur J Paediatr Neurol. 2009; : [epub ahead of print].. https://pubmed.ncbi.nlm.nih.gov/19211283 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3902105/
28. Saneto RP, Anderson GD. Onset of action and seizure control in Lennox-Gastaut syndrome. Ther Clin Risk Manag. 2009; 5:271-80. https://pubmed.ncbi.nlm.nih.gov/19536315 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2697537/
29. Brodie MJ, Rosenfeld WE, Vazquez B et al. Rufinamide for the adjunctive treatment of partial seizures in adults and adolescents: a randomized placebo-controlled trial. Epilepsia. 2009; Jun 1: 1-11.
30. Kluger G, Kurlemann G, Haberlandt E et al. Effectiveness and tolerability of rufinamide in children and adults with refractory epilepsy: first European experience. Epilepsy Behav. 2009; 14:491-5. https://pubmed.ncbi.nlm.nih.gov/19162229
32. Krivoy N, Taer M, Neuman MG. Antiepileptic drug-induced hypersensitivity syndrome reactions. Curr Drug Safety. 2006; 1:288-99.
35. Arzimanoglou A, Ferreira JA, Satlin, A et al. Safety and pharmacokinetic profile of rufinamide in pediatric patients aged less than 4 years with Lennox-Gastaut syndrome: An interim analysis from a multicenter, randomized, active-controlled, open-label study.(LGS). Eur J Paediatr Neurol. 2016; :393-402.
Related/similar drugs
Frequently asked questions
More about rufinamide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (9)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: dibenzazepine anticonvulsants
- Breastfeeding
- En español