Nelfinavir Mesylate (Monograph)
Brand name: Viracept
Drug class: HIV Protease Inhibitors
Introduction
Antiretroviral; HIV protease inhibitor (PI).1
Uses for Nelfinavir Mesylate
Treatment of HIV Infection
Treatment of HIV-1 infection in adults and pediatric patients ≥2 years of age; used in conjunction with other antiretroviral agents.1
Nelfinavir, a protease inhibitor (PI), was previously a component of a fully suppressive antiretroviral regimen; however, guidelines no longer recommend its use due to inferior virological efficacy and toxicities.200 201 202 Consult guidelines for the most current information on recommended regimens.200 201 202 Selection of an initial antiretroviral regimen should be individualized based on factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance test results, comorbid conditions, access, and cost.200 201 202
Nelfinavir Mesylate Dosage and Administration
General
Patient Monitoring
-
Consider monitoring for hyperglycemia, new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus.1
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) list of error-prone abbreviations, symbols, and dose designations states that the use of abbreviations for antiretroviral medications (e.g., DOR, TAF, TDF) during the medication use process should be avoided as their use has been associated with serious medication errors.503
Administration
Oral Administration
Administer orally 2 or 3 times daily with a meal.1
Commercially available as tablets (an oral powder for solution was discontinued).1
For patients unable to swallow tablets, place appropriate dose of 250-mg tablets in small amount of water and allow to disperse.1 After tablets dissolve, mix the cloudy liquid well and immediately consume.1 To ensure that entire dose is consumed, rinse glass with water and swallow the rinse.1
Do not mix nelfinavir tablets with acidic food or juice (e.g., apple juice, applesauce, orange juice) since the mixture may have a bitter taste.1
If a dose of nelfinavir is missed, take the dose as soon as it is remembered and the next dose at the regularly scheduled time.1 If a dose is skipped, do not administer a double dose to make up for the missed dose.1
Dosage
Available as nelfinavir mesylate; dosage expressed as nelfinavir.1
Pediatric Patients
Treatment of HIV Infection
Oral
Pediatric HIV guidelines no longer recommend the use of nelfinavir in children or adolescents due to its variable pharmacokinetics and inferior efficacy.201
Children 2 to <13 years of age: 45–55 mg/kg twice daily or 25–35 mg/kg three times daily using 250-mg tablets.1
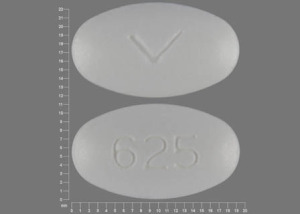
Children ≥13 years of age: 1.25 g (five 250-mg tablets or two 625-mg tablets) twice daily or 750 mg (three 250-mg tablets) three times daily.1
See Full Prescribing Information for additional dosing guidelines for nelfinavir tablets based on age and body weight.1
Adults
Treatment of HIV Infection
Oral
1.25 g (five 250-mg tablets or two 625-mg tablets) twice daily or 750 mg (three 250-mg tablets) three times daily.1
Special Populations
Hepatic Impairment
Dosage adjustment not needed in patients with mild hepatic impairment (Child-Pugh class A, score 5–6).1 Do not use in patients with moderate or severe hepatic impairment (Child-Pugh class B or C, score ≥7).1
Renal Impairment
Safety and efficacy not established.1
Geriatric Patients
No specific dosage recommendations.1
Cautions for Nelfinavir Mesylate
Contraindications
-
Concomitant use with drugs highly dependent on CYP3A for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening events (e.g., alfuzosin, amiodarone, cisapride, ergot alkaloids, oral midazolam, pimozide, quinidine, sildenafil used for treatment of pulmonary arterial hypertension [PAH], triazolam).1
-
Concomitant use with drugs that are CYP3A inducers where significantly reduced nelfinavir plasma concentrations may be associated with a potential loss of virologic response, and possible development of resistance or cross-resistance to other antiretrovirals (e.g., rifampin, St. John’s wort [Hypericum perforatum].1
Warnings/Precautions
Risk of Serious Adverse Reactions Due to Drug Interactions
Concomitant use with certain drugs not recommended or requires particular caution.1
Hepatic Impairment
Metabolized in the liver.1 Plasma concentrations of nelfinavir increased in patients with moderate hepatic impairment; do not use in moderate or severe hepatic impairment (Child-Pugh class B or C, score ≥7).1
Diabetes Mellitus/Hyperglycemia
Hyperglycemia, new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus reported with use of HIV protease inhibitors (PIs); diabetic ketoacidosis has occurred.1
Hemophilia
Increased bleeding, including spontaneous skin hematomas and hemarthrosis, reported with PIs; causal relationship not established.1
Increased hemostatic (e.g., factor VIII) therapy may be needed.1
Fat Redistribution
Possible redistribution or accumulation of body fat, including central obesity, dorsocervical fat enlargement (“buffalo hump”), peripheral wasting, breast enlargement, and general cushingoid appearance.1 Mechanisms and long-term consequences of fat redistribution unknown; causal relationship not established.1
Immune Reconstitution Syndrome
During initial treatment, patients who respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium complex [MAC], M. tuberculosis, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii]); this may necessitate further evaluation and treatment.1
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome) reported in the setting of immune reconstitution; time to onset is variable and can occur many months after initiation of antiretroviral therapy.1
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry at 800-258-4263 or [Web].1
Hepatic adverse effects, including hepatic enzyme elevations and hepatic failure, reported in pregnant patients exposed to nelfinavir; consider alternative antiretroviral agents during pregnancy.1
Lactation
Limited data indicate nelfinavir is present in human breastmilk.1
Per HHS perinatal HIV transmission guideline, inform patients that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates postnatal HIV transmission risk to the infant.202 Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces risk of breastfeeding HIV transmission to <1%, but not does not completely eliminate risk.202 Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.202
Females and Males of Reproductive Potential
May reduce efficacy of estrogen-containing oral contraceptives.1 Advise patients receiving nelfinavir and using oral contraceptives containing ethinyl estradiol or norethindrone to use additional or alternative contraceptives.1
Pediatric Use
Safety and efficacy not established in pediatric patients <2 years of age.1 Some data collected in this age group, but reliably effective dosage not established.1 Some evidence that those <2 years of age have a lower response rate than older pediatric patients.1
Consider that use of nelfinavir in pediatric patients is associated with highly variable drug exposure.1
Geriatric Use
Insufficient experience in those ≥65 years of age to determine whether they respond differently than younger adults.1
Hepatic Impairment
Do not use in patients with moderate or severe hepatic impairment (Child-Pugh B or C, score ≥7).1
Renal Impairment
Safety and efficacy not established in patients with renal impairment.1
Common Adverse Effects
Adverse effects (≥2%) of adult and adolescent patients ≥13 years of age include: diarrhea, nausea, rash, flatulence.1
Most commonly reported adverse effects in pediatric patients 2 to <13 years of age include: diarrhea, leukopenia/neutropenia, rash, anorexia, abdominal pain.1
Drug Interactions
Metabolized by CYP3A and CYP2C19.1
Inhibits CYP3A; does not inhibit CYP2D6, CYP2C9, CYP2C19, CYP2C8, CYP1A2, or CYP2E1.1
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions likely with drugs that are inhibitors, inducers, or substrates of CYP3A or CYP2C19 with possible alteration in metabolism of nelfinavir and/or other drug.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abacavir |
In vitro evidence of synergistic antiretroviral effects1 |
|
|
Alfuzosin |
Possible increased alfuzosin concentrations; may result in hypotension1 |
Concomitant use contraindicated1 |
|
Antiarrhythmic agents (amiodarone, quinidine) |
Possible increased antiarrhythmic agent concentrations; potential for serious or life-threatening effects (e.g., cardiac arrhythmias)1 |
Concomitant use with amiodarone or quinidine contraindicated1 |
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Decreased phenytoin concentrations and AUC; no change in nelfinavir concentrations1 Possible decreased nelfinavir concentrations with carbamazepine or phenobarbital1 |
Monitor phenytoin concentrations; adjustment of phenytoin dosage may be needed 1 |
|
Antifungals, azoles (ketoconazole) |
Ketoconazole: Increased nelfinavir concentrations and AUC1 |
|
|
Antimycobacterials (rifabutin, rifampin) |
Rifabutin: Increased rifabutin concentrations; decreased nelfinavir concentrations1 Rifampin: Decreased nelfinavir concentrations; possible decreased antiretroviral activity and development of resistance1 |
Rifabutin: Reduce rifabutin dosage by 50%; nelfinavir 1.25 g twice daily is preferred regimen when concomitant therapy is necessary1 Rifampin: Concomitant use contraindicated1 |
|
Benzodiazepines (e.g., midazolam, triazolam) |
Pharmacokinetic interaction with midazolam or triazolam; potential for prolonged or increased sedation or respiratory depression1 |
Concomitant use with oral midazolam or triazolam contraindicated1 |
|
Bosentan |
Possible increased bosentan concentrations1 |
If bosentan and nelfinavir used concomitantly, initiate or adjust bosentan dosage to 62.5 mg once daily or every other day based on individual tolerability1 |
|
Cisapride |
Pharmacokinetic interaction; potential for serious or life-threatening reactions (e.g., cardiac arrhythmias)1 |
Concomitant use contraindicated1 |
|
Colchicine |
Possible increased colchicine concentrations1 |
Patients with renal or hepatic impairment: Avoid concomitant use of colchicine and nelfinavir1 Colchicine for treatment of gout flares: In those receiving nelfinavir, use initial colchicine dose of 0.6 mg followed by 0.3 mg 1 hour later; repeat dose no earlier than 3 days later1 Colchicine for prophylaxis of gout flares: In those receiving nelfinavir, decrease colchicine dosage to 0.3 mg once daily in those originally receiving 0.6 mg twice daily or decrease dosage to 0.3 mg once every other day in those originally receiving 0.6 once daily1 Colchicine for treatment of familial Mediterranean fever (FMF): In those receiving nelfinavir, use maximum colchicine dosage of 0.6 mg daily (may be given as 0.3 mg twice daily)1 |
|
Corticosteroids (fluticasone) |
Fluticasone (orally inhaled, intranasal): Possible increased fluticasone concentrations1 |
Fluticasone (orally inhaled, intranasal): Consider alternatives in patients receiving nelfinavir, especially when long-term use of the corticosteroid is anticipated1 |
|
Didanosine |
No change in nelfinavir concentrations when didanosine administered 1 hour before nelfinavir1 In vitro evidence of additive antiretroviral effects1 |
Administer didanosine (without food) 1 hour before or 2 hours after nelfinavir (with food)1 |
|
Efavirenz |
Increased nelfinavir concentrations and AUC; decreased efavirenz concentrations and AUC1 In vitro evidence of additive to synergistic antiretroviral effects1 |
|
|
Ergot alkaloids (dihydroergotamine, ergotamine, methylergonovine) |
Possibility of pharmacokinetic interaction; potential for serious or life-threatening reactions (e.g., acute ergot toxicity)1 |
Concomitant use contraindicated1 |
|
Estrogens/Progestins |
Hormonal contraceptives: Decreased concentrations of ethinyl estradiol and norethindrone1 |
Use alternative or concomitant nonhormonal contraceptive measures1 |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin, lovastatin, rosuvastatin, simvastatin: Increased concentrations of the statin, increased risk of statin-associated adverse effects, including myopathy and rhabdomyolysis1 |
Atorvastatin: Do not exceed atorvastatin dosage of 40 mg daily; carefully titrate atorvastatin dosage and use lowest necessary dosage1 Lovastatin: Concomitant use with nelfinavir contraindicated1 Simvastatin: Concomitant use contraindicated1 |
|
Immunosuppressive agents |
Cyclosporine, sirolimus, tacrolimus: Possible increased concentrations of nelfinavir and the immunosuppressive agents1 |
|
|
Lamivudine |
Increased lamivudine peak concentrations and AUC1 In vitro evidence of additive or synergistic antiretroviral effects1 |
|
|
Macrolides (azithromycin) |
Increased azithromycin peak concentrations and AUC; no clinically important changes in nelfinavir pharmacokinetics1 |
Dosage adjustment not needed; monitor for azithromycin adverse effects (e.g., hepatic enzyme abnormalities, hearing impairment)1 |
|
Methadone |
Decreased methadone concentrations and AUC1 |
Consider need to increase methadone dosage1 |
|
Nevirapine |
No effect on nelfinavir peak concentrations or AUC1 In vitro evidence of synergistic antiretroviral effects1 |
Appropriate dosages for concomitant use with respect to safety and efficacy not established1 |
|
Pimozide |
Pharmacokinetic interaction; potential for serious or life-threatening reactions (e.g., cardiac arrhythmias)1 |
Concomitant use contraindicated1 |
|
Proton-pump inhibitors |
Omeprazole: Decreased nelfinavir concentrations and AUC1 Proton-pump inhibitors: Possible loss of virologic response and development of resistance1 |
|
|
Quetiapine |
Increased plasma concentrations of quetiapine1 |
Consider alternative antiretroviral therapy in patients already receiving quetiapine1 If concomitant use cannot be avoided, reduce quetiapine dose to 1/6th of current dose and monitor for quetiapine adverse effects.1 Refer to quetiapine prescribing information in patients already receiving nelfinavir being initiated on quetiapine for initial dosing and titration1 |
|
Ritonavir |
Increased nelfinavir concentrations; no change in ritonavir concentrations1 In vitro evidence of additive antiretroviral effects1 |
Appropriate dosages for concomitant use with respect to safety and efficacy not established 1 |
|
Salmeterol |
Increased salmeterol concentrations and increased risk of QT prolongation, palpitations, or sinus tachycardia1 |
Concomitant use not recommended1 |
|
St. John’s wort (Hypericum perforatum) |
Decreased nelfinavir concentrations; possible loss of virologic response and increased risk of resistance to nelfinavir or other antiretrovirals1 |
Concomitant use contraindicated1 |
|
Sildenafil |
Increased sildenafil concentrations and increased risk of sildenafil-associated adverse effects (e.g., hypotension, visual disturbances, prolonged erection, syncope)1 |
Sildenafil (Revatio) for treatment of pulmonary arterial hypertension (PAH): Concomitant use with nelfinavir contraindicated1 Sildenafil for treatment of erectile dysfunction: Do not exceed sildenafil dosage of 25 mg once every 48 hours; use caution and closely monitor for sildenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection, syncope)1 |
|
Tadalafil |
Increased tadalafil concentrations and increased risk of tadalafil-associated adverse effects (e.g., hypotension, visual disturbances, prolonged erection, syncope)1 |
Tadalafil for treatment of PAH: Initiate or adjust tadalafil dosage to 20 mg once daily; based on individual tolerability, may increase tadalafil dosage to 40 mg once daily1 Tadalafil for treatment of erectile dysfunction: Do not exceed tadalafil dosage of 10 mg once every 72 hours; use caution and closely monitor for tadalafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection, syncope)1 |
|
Trazodone |
Possible increased trazodone concentrations1 |
Use with caution; consider using decreased trazodone dosage1 |
|
Vardenafil |
Increased vardenafil concentrations and increased risk of vardenafil-associated adverse effects (e.g., hypotension, visual disturbances, prolonged erection, syncope)1 |
Vardenafil for treatment of erectile dysfunction: Do not exceed vardenafil dosage of 2.5 mg once every 24 hours; use caution and closely monitor for vardenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection, syncope)1 |
|
Warfarin |
Possible altered warfarin concentrations1 |
Carefully monitor INR1 |
|
Zidovudine |
Decreased zidovudine peak concentrations and AUC; no effect on nelfinavir concentrations1 In vitro evidence of synergistic antiretroviral effects1 |
Nelfinavir Mesylate Pharmacokinetics
Absorption
Bioavailability
Nelfinavir 625-mg tablets are not bioequivalent to the 250-mg tablets; AUC 24% higher with the 625-mg tablets (given with food) compared with the 250-mg tablets (given with food).1
Food
Presence of food in the GI tract substantially increases extent of absorption and decreases pharmacokinetic variability of the drug relative to the fasting state.1 Peak plasma concentration and AUC reportedly are 2–5 times greater when administered with a meal (125–1000 kcal with 20–50% fat) rather than under fasting conditions.1
Special Populations
Highly variable plasma concentrations reported in children; may be related to inconsistent food intake.1
Plasma concentrations and AUC in individuals with mild hepatic impairment (Child-Pugh class A) are similar to those in individuals with normal hepatic function.1 In those with moderate hepatic impairment (Child-Pugh class B), peak plasma concentrations and AUC are increased 22 and 62%, respectively.1 Pharmacokinetics not investigated in individuals with severe hepatic impairment.1
Distribution
Extent
Distributed into human milk.1
Plasma Protein Binding
98%.1
Elimination
Metabolism
Metabolized by CYP3A and CYP2C19.1
Elimination Route
Excreted principally in feces as unchanged drug and metabolites.1
Half-life
3.5–5 hours.1
Special Populations
Studies have not shown gender-related differences in pharmacokinetics; further research needed to determine if there are race-related differences.1
Stability
Storage
Oral
Tablets
15–30°C.1
Actions and Spectrum
-
Active against HIV-1 and HIV-2.1 7 8 The major metabolite (M8) has antiviral activity similar to that of nelfinavir.1
-
Inhibits replication of HIV-1 and HIV-2 by interfering with HIV protease.1 2 3 4 7 92 120
-
HIV-1 with reduced susceptibility to nelfinavir have been selected in vitro and have emerged during therapy with the drug.1 7 9
-
Cross-resistance between nelfinavir and nucleoside reverse transcriptase inhibitors (NRTIs) or nonnucleoside reverse transcriptase inhibitors (NNRTIs) unlikely since the drugs have different target enzymes and mechanisms of action.1
Advice to Patients
-
Inform patients of the critical nature of adherence with HIV therapy and importance of remaining under the care of a clinician.1 Advise patients of the importance of taking as prescribed; do not alter or discontinue antiretroviral regimen without consulting clinician.1
-
If a dose is missed, it should be taken as soon as it is remembered and the next dose taken at the regularly scheduled time.1 If a dose is skipped, do not administer a double dose to make up for the missed dose.1
-
Advise patients that redistribution/accumulation of body fat may occur, with unknown long-term health effects.1
-
Inform patients that hyperglycemia, new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus may occur.1 Advise patients to inform their healthcare provider if an increase in thirst or urination develops while receiving nelfinavir.1
-
If using oral contraceptives, advise patients to use an alternative or concomitant nonhormonal contraceptive measures.1
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription (e.g., PDE5 inhibitors) and OTC drugs and dietary or herbal products (e.g., St. John's Wort).1
-
Advise patients to inform clinicians if they are or plan to become pregnant or plan to breast-feed.1 Inform patients that an antiretroviral pregnancy registry is available that monitors fetal outcomes of infants exposed to nelfinavir.1 Providers can register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.1
-
Inform patients of other important precautionary information.1
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
250 mg (of nelfinavir) |
Viracept |
Aguoron Pharmaceuticals |
|
625 mg (of nelfinavir) |
Viracept |
Aguoron Pharmaceuticals |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Aguoron Pharmaceuticals. Nelfinavir mesylate tablets and oral powder. Research Triangle Park, NC; 2021 Mar.
2. Longer M, Shetty B, Zamansky I et al. Preformulation studies of a novel HIV protease inhibitor, AG1343. J Pharm Sci. 1995; 84:1090-3. https://pubmed.ncbi.nlm.nih.gov/8537887
3. Kaldor SW, Kalish VJ, davies JF et al. Viracept (nelfinavir mesylate, AG13430: a potent orally bioavailable inhibitor of HIV-1 protease. J Med Chem. 1997; 40:3979-85. https://pubmed.ncbi.nlm.nih.gov/9397180
4. Moyle G, Gazzard B. Current knowledge and future prospects for the use of HIV protease inhibitors. Drugs. 1996; 51:701-12. https://pubmed.ncbi.nlm.nih.gov/8861542
5. Vella S. Rationale and experience with reverse transcriptase inhibitors and protease inhibitors. J Acquir Immune Defic Syndr Hum Retrovirol. 1995; 10(Suppl 1):S58-61.
7. Patick AK, Mo H, Markowitz M et al. Antiviral and resistance studies of AG1343, an orally bioavailable inhibitor of human immunodeficiency virus protease. Antimicrob Agents Chemother. 1996; 40:292-7. https://pubmed.ncbi.nlm.nih.gov/8834868
8. Shetty BV, Kosa MB, Khalil DA et al. Preclinical pharmacokinetics and distribution to tissue of AG1343, an inhibitor of human immunodeficiency virus type 1 protease. Antimicrob Agents Chemother. 1996; 40:110-4. https://pubmed.ncbi.nlm.nih.gov/8787890
9. Patick AK, Duran M, Cao Y et al. Genotypic and phenotypic characterization of human immunodeficiency virus type 1 variants isolated from patients treated with the protease inhibitor nelfinavir. Antimicrob Agents Chemother. 1998; 42:2637-44. https://pubmed.ncbi.nlm.nih.gov/9756769
10. Lech WJ, Wang G, Yang YL et al. In vivo sequence diversity of the protease of human immunodeficiency virus type 1: presence of protease inhibitor-resistant variants in untreated subjects. J Virol. 1996; 70:2038-43. https://pubmed.ncbi.nlm.nih.gov/8627733
11. Ridky T, Leis J. Development of drug resistance to HIV-1 protease inhibitors. J Biol Chem. 1995; 270:29621-3. https://pubmed.ncbi.nlm.nih.gov/8530341
13. Deeks SG, Smith M, Holodniy M et al. HIV-1 protease inhibitors: a review for clinicians. JAMA. 1997; 277:145-53. https://pubmed.ncbi.nlm.nih.gov/8990341
14. Izzedine H, Diquet B, Launay-Vacher V et al. Pharmacokinetics of nelfinavir in an HIV patient with renal insufficiency. AIDS. 1999; 13:1989. https://pubmed.ncbi.nlm.nih.gov/10513666
16. Moyle GJ. Resistance to antiretroviral compounds: implications for the clinical management of HIV infection. Immunol Infect Dis. 1995; 5:170-82.
17. Pollard RB. Use of proteinase inhibitors in clinical practice. Pharmacotherapy. 1994; 14:21-9S.
92. Gehlhaar DK, Verkhivker GM, Rejto PA et al. Molecular recognition of the inhibitor AG-1343 by HIV-1 protease: conformationally flexible docking by evolutionary programming. Chem Biol. 1995; 2:317-24. https://pubmed.ncbi.nlm.nih.gov/9383433
120. FDA summary basis of approval on nelfinavir. Rockville, MD; 1997.
121. Saag MS, Tebas P, Sension M et al. Randomized, double-blind comparison of two nelfinavir doses plus nucleosides in HIV-infected patients (Agouron study 511). AIDS. 2001; 15:1971-8. https://pubmed.ncbi.nlm.nih.gov/11600825
125. Patick AK, Boritzki TJ, Bloom LA. Activities of the human immunodeficiency virus type 1 (HIV-1) protease inhibitor nelfinavir mesylate in combination with reverse transcriptase and protease inhibitors against acute HIV-1 infection in vitro. Antimicrob Agents Chemother. 1997; 41:2159-64. https://pubmed.ncbi.nlm.nih.gov/9333041
126. Aboulker JP, Babiker A, Chaix ML et al. Highly active antiretroviral therapy started in infants under 3 months of age: 72-week follow-up for CD4 cell count, viral load and drug resistance outcome. AIDS. 2004; 18:237-45. https://pubmed.ncbi.nlm.nih.gov/15075541
127. Krogstad P, Wiznia A, Luzuriaga K et al. Treatment of human immunodeficiency virus 1-infected infants and children with the protease inhibitor nelfinavir mesylate. Clin Infect Dis. 1999; 28:1109-18. https://pubmed.ncbi.nlm.nih.gov/10452644
156. Wiznia A, Stanley K, Korgstad P et al. Combination nucleoside analog reverse trancriptase inhibitor(s) plus nevirapine, nelfinavir, or ritonavir in stable antiretroviral therapy-experienced HIV-infected children: week 24 results of a randomized controlled trial—PACTG 377. AIDS Res Hum Retroviruses. 2000; 16:1113-21. https://pubmed.ncbi.nlm.nih.gov/10954886
200. Panel on Antiretroviral Guidelines for Adults and Adolescents, US Department of Health and Human Services (HHS). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (February 27, 2024). Updates may be available at HIV.gov website. https://clinicalinfo.hiv.gov/en/guidelines
201. Panel on Antiretroviral Therapy and Medical Management of HIV-infected Children, US Department of Health and Human Services (HHS). Guidelines for the use of antiretroviral agents in pediatric HIV infection (January 31, 2023). Updates may be available at HIV.gov website. https://clinicalinfo.hiv.gov/en/guidelines
202. Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, US Department of Health and Human Services (HHS). Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States (January 31, 2024). Updates may be available at HIV.gov website. https://clinicalinfo.hiv.gov/en/guidelines
500. Gartland M, AVANTI Study Group. AVANTI 3: a randomized, double-blind trial to compare the efficacy and safety of lamivudine plus zidovudine versus lamivudine plus zidovudine plus nelfinavir in HIV-1-infected antiretroviral-naïve patients. Antivir Ther. 2001;6(2):127-134.
501. Albrecht M, Bosch R, Hammer S, et al. Nelfinavir, efavirenz, or both after the failure of nucleoside treatment of HIV infection. N Engl J Med. 2001;345(6):398-407.
502. Paediatric European Network for Treatment of AIDS (PENTA). Highly active antiretroviral therapy started in infants under 3 months of age: 72-week follow-up for CD4 cell count, viral load and drug resistance outcome. AIDS. 2004;18:237-245.
503. Institute for Safe Medication Practices. ISMP list of error-prone abbreviations, symbols, and dose designations. 2024.
Related/similar drugs
Frequently asked questions
More about nelfinavir
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
- Breastfeeding
- En español