Molindone (Monograph)
Drug class: Dihydroindolones
Introduction
Molindone hydrochloride is a dihydroindolone-derivative antipsychotic agent. The drug is considered a conventional or first-generation antipsychotic agent.
Uses for Molindone
Psychotic Disorders
Molindone is used in the symptomatic management of schizophrenic disorder. Drug therapy is integral to the management of acute psychotic episodes in patients with schizophrenia and generally is required for long-term stabilization to improve symptoms between episodes and to minimize the risk of recurrent acute episodes. Antipsychotic agents are the principal class of drugs used for the management of all phases of schizophrenia and generally are effective in all subtypes of the disorder and subgroups of patients. Patient response and tolerance to antipsychotic agents are variable, and patients who do not respond to or tolerate one drug may be successfully treated with an agent from a different class or with a different adverse effect profile.
Molindone has been effective in patients with chronic schizophrenia and in those with acute schizophrenic reactions. The drug may control symptoms of schizophrenia such as disorientation, conceptual disorganization, perceptual distortion, hallucinations, grandiosity, emotional withdrawal, and tension. Somatic concern, anxiety, guilt feelings, and depression usually show less improvement. During molindone therapy, hospitalized patients have also shown improvement in social competence and social interest. Although results of some studies indicate that the effectiveness of molindone is about equal to that of the phenothiazines, results in other clinical trials have been variable and in some instances negative (possibly because of inadequate molindone dosage). Molindone is sometimes effective in treating patients with long-term, chronic schizophrenia who have not responded to other drugs.
Molindone Dosage and Administration
Administration
Molindone hydrochloride is administered orally.
Dosage
Dosage of molindone hydrochloride must be carefully adjusted according to individual requirements and response using the lowest possible effective dosage. Geriatric and debilitated patients should be started on low dosages.
Psychotic Disorders
In the management of schizophrenia, the usual initial adult dosage of molindone hydrochloride is 50–75 mg daily, given in 3 or 4 divided doses. Dosage may be increased to 100 mg daily after 3 or 4 days of therapy. In patients with severe symptomatology, dosages of molindone hydrochloride up to 225 mg daily may be required initially.
The usual adult maintenance dosage of molindone hydrochloride when symptoms of schizophrenia are mild is 5–15 mg 3 or 4 times a day. When the symptoms of schizophrenia are moderately severe, the usual adult maintenance dosage is 10–25 mg 3 or 4 times daily. When schizophrenic symptoms are severe, maintenance dosages up to 225 mg of molindone hydrochloride daily may be necessary; however, some clinicians have found that dosages greater than 150 mg daily rarely produce additional therapeutic benefits. For maintenance therapy, a single daily dose of the drug is often adequate. Weeks or months of treatment at optimum dosage levels may be necessary to produce maximum clinical improvement in patients with resistant mental and emotional disturbances.
Cautions for Molindone
Although molindone differs chemically from the phenothiazines, the drug may be capable of producing many of the toxic manifestations of phenothiazine derivatives. While all adverse reactions of the phenothiazines have not been reported with molindone, the possibility that they may occur should be considered. Adverse effects of molindone and the phenothiazines are numerous and may involve nearly all organ systems; however, they usually are reversible when dosage is reduced or the drug is discontinued. Some adverse effects may be attributed to the actions of the drug on the central and autonomic nervous systems, whereas others are hypersensitivity reactions. Unexpected deaths have been reported during phenothiazine therapy. In some patients, cardiac arrest or asphyxia resulting from failure of the cough reflex appeared to be the cause of death. In other cases, the cause of death could not be determined or definitely attributed to phenothiazine therapy.
Nervous System Effects
The most frequent adverse effect of molindone is transient initial drowsiness.
Extrapyramidal Reactions
Extrapyramidal syndromes such as akathisia or a parkinsonian-like condition manifested by akinesia (characterized by rigidity, immobility, and reduction of voluntary movements and tremor) occur frequently. Extrapyramidal symptoms usually are dose-related and can be controlled with dosage reduction and/or administering an anticholinergic antiparkinsonian drug. Patients who have experienced extrapyramidal syndromes in association with other antipsychotic drugs will probably react similarly to molindone.
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome (NMS) may occur in patients receiving molindone or other antipsychotic therapy. NMS is potentially fatal and requires immediate discontinuance of the drug and intensive symptomatic and supportive care.
Tardive Dyskinesia
Persistent tardive dyskinesia may occur in patients receiving long-term therapy with antipsychotic drugs, or may appear after drug therapy has been discontinued. The possibility that long-term therapy with molindone may cause this effect should be considered. The risk of persistent tardive dyskinesia appears to be greater in geriatric patients (particularly females) receiving high-dose therapy.
Management of tardive dyskinesia generally consists of gradual discontinuance of the precipitating antipsychotic agent when possible, reducing the dosage of the first-generation (conventional) antipsychotic agent or switching to a second-generation (atypical) antipsychotic agent, or switching to clozapine therapy. Vesicular monoamine transporter 2 (VMAT2) inhibitors (e.g., deutetrabenazine, valbenazine tosylate) have been effective in reducing symptoms of tardive dyskinesia in controlled clinical studies. Anticholinergic antiparkinsonian drugs usually do not relieve the symptoms of this syndrome and may aggravate the condition. It has been suggested that an early sign of the syndrome may be fine vermicular movements of the tongue and that if the drug is discontinued as soon as this occurs, the syndrome may not develop.
Other Nervous System Effects
Adverse effects attributed to the action of molindone on the autonomic nervous system include dryness of the mouth, constipation, blurred vision, and nasal congestion. Insomnia, mental depression, suicidal tendencies, euphoria, headache, feeling of weakness, and dizziness also may occur. Infrequent neuromuscular symptoms which may occur following administration of molindone include oculogyric crisis, spasticity, dystonias, restlessness, and hyperactivity.
Hematologic Effects
Transitory fluctuations in leukocyte counts, leukopenia, and eosinophilia without clinical manifestations have been observed occasionally. Since blood disorders (including agranulocytosis, hemolytic anemia, thrombocytopenia, and pancytopenia) have been reported in patients receiving other antipsychotic agents, the possibility that such adverse effects may occur in patients receiving molindone should be considered.
Endocrine, Genitourinary, and Metabolic Effects
Moderate engorgement of the breast with lactation has occurred infrequently in female patients receiving molindone. Other reported endocrine disorders include menstrual irregularities (heavy menses, amenorrhea, or dysmenorrhea) and increased libido. Premature ejaculation, gynecomastia, false-positive pregnancy test results, hypoglycemia, hyperglycemia, or glycosuria has been associated with phenothiazine therapy. At least one case of priapism, which required surgical intervention resulting in apparent residual impairment of erectile function, has been reported with molindone therapy. Molindone has produced increases in plasma free fatty acid concentrations 2 hours after administration of the drug in healthy individuals. Weight gain or loss has been reported in a few patients receiving molindone. It should be considered that phenothiazine therapy has been associated with peripheral edema.
Hepatic Effects
Since cholestatic jaundice has been reported in patients receiving other antipsychotic agents, the possibility that such an adverse effect may occur in patients receiving molindone should be considered. Elevated SGOT (AST), SGPT (ALT), and serum alkaline phosphatase concentrations without clinical manifestations have been observed occasionally.
Cardiovascular Effects
Tachycardia and postural hypotension have occurred in a few patients. Nonspecific ECG changes, which were not associated with clinical manifestations and which disappeared when the drug was discontinued, have been observed in some patients receiving molindone. Severe orthostatic hypotension has not been reported to date with molindone, but the possibility of its occurrence should be considered.
GI Effects
Anorexia, nausea, or GI upset may occur with molindone therapy.
Other Adverse Effects
Skin pigmentation and ocular changes have occurred in some patients receiving long-term therapy with some phenothiazines. Although these adverse effects have not been reported to date in patients receiving molindone, patients receiving the drug should be carefully observed for pigmentary changes and periodic ophthalmologic examinations (including slit-lamp examinations) should be performed in patients receiving prolonged molindone therapy. Other adverse effects that have occurred in a few patients receiving molindone include skin rash and tinnitus.
Phenothiazine therapy also has been associated with peripheral edema, cerebral edema, and a syndrome resembling systemic lupus erythematosus.
Precautions and Contraindications
Molindone shares the toxic potentials of other antipsychotic agents (e.g., phenothiazines), and the usual precautions associated with therapy with these agents should be observed.
Geriatric patients with dementia-related psychosis treated with either conventional (first-generation) or atypical (second-generation) antipsychotic agents are at an increased risk of mortality.
Since drowsiness may occur, particularly when molindone therapy is initiated, patients should be cautioned that the drug may impair their ability to perform hazardous activities requiring mental alertness or physical coordination such as operating machinery or driving a motor vehicle. Since increased activity has been observed in some patients during molindone therapy, the drug should be administered with caution to those patients in whom increased activity might be harmful. Although molindone has not lowered the seizure threshold in animals to the same extent as some other antipsychotic agents, the manufacturer cautions that seizures have reportedly occurred in a few patients receiving molindone. Since molindone has an antiemetic effect in animals and may have a similar effect in humans, it is possible that the drug could mask the signs of overdosage of toxic agents or interfere with the diagnosis of such conditions as intestinal obstruction or brain tumor.
Molindone is contraindicated in comatose patients and in patients who have severe CNS depression from any cause or known hypersensitivity to the drug.
Pediatric Precautions
Pending further accumulation of clinical data to establish safety and efficacy in children, molindone is not recommended for use in children younger than 12 years of age.
Mutagenicity and Carcinogenicity
Although an increase in mammary neoplasms has been found in rodents following long-term administration of prolactin-stimulating antipsychotic agents, no clinical or epidemiologic studies conducted to date have shown an association between long-term administration of these drugs and mammary tumorigenesis in humans. Current evidence is considered too limited to be conclusive, and further study is needed to determine the clinical importance in most patients of elevated serum prolactin concentrations associated with antipsychotic agents. Since in vitro tests indicate that approximately one-third of human breast cancers are prolactin dependent, molindone should be used with caution in patients with previously detected breast cancer.
Pregnancy and Lactation
Pregnancy
Neonates exposed to antipsychotic agents during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery. The symptoms reported in these neonates have included agitation, hypertonia, hypotonia, tardive dyskinetic-like symptoms, tremor, somnolence, respiratory distress, and feeding disorder; neonates exhibiting such symptoms should be monitored. The reactions were self-limiting in some neonates but varied in severity; some infants required intensive support and prolonged hospitalization.
Safe use of molindone during pregnancy has not been established. The drug should be used during pregnancy only if the potential benefits outweigh the potential risks to the woman and fetus.
Lactation
Safe use of molindone in lactating women has not been established. The drug should not be used in nursing women unless the potential benefits outweigh the possible risk to the woman or nursing infant.
Drug Interactions
Because molindone hydrochloride tablets contain calcium sulfate as an excipient, calcium ions could potentially decrease the absorption of concomitantly administered phenytoin or tetracyclines.
Acute Toxicity
Limited information is available on the acute toxicity of molindone. Overdosage of molindone presumably may be manifested by severe extrapyramidal reactions and sedation. Coma with respiratory depression and severe hypotension resulting in a shock-like syndrome could occur. In the treatment of overdosage, symptomatic supportive therapy is indicated and general physiologic measures such as maintenance of adequate airway, oxygen uptake, and carbon dioxide removal should be maintained. Early gastric lavage may be done if an endotracheal tube with cuff inflated is in place to prevent aspiration of gastric contents. Anticholinergic antiparkinsonian agents may be used to treat severe extrapyramidal reactions. It is unlikely that forced diuresis, peritoneal dialysis, or hemodialysis would be effective in the management of acute intoxication with molindone.
Pharmacology
Molindone produces pharmacologic responses similar to those of the phenothiazines, butyrophenones, and thioxanthenes. Although the precise mechanism of action is not known, some investigators have postulated that molindone acts primarily on the ascending reticular activating system. In animals, molindone suppresses locomotor activity, conditioned avoidance behavior, and amphetamine-induced stereotypy. In rodents, the drug shows antidepressant properties, i.e., it antagonizes tetrabenazine-induced ptosis and potentiates the stimulatory effects of dihydroxyphenylalanine and 5-hydroxytryptophan without monoamine oxidase inhibition. Although antiemetic activity in humans has not been clinically evaluated, the drug appears to have potent antiemetic effects in dogs. Molindone has also shown some anti-nociceptive effects in rodents. In humans, molindone produces marked changes in resting and sleep EEG recordings. In one study, the drug significantly decreased the duration of deep sleep. There appears to be a very narrow range between the effective therapeutic dose and doses causing extrapyramidal symptoms.
Molindone Pharmacokinetics
Absorption
Molindone is rapidly absorbed from the GI tract. Peak blood concentrations of unmetabolized drug occur within approximately 1.5 hours. Plasma concentrations of the drug necessary to produce antipsychotic effects are unknown. Following a 30-mg oral dose, molindone plasma concentrations of 2 ng/mL have been detected. The duration of action from a single oral dose of molindone may persist for 24–36 hours. This long duration of action, relative to the drug’s short plasma half-life, may be due to active metabolites that possess antipsychotic activity.
Distribution
Studies in monkeys indicate that the drug is widely distributed into body tissues. Approximately 76% of molindone is bound to plasma proteins. No data are available on the distribution of molindone in humans, but the drug probably enters the CSF and may distribute into the milk of nursing women. It is not known whether the drug crosses the placenta.
Elimination
The elimination half-life of molindone is reported to be approximately 2 hours. Molindone is rapidly metabolized, probably by the liver; 36 inactive metabolites have been identified in urine and feces. Less than 2–3% of the drug is excreted unchanged. More than 90% of a single dose of molindone is excreted in feces and urine within 24 hours. A small amount is excreted via the lungs as carbon dioxide.
Chemistry and Stability
Chemistry
Molindone hydrochloride is a dihydroindolone-derivative antipsychotic agent. The drug is structurally related to naturally occurring psychotropics such as serotonin, bufotenine, and psilocin. Molindone hydrochloride occurs as a white to off white, crystalline powder and is freely soluble in water and in alcohol. Molindone is a weak base with a pKa of 6.94.
Stability
Commercially available molindone hydrochloride tablets should be stored at 20–25°C and protected from light.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
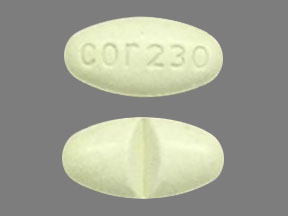
Oral |
Tablets |
5 mg |
Molindone Hydrochloride Tablets |
CorePharma |
|
10 mg |
Molindone Hydrochloride Tablets |
CorePharma |
||
|
25 mg |
Molindone Hydrochloride Tablets (scored) |
CorePharma |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about molindone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antipsychotic agents
- Breastfeeding
- En español