Leucovorin (Monograph)
Brand name: Wellcovorin
Drug class: Chemotherapy antidotes/protectants
Introduction
Folic acid derivative; antidote for folic acid antagonists.b c
Uses for Leucovorin
Toxicity Associated with Folic Acid Antagonists
Antidote for unintentional overdosage of methotrexate (e.g., resulting from impaired elimination) and other folic acid antagonists (e.g., pyrimethamine, trimethoprim).b c
IV rescue therapy after high-dose methotrexate regimen (to control duration of exposure of sensitive cells to methotrexate) in the treatment of osteosarcomaa c (designated an orphan drug by FDA for this use).d
Prevention of hematologic toxicity† [off-label] associated with pyrimethamine, trimethoprim, or trimetrexate therapy.160 a
Megaloblastic Anemia
IV treatment of folate deficient megaloblastic anemias (e.g., serum folate concentration <0.002 mcg/mL) of infancy, pregnancy, sprue, and nutritional deficiencies when oral folic acid therapy is not feasible.a c No advantage over folic acid injection since ability to convert folic acid to tetrahydrofolic acid (THF) is not impaired in these anemias.a
Effective in the treatment of megaloblastic anemia resulting from congenital dihydrofolate reductase deficiency† [off-label] .a
Not effective in the treatment of pernicious anemia and other megaloblastic anemias secondary to lack of vitamin B12; avoid such use.101 102 106 (See Contraindications under Cautions.)
Colorectal Cancer
Adjunct to fluorouracil to prolong survival in the palliative treatment of advanced colorectal cancer102 108 112 114 116 118 124 125 126 127 128 129 131 140 146 153 154 155 (designated an orphan drug by FDA for this use).164
First-line therapy for management of advanced colorectal cancer in a combination regimen consisting of fluorouracil, leucovorin, and either irinotecan or oxaliplatin.e f
Leucovorin Dosage and Administration
General
Toxicity Associated with Folic Acid Antagonists
- Methotrexate Overdosage or Rescue after High-dose Methotrexate Therapy
-
Monitoring of serum methotrexate concentration required to determine optimum dose and duration of leucovorin therapy.b c
-
Maintain adequate hydration (3 L daily) and administer sodium bicarbonate to maintain urinary pH at ≥7 during therapy.b c
-
Monitor fluid and electrolyte status in patients experiencing delayed early methotrexate elimination and nonoliguric renal failure until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM) and renal failure has resolved.b c
- Prevention of Pyrimethamine Toxicity† [off-label]
-
Dosage of leucovorin necessary to prevent hematologic toxicity varies depending on the dosage of the folic acid antagonist and patient’s clinical status.159
- Prevention of Trimetrexate Toxicity† [off-label]
-
Monitoring of neutrophil counts and platelet counts required; modify dosage of trimetrexate and leucovorin based on the worst of the two blood cell counts.160 (See Table 4.)
Administration
Administer orally or by IV or IM injection.b c
Administer parenterally rather than orally in patients with GI toxicity (e.g., nausea, vomiting) and in those receiving individual doses >25 mg.101 b c Parenteral administration also preferred if possibility of vomiting and/or decreased GI absorption exists.b c
Do not administer intrathecally (potentially harmful or fatal).102 b c
Oral Administration
Saturable absorption; administration of doses >25 mg not recommended.b (See Absorption under Pharmacokinetics.)
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
If used concomitantly with fluorouracil, administer separately to avoid possible formation of a precipitate.c However, no visually apparent precipitate was detected when the drugs were injected sequentially (with no flush between) into Y-site.HID (See Compatibility under Stability.)
Reconstitution
Add 5, 10, or 20 mL of sterile water for injection or bacteriostatic water for injection (benzyl alcohol-preserved) to vial containing 50, 100, or 200 mg of leucovorin, respectively, to provide a solution containing 10 mg/mL.c
For vial containing 350 mg of leucovorin, reconstitute with 17.5 mL of sterile water for injection or bacteriostatic water for injection to provide a solution containing 20 mg/mL.c
Due to benzyl alcohol content in bacteriostatic water for injection, reconstitute with sterile water for injection when preparing doses >10 mg/m2.102 106 c
Rate of Administration
Due to calcium content, administer no more than 160 mg per minute (16 mL of a 10-mg/mL solution or 8 mL of a 20-mg/mL solution per minute).102 106 c
For prevention of trimetrexate toxicity† [off-label], administer dose over 5–10 minutes.160
Dosage
Available as leucovorin calcium; dosage expressed in terms of leucovorin.b c
Pediatric Patients
Toxicity Associated with Folic Acid Antagonists
Prevention of Pyrimethamine Toxicity†
OralFor pyrimethamine dosages of 25–100 mg daily or 1–2 mg/kg daily (for treatment of toxoplasmosis): 10–25 mg administered with each pyrimethamine dose.161
For pyrimethamine dosages of 25–50 mg once daily (given with clindamycin or sulfadiazine for secondary prophylaxis of toxoplasmosis in adolescents): 10–25 mg once daily.105
For pyrimethamine dosage of 1 mg/kg once daily (given with dapsone or clindamycin for primary or secondary prophylaxis of toxoplasmosis, respectively, in HIV-infected children): 5 mg once every 3 days.105
For pyrimethamine dosage of 25 mg once daily (given with atovaquone for primary or secondary prophylaxis against toxoplasmosis in HIV-infected adolescents): 10 mg daily, administered concomitantly with pyrimethamine.105
For pyrimethamine dosage of 50 or 75 mg once weekly (given with dapsone for primary prevention of Pneumocystis jiroveci [formerly Pneumocystis carinii] pneumonia or toxoplasmosis or for secondary prophylaxis of P. jiroveci pneumonia in HIV-infected adolescents): 25 mg once weekly, administered concomitantly with pyrimethamine.105 161
Adults
Toxicity Associated with Folic Acid Antagonists
Methotrexate Overdosage
Dosage is approximately twice that of levoleucovorin (the active l-isomer).162
Oral, IV, or IM15 mg (approximately 10 mg/m2) every 6 hours until serum methotrexate concentration declines to <0.005 mcg/mL (0.01 μM); initiate administration as soon as possible after overdosage and within 24 hours following methotrexate administration if delayed elimination is detected.b c (See Table 1 and Table 2 under Dosage and Administration.)
If 24-hour Scr increases 50% over baseline, 24-hour methotrexate concentration is >2.27 mcg/mL (5 μM, or 48-hour methotrexate concentration is >0.409 mcg/mL (0.9 μM), increase dosage immediately to 150 mg (approximately 100 mg/m2) IV every 3 hours until serum methotrexate concentration declines to <0.005 mcg/mL (0.01 μM).b c
Pyrimethamine or Trimethoprim Overdosage
Oral5–15 mg daily is recommended by some clinicians.b
Rescue after High-dose Methotrexate Therapy
Dosage is approximately twice that of levoleucovorin (the active l-isomer).162
Oral, IV, or IM15 mg (approximately 10 mg/m2) every 6 hours for 10 doses, starting at 24 hours after initiation of methotrexate (12–15 g/m2) infusion for patients with normal methotrexate elimination (i.e., serum methotrexate concentration approximately 4.54 mcg/mL [10 μM] at 24 hours after administration, 0.454 mcg/mL [1 μM] at 48 hours, and <0.091 mcg/mL [0.2 μM] at 72 hours).c
Continue therapy and maintain adequate hydration and urinary alkalization (pH ≥7) until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM).c
If substantial clinical toxicity occurs in patients with mild abnormalities in methotrexate elimination or renal function, extend rescue therapy for an additional 24 hours (i.e., 14 doses over 84 hours) for subsequent methotrexate courses.b c
Monitor Scr and methotrexate concentration at least once daily.c Adjust dosage and duration of therapy based on methotrexate elimination pattern and patient’s renal function.c (See Tables 1 and 2.)
|
Serum Methotrexate Concentration |
Leucovorin Dosage Adjustment |
|---|---|
|
>0.091 mcg/mL (0.2 μM) at 72 hours and >0.023 mcg/mL (0.05 μM) at 96 hours following methotrexate administration |
Continue leucovorin 15 mg every 6 hours until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM)b c |
|
Serum Methotrexate and/or Scr Concentration |
Leucovorin Dosage Adjustment and Monitoring |
|---|---|
|
≥22.7 mcg/mL (50 μM) at 24 hours or ≥2.27 mcg/mL (5 μM) at 48 hours after methotrexate administration and/or ≥100% increase in Scr at 24 hours after administration |
Leucovorin 150 mg IV every 3 hours until methotrexate concentration declines to <0.454 mcg/mL (1 μM), then leucovorin 15 mg IV every 3 hours until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM)b c If nonoliguric renal failure develops, monitor fluid and electrolyte status until methotrexate concentration declines to 0.023 mcg/mL (0.05 μM) and renal failure has resolvedb c |
Prevention of Pyrimethamine Toxicity†
OralFor pyrimethamine dosages of 25–100 mg daily or 1–2 mg/kg daily (for treatment of toxoplasmosis): 10–25 mg administered with each pyrimethamine dose.161
For pyrimethamine dosages of 25–50 mg once daily (given with clindamycin or sulfadiazine for secondary prophylaxis of toxoplasmosis): 10–25 mg once daily.105
For pyrimethamine dosage of 25 mg once daily (given with atovaquone for primary or secondary prophylaxis of toxoplasmosis in HIV-infected individuals): 10 mg daily, administered concomitantly with pyrimethamine.105
For pyrimethamine dosage of 50 or 75 mg once weekly (given with dapsone for primary prevention of P. jiroveci pneumonia or toxoplasmosis or for secondary prophylaxis of P. jiroveci pneumonia in HIV-infected individuals): 25 mg once weekly, administered concomitantly with pyrimethamine.105 161
Prevention of Trimetrexate Toxicity†
Oral or IVFor trimetrexate dose of 45 mg/m2: 20 mg/m2 every 6 hours (total daily dose: 80 mg/m2).160 161
Alternatively, dose may be based on body weight.160 (See Table 3.)
|
Body Weight (kg) |
Trimetrexate Dosage (mg/kg/day) |
Leucovorin Dosage (mg/kg Every 6 Hours) |
|---|---|---|
|
<50 |
1.5 |
0.6 |
|
50–80 |
1.2 |
0.5 |
|
>80 |
1.0 |
0.5 |
Round calculated oral dose up to the next 25-mg increment.160
Continue leucovorin therapy for at least 72 hours after last trimetrexate dose (usual duration: 24 days).160
Adjust dosage if hematologic toxicities occur, based on the worst of the two blood cell counts.160 (See Table 4.)
Adjust dosage based on the worse of the two blood counts
|
Toxicity Grade |
ANC (cells/mm3) |
Platelets (cells/mm3) |
Dosage Adjustments |
|---|---|---|---|
|
1 |
>1000 |
>75,000 |
No adjustment in trimetrexate or leucovorin dosages |
|
2 |
750–1000 |
50,000–75,000 |
No adjustment in trimetrexate dosage; increase leucovorin to 40 mg/m2 every 6 hours |
|
3 |
500–749 |
25,000–49,999 |
Decrease trimetrexate dose to 22 mg/m2 once daily; increase leucovorin to 40 mg/m2 every 6 hours |
|
4 |
<500 |
<25,000 |
Day 1–9: Discontinue trimetrexate; increase leucovorin to 40 mg/m2 every 6 hours for an additional 72 hours Day 10–21: Discontinue trimetrexate; increase leucovorin to 40 mg/m2 every 6 hours for an additional 72 hours. If hematologic toxicity improves within 96 hours to grade 3 or grade 2, reinitiate trimetrexate at 22 mg/m2 or 45 mg/m2, respectively, once daily; continue leucovorin for 72 hours after the last trimetrexate dose |
Megaloblastic Anemia
IM
Up to 1 mg daily; no evidence that doses >1 mg daily are more effective.a c
Duration of therapy depends on hematologic response.a In general, improved sense of well-being occurs within first 24 hours; bone marrow begins to become normoblastic within 48 hours; and reticulocytosis begins within 2–5 days after initiation of therapy.a
Colorectal Cancer
IV
Leucovorin 20 mg/m2 followed by IV fluorouracil (425 mg/m2) daily for 5 days102 126 130 131 132 144 c or leucovorin 200 mg/m2 by slow IV injection (over a minimum of 3 minutes) followed by IV fluorouracil (370 mg/m2) daily for 5 days;102 116 126 130 131 132 144 156 c no evidence of superiority of either regimen.131
Repeat either regimen at 4-week intervals for 2 additional courses, then at 4- to 5-week intervals provided toxicity from the previous course has subsided.102 126 c
Do not administer repeat courses until WBC >4000/mm3 and platelet count >130,000/mm3.c If blood counts do not return to these levels within 2 weeks, discontinue therapy.102 c Discontinue therapy when there is clear evidence of tumor progression.102 c (See Patient Evaluation and Monitoring under Cautions.)
If WBC and platelet count return to >4000/mm3 and >130,000/mm3, respectively, within 2 weeks, adjust subsequent fluorouracil dosages based on severity of GI toxicity and nadir blood counts from previous course; leucovorin dosage generally not adjusted according to toxicity.102 c (See Table 5.) If no toxicity occurred in the prior course, increase subsequent fluorouracil dosage by 10%.102 c
Adjust dosage based on the most severe toxicity.
|
Toxicity after Prior Dose |
Fluorouracil Daily Dosage for Subsequent Course |
|---|---|
|
If moderate diarrhea and/or stomatitis or WBC nadir of 1000–1900/mm3 or Platelet nadir of 25,000–75,000/mm3 occurs |
Reduce dosage by 20% |
|
If severe diarrhea and/or stomatitis or WBC nadir of <1000/mm3 or Platelet nadir of <25,000/mm3 occurs |
Reduce dosage by 30% |
Prescribing Limits
Pediatric Patients
Oral
Administration of doses >25 mg not recommended.b (See Absorption under Pharmacokinetics.)
Adults
Oral
Administration of doses >25 mg not recommended.b (See Absorption under Pharmacokinetics.)
Special Populations
Patients with Delayed Methotrexate Elimination
Higher dosages and extended duration of therapy may be required if delayed methotrexate excretion is caused by third space fluid accumulation (i.e., ascites, pleural effusion), renal impairment, or inadequate hydration.b c
Cautions for Leucovorin
Contraindications
-
Pernicious anemia or other megaloblastic anemias secondary to lack of vitamin B12;101 102 106 such use may obscure diagnosis of pernicious anemia by alleviating hematologic manifestations while allowing neurologic complications to progress.a b c
Warnings/Precautions
Warnings
Use as Antidote
Administer as soon as possible following unintentional overdosage.b c Delayed administration may reduce effectiveness in counteracting hematologic toxicity associated with folic acid antagonists.b c
Toxicity Potentiation with Concomitant Therapy
When used concomitantly with other chemotherapeutic agents (e.g., fluorouracil, methotrexate), administer only under the supervision of a qualified clinician experienced in the use of cancer chemotherapeutic agents.a c
Possible potentiation of fluorouracil toxicity.c GI toxicities (particularly stomatitis and diarrhea) observed more frequently, and possibly more severe and prolonged, compared with fluorouracil monotherapy.c Diarrhea may result in clinical deterioration, leading to death;102 143 155 c if diarrhea occurs, monitor patients until manifestations have completely resolved.c Do not initiate or continue combination therapy in patients with manifestations of GI toxicity until such manifestations have completely resolved.102 114 126 c Increased risk of severe GI toxicity in debilitated or geriatric patients; use with extreme caution.102 143 c (See Geriatric Use under Cautions.)
Concomitant use with co-trimoxazole for treatment of P. jiroveci pneumonia in HIV-infected patients associated with increased rates of treatment failure, morbidity, and mortality.b c
Seizures and/or syncope reported rarely, usually following concomitant therapy with fluoropyrimidines; most commonly reported in cancer patients with CNS metastases or other predisposing factors.c
Sensitivity Reactions
Anaphylactoid Reactions
Anaphylactoid reactions and urticaria reported.b c
General Precautions
Patient Evaluation and Monitoring
Treatment of advanced colorectal cancer: When used in combination with fluorouracil, perform physical examination prior to each treatment course and appropriate radiological examination as needed; discontinue therapy when there is clear evidence of tumor progression.102 c Monitor CBC (with differential) and platelet count prior to initiation of therapy.c During first 2 courses, monitor CBC (with differential) and platelet count weekly; thereafter, monitor once each cycle at time of anticipated WBC nadir.102 c Monitor electrolytes and liver function tests prior to each course for the first 3 courses, then prior to every other course.c
Specific Populations
Pregnancy
Lactation
Not known whether distributed into milk.b c Use with caution.b c
Pediatric Use
Possible decreased anticonvulsant effect in pediatric patients receiving anticonvulsant therapy concomitantly with large amounts of folic acid; possible increased frequency of seizures in susceptible patients.b c (See Interactions.)
Geriatric Use
Treatment of advanced colorectal cancer: Increased risk of severe GI toxicity when used in combination with fluorouracil.c Death secondary to severe enterocolitis, diarrhea, and dehydration reported in geriatric patients receiving weekly leucovorin and fluorouracil therapy;102 143 c concomitant granulocytopenia and fever observed in some patients.c Use with extreme caution.102 143 c
Common Adverse Effects
Leucovorin in combination with fluorouracil: leukopenia, nausea, vomiting, diarrhea, stomatitis, lethargy/malaise/fatigue, alopecia, dermatitis, anorexia.c
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticonvulsants (phenobarbital, phenytoin, primidone) |
Decreased anticonvulsant effect if used concomitantly with large amounts of folic acid; possible increased frequency of seizures in susceptible pediatric patientsb c |
Use concomitantly with caution167 |
|
Co-trimoxazole |
Increased rates of treatment failure, morbidity, and mortality in HIV-infected patients receiving combination therapy for treatment of P. jiroveci pneumoniac |
|
|
Glucarpidase |
Administration of glucarpidase 2 hours before racemic leucovorin reduces peak concentrations and exposure of leucovorin and 5-methyl-THF;165 similar effects expected with levoleucovorin166 Methotrexate concentrations measured by immunoassay within 48 hours after glucarpidase administration are unreliable165 |
Do not administer leucovorin within 2 hours before or after glucarpidase165 166 During first 48 hours after glucarpidase administration, administer leucovorin at same dosage administered prior to glucarpidase; beyond 48 hours, base dosage on methotrexate concentration165 166 Continue leucovorin therapy until methotrexate concentration remains below the leucovorin treatment threshold for ≥3 days165 166 |
|
Fluorouracil |
Possible potentiation of fluorouracil antineoplastic activity and toxicity102 119 128 141 144 146 147 148 149 150 b c |
|
|
Methotrexate, intrathecal |
Possible decreased methotrexate efficacy if used concomitantly with high doses of leucovorinb c |
Leucovorin Pharmacokinetics
Absorption
Bioavailability
Peak serum concentrations of leucovorin (5-formyl-THF), active metabolite (5-methyl-THF), or total reduced folates attained within several hours.c (See Table 6.)
Dose studied: 25 mg
Doses studied: 15 and 25 mg
|
Route |
Leucovorin |
5-Methyl-THF |
Total Reduced Folates |
|---|---|---|---|
|
Oral |
1.2 hours |
2.4 hours |
1.72 and 2.3 hours |
|
IV |
10 minutes |
1.3 hours |
10 minutes |
|
IM |
28 minutes |
2.8 hours |
40 and 52 minutes |
Oral absorption saturable at doses >25 mg.b c Apparent bioavailability is 97, 75, or 37% for 25-, 50-, or 100-mg dose, respectively.b c
AUC of leucovorin, 5-methyl-THF, and total reduced folates is similar following IV and IM administration.c AUC of total reduced folates following oral administration of 25-mg dose is 92% of that following IV administration.c AUC is 8% less following IM injection in gluteal region than in deltoid region.a
Distribution
Extent
THF and derivatives distributed to all body tissues; liver contains about one-half of total body folate stores.a
Small amounts of 5-methyl-THF distributed into CSF.b c
Elimination
Metabolism
Rapidly metabolized to active metabolite 5-methyl-THF (major transport and storage form of folate in body).a c
Elimination Route
Excreted in urine, mainly as 10-formyl-THF and 5,10-methenyl-THF.a
Urinary excretion of folate becomes approximately logarithmic at doses >1 mg.c
Half-life
Oral administration: 3.5–5.7 hours.b c
IV or IM administration: 6.2 hours (for total reduced folates).c
Stability
Storage
Oral
Tablets
15–30°C.b Protect from light and moisture.b
Parenteral
Injection
2–8°C.c Protect from light; retain in original carton until time of use.c Discard unused portion.c
Powder for Injection
15–30°C.a c Protect from light.a c
Following reconstitution with sterile water for injection, use immediately and discard unused portion.102 c
Following reconstitution with bacteriostatic water for injection, use within 7 days.102 c
Compatibility
Parenteral
Solution CompatibilityHID
|
Compatible |
|---|
|
Dextrose 10% in sodium chloride 0.9% |
|
Dextrose 5 or 10% in water |
|
Ringer’s injection |
|
Ringer’s injection, lactated |
|
Variable |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|---|
|
Cisplatin |
|
Cisplatin with floxuridine |
|
Floxuridine |
|
Incompatible |
|
Fluorouracil |
|
Compatible |
|---|
|
Amifostine |
|
Aztreonam |
|
Bleomycin sulfate |
|
Cefepime HCl |
|
Cisplatin |
|
Cladribine |
|
Cyclophosphamide |
|
Docetaxel |
|
Doxorubicin HCl |
|
Doxorubicin HCl liposome injection |
|
Etoposide phosphate |
|
Filgrastim |
|
Fluconazole |
|
Fluorouracil |
|
Furosemide |
|
Gemcitabine HCl |
|
Granisetron HCl |
|
Heparin sodium |
|
Linezolid |
|
Methotrexate sodium |
|
Metoclopramide HCl |
|
Mitomycin |
|
Oxaliplatin |
|
Pemetrexed disodium |
|
Piperacillin sodium–tazobactam sodium |
|
Tacrolimus |
|
Teniposide |
|
Thiotepa |
|
Vinblastine sulfate |
|
Vincristine sulfate |
|
Incompatible |
|
Amphotericin B cholesteryl sulfate complex |
|
Droperidol |
|
Foscarnet sodium |
|
Lansoprazole |
|
Sodium bicarbonate |
Actions
-
Racemic mixture of diastereoisomers of 5-formyl-THF; reduced form of folic acid.b c Consists of equal amounts of d- and l-isomers; l-isomer (levoleucovorin) is the pharmacologically active isomer.162 163 Does not require reduction by dihydrofolate reductase to participate in reactions utilizing folates.b c
-
Counteracts therapeutic and toxic effects (e.g., hematologic toxicity) of folic acid antagonists (e.g., methotrexate).b c No effect on other established toxicities of methotrexate resulting from drug and/or metabolite precipitation in kidneys (e.g., nephrotoxicity).b c
-
Enhances therapeutic and toxic effects of fluoropyrimidines (e.g., fluorouracil) by stabilizing binding of fluorouracil metabolite (fluorodeoxyridylic acid) to thymidylate synthase (enzyme responsible for DNA repair and replication), thus enhancing inhibition of this enzyme.102 119 128 141 144 146 147 148 149 150 c
Advice to Patients
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.b c
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.b c
-
Importance of informing patients of other important precautionary information.b c (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer's labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
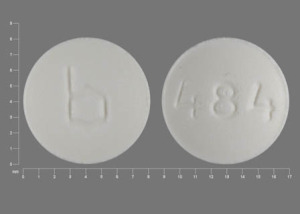
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
5 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|
|
10 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|||
|
15 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|||
|
25 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|||
|
Parenteral |
For injection |
50 mg (of leucovorin)* |
Leucovorin Calcium for Injection |
|
|
100 mg (of leucovorin)* |
Leucovorin Calcium for Injection |
|||
|
200 mg (of leucovorin)* |
Leucovorin Calcium for Injection (preservative-free) |
|||
|
350 mg (of leucovorin)* |
Leucovorin Calcium for Injection |
|||
|
500 mg (of leucovorin)* |
Leucovorin Calcium for Injection (preservative-free) |
|||
|
Injection |
10 mg (of leucovorin) per mL (500 mg)* |
Leucovorin Calcium Injection (preservative-free) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
Only references cited for selected revisions after 1984 are available electronically.
101. Immunex. Leucovorin calcium tablets prescribing information. Seattle, WA; 1994 May.
102. Immunex. Leucovorin calcium for injection prescribing information. Seattle, WA; 1994 May.
103. Engel SI (Lederle Laboratories, Pearl River, NY): personal communication; 1987 Jun.
104. Benvenuto JA, Anderson RW, Kerkof K et al. Stability and compatibility of antitumor agents in glass and plastic containers. Am J Hosp Pharm. 1981; 38:1914-8. https://pubmed.ncbi.nlm.nih.gov/7325172
105. US Public Health Service (USPHS) and Infectious Diseases Society of America (IDSA) Prevention of Opportunistic Infections Working Group. 2001 USPHS/IDSA guidelines for the prevention of opportunistic infections in persons with human immunodeficiency virus. From HIV/AIDS Treatment Information Services (ATIS) website https://www.cdc.gov/mmwr/PDF/rr/rr4810.pdf http://www.aidsinfo.nih.gov
106. Quad Pharmaceuticals. Leucovorin calcium for injection prescribing information. Indianapolis, IN; 1987 Mar.
107. Machover D, Schwarzenberg L, Goldschmidt E et al. Treatment of advanced colorectal and gastric adenocarcinomas with 5-FU combined with high-dose folinic acid: a pilot study. Cancer Treat Rep. 1982; 66:1803-7. https://pubmed.ncbi.nlm.nih.gov/6982099
108. Budd GT, Fleming TR, Bukowski RM et al. 5-fluorouracil and folinic acid in the treatment of metastatic colorectal cancer: a randomized comparison: a Southwest Oncology Group study. J Clin Oncol. 1987; 5:272-7. https://pubmed.ncbi.nlm.nih.gov/3543246
109. Panasci L, Ford J, Margolese R. A phase II study of sequential methotrexate and fluorouracil in advanced colorectal cancer. Cancer Chemother Pharmacol. 1985; 15:164-6. https://pubmed.ncbi.nlm.nih.gov/4017165
110. Glimelius B, Ginman C, Graffman S et al. Sequential methotrexate-5-FU-leucovorin (MFL) in advanced colorectal cancer. Eur J Cancer Clin Oncol. 1986; 22:295-300. https://pubmed.ncbi.nlm.nih.gov/3486768
111. Hansen RM, Ritch PS, Anderson T. Sequential methotrexate, 5-fluorouracil, and calcium leucovorin in colorectal carcinoma. Am J Clin Oncol. 1986; 9:352-4. https://pubmed.ncbi.nlm.nih.gov/3489407
112. Machover D, Goldschmidt E, Chollet P et al. Treatment of advanced colorectal and gastric adenocarcinomas with 5-fluorouracil and high-dose folinic acid. J Clin Oncol. 1986; 4:685-96. https://pubmed.ncbi.nlm.nih.gov/3517242
113. Leone BA, Romero A, Rabinovich MG et al. Sequential therapy with methotrexate and 5-fluorouracil in the treatment of advanced colorectal carcinoma. J Clin Oncol. 1986; 4:23-7. https://pubmed.ncbi.nlm.nih.gov/3941331
114. Petrelli N, Douglass HO Jr, Herrera L et al. The modulation of fluorouracil with leucovorin in metastatic colorectal carcinoma: a prospective randomized phase III trial. J Clin Oncol. 1989; 7:1419-26. https://pubmed.ncbi.nlm.nih.gov/2674331
115. Petrelli NJ, Madajewicz S, Herrera L et al. Biologic modulation of 5-fluorouracil with high-dose leucovorin and combination chemotherapy of 5-fluorouracil and cisplatin in metastatic colorectal adenocarcinoma. In: Development of folates and folic acid antagonists in cancer chemotherapy. NCI monographs 1987 No. 5. NIH Publication No. 87-2901 Number 5 1987. Bethesda, MD: National Cancer Institute; 1987:189-92.
116. Erlichman C, Fine S, Wong A et al. A randomized trial of fluorouracil and folinic acid in patients with metastatic colorectal carcinoma. J Clin Oncol. 1988; 6:469-75. https://pubmed.ncbi.nlm.nih.gov/3280741
117. Doroshow JH, Bertrand M, Newman E et al. Preliminary analysis of a randomized comparison of 5-fluorouracil versus 5-fluorouracil and high dose continuous-infusion folinic acid in disseminated colorectal cancer. In: Development of folate and folate acid antagonists in cancer chemotherapy. NCI Monograph 1987 No. 5. NIH Publication No. 87-2901 Number 5 1987. Bethesda, MD; National Cancer Institute; 1987:171-4.
118. Petrelli N, Herrera L, Rustum Y et al. A prospective randomized trial of 5-fluorouracil versus 5-fluorouracil and high-dose leucovorin versus 5-fluorouracil and methotrexate in previously untreated patients with advanced colorectal cancer. J Clin Oncol. 1987; 5:1559-65. https://pubmed.ncbi.nlm.nih.gov/2443619
119. Evans RM, Laskin JD, Hakala MT. Effect of excess folates and deoxyinosine on the activity and site of action of 5-fluorouracil. Cancer Res. 1981; 41:3288-95. https://pubmed.ncbi.nlm.nih.gov/6973389
120. Lockshin A, Danenberg PV. Biochemical factors affecting the tightness of 5-fluorouridylate binding to human thymidylate synthetase. Biochem Pharmacol. 1981; 30:247-57. https://pubmed.ncbi.nlm.nih.gov/6939434
121. Ullman B, Lee M, Martin DW Jr et al. Cytotoxicity of 5-fluoro-2′deoxyuridine: requirement for reduced folate cofactors and antagonism by methotrexate. Proc Natl Acad Sci USA. 1978; 75:980-3. https://pubmed.ncbi.nlm.nih.gov/147465 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC411383/
122. Waxman S, Bruckner H, Wagle A et al. Potentiation of 5-fluorouracil (5-FU) antimetabolic effect by leucovorin (LV). Proc Annu Meet Am Assoc Cancer Res Proc Annu Meet Am Soc Clin Oncol. 1978; 19:149.
123. Berger SH, Hakala MT. Relationship of dUMP and free FdUMP pools to inhibition of thymidylate synthase by 5-fluorouracil. Mol Pharmacol. 1984; 25:303-9. https://pubmed.ncbi.nlm.nih.gov/6608049
124. Rectal cancer. From: PDQ. Physician data query (database). Bethesda, MD: National Library of Medicine; 1992 June 8.
125. Colon cancer. From: PDQ. Physician data query (database). Bethesda, MD: National Library of Medicine; 1992 June 8.
126. Lederle. Combination chemotherapy with leucovorin calcium and 5-fluorouracil. Pearl River, NY; 1992 Mar.
127. DeLap RJ. The effect of leucovorin on the therapeutic index of fluorouracil in cancer patients. Yale J Biol Med. 1988; 61:23-34. https://pubmed.ncbi.nlm.nih.gov/3284210 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2590394/
128. Saltz L. Drug treatment of colorectal cancer: current status. Drugs. 1991; 42:616-27. https://pubmed.ncbi.nlm.nih.gov/1723364
129. Erlichman C. Fluorouracil and leucovorin for metastatic colorectal cancer. J Chemother. 1990; 2(Suppl 1):38-40. https://pubmed.ncbi.nlm.nih.gov/2195136
130. O’Connell MJ. A phase III trial of 5-fluorouracil and leucovorin in the treatment of advanced colorectal cancer: a Mayo Clinic/North Central Cancer Treatment Group Study. Cancer. 1989; 63:1026-30. https://pubmed.ncbi.nlm.nih.gov/2465076
131. Poon MA, O’Connell MJ, Moertel CG et al. Biochemical modulation of fluorouracil: evidence of significant improvement of survival and quality of life in patients with advanced colorectal carcinoma. J Clin Oncol. 1989; 7:1407-18. https://pubmed.ncbi.nlm.nih.gov/2476530
132. Poon MA, O’Connell MJ, Wieand HS et al. Biochemical modulation of fluorouracil with leucovorin: confirmatory evidence of improved therapeutic efficacy in advanced colorectal carcinoma. J Clin Oncol. 1991; 9:1967-72. https://pubmed.ncbi.nlm.nih.gov/1941055
133. Doroshow JH, Multhauf P, Leong L et al. Prospective randomized comparison of fluorouracil versus fluorouracil and high-dose continuous infusion leucovorin calcium for the treatment of advanced measurable colorectal cancer in patients previously unexposed to chemotherapy. J Clin Oncol. 1990; 8:491-501. https://pubmed.ncbi.nlm.nih.gov/2407810
134. Valone FH, Friedman MA, Wittinger PS et al. Treatment of patients with advanced colorectal carcinomas with fluorouracil alone, high-dose leucovorin plus fluorouracil, or sequential methotrexate, fluorouracil, and leucovorin: a randomized trial of the Northern California Oncology Group. J Clin Oncol. 1989; 7:1427-36. https://pubmed.ncbi.nlm.nih.gov/2789272
135. Erlichman C. Fluorouracil/leucovorin study update. J Clin Oncol. 1991; 9:2076. https://pubmed.ncbi.nlm.nih.gov/1941066
136. Nobile MT, Canobbio L, Sobrero A et al. A randomized trial of 5-fluorouracil alone versus 5-fluorouracil and high-dose leucovorin in untreated advanced colorectal cancer patients. Adv Exp Med Biol. 1988; 244:213-8. https://pubmed.ncbi.nlm.nih.gov/3073656
137. Loffler TM, Weber FW, Hausamen TU. Protracted continuous-infusion 5-fluorouracil with intermittent high-dose leucovorin in advanced and metastatic colorectal cancer: a pilot study. In: Pinedo HM, Rustum YM, eds. Leucovorin modulation of fluoropyrimidines: a new frontier in cancer chemotherapy. New York: Royal Society of Medicine Services; 1989:65-8.
138. Labianca R, Pancera G, Aitini E et al. Folinic acid + 5-fluorouracil (5-FU) versus equidose 5-FU in advanced colorectal cancer. Phase III study of “GISCAD” (Italian Group for the Study of Digestive Tract Cancer). Ann Oncol. 1991; 2:673-9. https://pubmed.ncbi.nlm.nih.gov/1742223
139. Hines JD, Adelstein DJ, Speiss JL et al. Efficacy of high-dose oral leucovorin and 5-fluorouracil in advanced colorectal carcinoma. Cancer. 1989; 63(Suppl):1022-5. https://pubmed.ncbi.nlm.nih.gov/2783879
140. Laufman LR, Brenckman WD Jr, Stydnicki KA et al. Clinical experience with leucovorin and 5-fluorouracil. Cancer. 1989; 63(Suppl):1031-5. https://pubmed.ncbi.nlm.nih.gov/2783880
141. Rustum YM. Biochemical rationale for the 5-fluorouracil leucovorin combination and update of clinical experience. J Chemother. 1990; 2(Suppl 1):5-11. https://pubmed.ncbi.nlm.nih.gov/2195138
142. Gerstner J, O’Connell MJ, Wieand HS et al. A prospectively randomized clinical trial comparing 5-FU combined with either high- or low-dose leucovorin for the treatment of advanced colorectal cancer. Proc Annu Meet Am Soc Clin Oncol. 1991; 10:A404.
143. Grem JL, Shemaker DD, Petrelli NJ et al. Severe and fatal toxic effects observed in treatment with high- and low-dose leucovorin plus 5-fluorouracil for colorectal carcinoma. Cancer Treat Rep. 1987; 71:1122. https://pubmed.ncbi.nlm.nih.gov/3499982
144. Advanced colorectal cancer meta-analysis project. Modulation of fluorouracil by leucovorin in patients with advanced colorectal cancer: evidence in terms of response rate. J Clin Oncol. 1992; 10:896-903. https://pubmed.ncbi.nlm.nih.gov/1534121
145. Bruckner HW, Petrelli NJ, Stablein D et al. Comparison of unique leucovorin and 5-fluorouracil “escalating” and “maximum” dosage strategies. In: Development of folates and folic acid antagonists in cancer chemotherapy. NCI monographs 1987 No. 5. NIH Publication No. 87-2901 Number 5 1987. Bethesda, MD: National Cancer Institute; 1987:179-84.
146. Mini E, Trave F, Rustum YM et al. Enhancement of the antitumor effects of 5-fluorouracil by folinic acid. Pharmacol Ther. 1990; 47:1-19. https://pubmed.ncbi.nlm.nih.gov/2195551
147. Romanini A, Lin JT, Niedzwiecki D et al. Role of folylpolyglutamates in biochemical modulation of fluoropyrimidines by leucovorin. Cancer Res. 1991; 51:789-93. https://pubmed.ncbi.nlm.nih.gov/1988119
148. Machover D. Potentiation of the antitumour activity of the fluoropyrimidines by leucovorin: rationale and clinical data. In: Pinedo HM, Rustum YM, eds. Leucovorin modulation of fluoropyrimidines: a new frontier in cancer chemotherapy. New York: Royal Society of Medicine Services; 1989:1-9.
149. Rustum YM. Rationale for the combination of 5-fluorouracil/leucovorin: role of dose, schedule and route of administration. In: Pinedo HM, Rustum YM, eds. Leucovorin modulation of fluoropyrimidines: a new frontier in cancer chemotherapy. New York: Royal Society of Medicine Services; 1989:11-19.
150. Peters GJ, van der Wilt CL, van Groeningen CJ et al. Development of leucovorin/5-fluorouracil combinations. In: Pinedo HM, Rustum YM, eds. Leucovorin modulation of fluoropyrimidines: a new frontier in cancer chemotherapy. New York: Royal Society of Medicine Services; 1989:21-35.
151. Creaven PJ, Petrelli NJ, Rustum YM. Leucovorin/5-fluorouracil: response and toxicity in relation to quality of life. In: Pinedo HM, Rustum YM, eds. Leucovorin modulation of fluoropyrimidines: a new frontier in cancer chemotherapy. New York: Royal Society of Medicine Services; 1989:57-64.
152. Wilke H, Preusser P, Stahl M et al. Leucovorin/5-fluorouracil alone or in combination with other cytostatic drugs in the treatment of advanced gastric carcinoma. In: Pinedo HM, Rustum YM, eds. Leucovorin modulation of fluoropyrimidines: a new frontier in cancer chemotherapy. New York: Royal Society of Medicine Services; 1989:87-95.
153. Schöber CH, Köhne-Wömpner CH, Schmoll HJ et al. A 3-day schedule of 5-fluorouracil and folinic acid in metastatic progressive colorectal cancer and its impact in terms of palliation. Semin Oncol. 1992; 19(Suppl 3):136-40. https://pubmed.ncbi.nlm.nih.gov/1557639
154. Schöber CH, Bokemeyer C, Stahl M et al. The role of schedule dependency of 5-fluorouracil/leucovorin combinations in advanced colorectal cancer. Semin Oncol. 1992; 19(Suppl 3):131-5. https://pubmed.ncbi.nlm.nih.gov/1557638
155. Steinke B, Günther E, Hirschmann WD et al. Fluorouracil versus folinic acid/fluorouracil in advanced colorectal cancer—preliminary results of a randomized trial. Semin Oncol. 1992; 19(Suppl 3):141-7. https://pubmed.ncbi.nlm.nih.gov/1557640
156. Reviewers’ comments (personal observations).
157. Lederle, Pearl River, NY: personal communication.
158. Nobile MT, Vidili MG, Sobrero A et al. 5-Fluorouracil (FU) alone or combined with high dose folinic acid (FA) in advanced colorectal cancer patients: a randomized trial. Proc Annu Meet Am Soc Clin Oncol. 1988; 7:A371.
159. Kaplan J. Centers for Disease Control and Prevention: personal communication. 1995 Dec.
160. US Bioscience. Neutrexin (trimetrexate glucuronate for injection) prescribing information (dated July 1995). In: Physicians’ desk reference. 51st ed. Montvale, NJ: Medical Economics Company Inc; 1997:2761-4.
161. Anon. Drugs for parasitic infections. Med Lett Drugs Ther. 2002. From website http://www.medletter.com
162. Spectrum Pharmaceuticals, Inc. Fusilev (levoleucovorin calcium) powder for injection prescribing information. Irvine, CA; 2008 Jul.
163. Goorin A, Strother D, Poplack D et al. Safety and efficacy of l-leucovorin rescue following high-dose methotrexate for osteosarcoma. Med Pediatr Oncol. 1995; 24:362-7. https://pubmed.ncbi.nlm.nih.gov/7715542
164. Food and Drug Administration. Orphan designations pursuant to Section 526 of the Federal Food and Cosmetic Act as amended by the Orphan Drug Act (P.L. 97-414), to June 28, 1996. Rockville, MD; 1996 Jul.
165. BTG International Inc. Glucarpidase (Voraxaze) for injection prescribing information. West Conshohocken, PA; 2012 Jan.
166. BTG International Inc. West Conshohocken, PA: Personal communication.
167. Tidwell BH, Cleary JD. Comment: leucovorin-phenytoin: a drug-drug interaction?. Ann Pharmacother. 1995; 29:1303-4. https://pubmed.ncbi.nlm.nih.gov/8672847
a. AHFS drug information 2004. McEvoy GK, ed. Leucovorin Calcium. Bethesda, MD: American Society of Health-System Pharmacists; 2004:3537-40.
b. Roxane Laboratories Inc. Leucovorin calcium tablets USP prescribing information. Columbus, OH; 1999 Aug.
c. Bedford Laboratories. Leucovorin calcium injection USP and leucovorin calcium for injection prescribing information. Bedford, OH; 2000 Sep.
d. Food and Drug Administration. Orphan designations pursuant to Section 526 of the Federal Food and Cosmetic Act as amended by the Orphan Drug Act (P.L. 97-414), to May 4, 2004. Rockville, MD; 2004 Jul.
e. Colon cancer. From: PDQ. Physician data query (database). Bethesda, MD: National Library of Medicine; 2004 Apr 21.
f. Anon. Drugs of choice for cancer. Treatment Guidelines from the Medical Letter. 2003; 1:41-53. https://pubmed.ncbi.nlm.nih.gov/15529105
HID. Trissel LA. Handbook on injectable drugs. 14th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2007:991-6.
Related/similar drugs
Khapzory
Khapzory is used for colorectal cancer, methotrexate overdosage, methotrexate rescue
Opdivo Qvantig
Opdivo Qvantig is used to treat adults with melanoma, non-small cell lung cancer, renal cell ...
Platinol
Platinol is used for bladder cancer, blood cell transplantation, bone marrow transplantation, brain ...
Zynyz
Zynyz is a targeted cancer treatment used to squamous cell carcinoma of the anal canal (SCAC) and ...
Mutamycin
Mutamycin is used for bladder cancer, pancreatic cancer, stomach cancer
Adrucil
Adrucil is used for breast cancer, breast cancer, palliative, cancer, colorectal cancer, pancreatic ...
Zusduri
Zusduri is used to treat recurrent low-grade, intermediate-risk, non-muscle invasive bladder cancer ...
Retifanlimab
Retifanlimab is used for anal cancer, merkel cell carcinoma
Frequently asked questions
- What is the FOLFOX chemo regimen and is it effective?
- What is the FOLFIRI chemo regimen and how does it work?
- What is the FLOT chemotherapy regimen and how does it work?
- What is FOLFIRINOX regimen and how is it used?
More about leucovorin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antidotes
- Breastfeeding
Patient resources
Professional resources
- Calcium Folinate Injection prescribing information
- Leucovorin Injection (FDA)
- Leucovorin Tablets (FDA)