Denosumab (Monograph)
Brand names: Prolia, Xgeva
Drug class: Bone-modifying Agents
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for denosumab to ensure that the benefits outweigh the risk. The REMS may apply to one or more preparations of denosumab and consists of the following: medication guide and communication plan. See https://www.accessdata.fda.gov/scripts/cder/rems/.
Warning
- Severe Hypocalcemia in Patients in Patients with Advanced Kidney Disease
-
Increased risk of severe hypocalcemia in patients with advanced chronic kidney disease (eGFR <30 mL/min/1.73 m2 ), including dialysis-dependent patients, receiving denosumab (Prolia). Severe hypocalcemia resulting in hospitalization, life-threatening events, and fatalities has been reported.
-
Presence of chronic kidney disease-mineral bone disorder (CKD-MBD) markedly increases risk of hypocalcemia in these patients.
-
Prior to initiating denosumab (Prolia) in patients with advanced chronic kidney disease, evaluate for presence of CKD-MBD. Treatment with denosumab in these patients should be supervised by a healthcare provider with expertise in the diagnosis and management of CKD-MBD.
Introduction
Bone resorption inhibitor; fully human monoclonal antibody specific for receptor activator of nuclear factor kappa-B ligand (RANKL); RANKL inhibitor.
Uses for Denosumab
Osteoporosis
Treatment of osteoporosis in postmenopausal women and men at high risk of fracture, defined as history of osteoporotic fracture or multiple risk factors for fracture.
Treatment of osteoporosis in postmenopausal women and men following failure of or intolerance to other available osteoporosis therapies.
When pharmacotherapy for postmenopausal osteoporosis is indicated, denosumab may be used as the initial therapeutic agent, particularly in postmenopausal women who cannot or prefer not to take oral therapy (i.e., bisphosphonates). Some experts suggest reserving denosumab for postmenopausal women who have contraindications to or who experience adverse effects of bisphosphonates. Guidelines suggest using denosumab as a second-line treatment option in osteoporotic men who have contraindications to or who experience adverse effects of bisphosphonates.
Glucocorticoid-induced Osteoporosis
Treatment of glucocorticoid-induced osteoporosis in men and women at high risk of fracture, defined as a history of osteoporotic fracture or multiple risk factors for fracture.
Treatment of glucocorticoid-induced osteoporosis in men and women following failure of or intolerance to other osteoporosis therapies.
Manufacturer recommends use in patients who are either initiating or continuing long-term (≥6 months) systemic glucocorticoid therapy in a dosage equivalent to ≥7.5 mg daily of prednisone.
Guidelines conditionally recommend denosumab as one of several treatment options for adults at moderate to high risk of osteoporotic fracture who are receiving long-term glucocorticoid therapy; choice of therapeutic agent should be based on patient and physician preferences.
Bone Loss Associated with Androgen Deprivation Therapy
Treatment to increase bone mass in men at high risk for fracture receiving androgen deprivation therapy for nonmetastatic prostate cancer.
Guidelines recommend the use of denosumab to reduce the risk of fracture in men with osteoporosis or increased risk of fracture who are receiving androgen deprivation therapy for nonmetastatic prostate cancer.
Bone Loss Associated with Aromatase Inhibitor Therapy
Treatment to increase bone mass in women at high risk for fracture receiving adjuvant aromatase inhibitor therapy for breast cancer.
Guidelines state that denosumab is an option for bone-modifying therapy in postmenopausal women taking aromatase inhibitors who have osteoporosis or who are at increased risk of fracture; selection of a bone-modifying agent in this patient population should be individualized based on patient preference, potential adverse effects, quality of life considerations, adherence, safety, cost, and availability.
Multiple Myeloma and Bone Metastases of Solid Tumors
Prevention of skeletal-related events (SREs) in patients with multiple myeloma or bone metastases from solid tumors.
Guidelines recommend denosumab as an option to prevent SREs in patients with metastatic castration-resistant prostate cancer. Bone-modifying therapy is recommended for patients with metastatic breast cancer and evidence of bone destruction, but no specific agents are recommended for this patient population. For patients with multiple myeloma who have lytic destruction of the bone evident on imaging or compression fracture of the spine from osteopenia, IV bisphosphonates are recommended first line; denosumab is a recommended alternative.
Giant Cell Tumor of Bone
Treatment of giant cell tumor of bone in adults and skeletally mature adolescents (12-16 years of age) if the disease is unresectable or surgical resection is likely to result in severe morbidity.
International experts state that denosumab is standard treatment for patients with unresectable or metastatic giant cell tumor of bone.
Hypercalcemia Associated with Malignancy
Treatment of bisphosphonate-refractory hypercalcemia of malignancy.
Initial treatment for hypercalcemia of malignancy typically consists of aggressive IV hydration and IV bisphosphonates, with denosumab used as an alternative if the response to IV bisphosphonate therapy is inadequate.
Denosumab Dosage and Administration
General
Pretreatment Screening
-
Perform pregnancy testing in females of reproductive potential prior to treatment with denosumab.
-
Check blood calcium levels; pre-existing hypocalcemia must be corrected prior to treatment with denosumab. Adequately supplement all patients with calcium and vitamin D.
-
In patients with advanced chronic kidney disease, evaluate for presence of chronic kidney disease mineral and bone disorder (CKD-MBD) with intact parathyroid hormone (iPTH), serum calcium, 25(OH) vitamin D, and 1,25(OH)2 vitamin D prior to initiating denosumab (Prolia) treatment. Consider also assessing bone turnover status (serum markers of bone turnover or bone biopsy) to evaluate the underlying bone disease that may be present.
-
Perform a dental examination prior to treatment.
Patient Monitoring
-
In patients without advanced chronic kidney disease who are predisposed to hypocalcemia and disturbances of mineral metabolism (e.g., history of hypoparathyroidism, thyroid surgery, parathyroid surgery, malabsorption syndromes, excision of small intestine, treatment with other calcium-lowering drugs), assess serum calcium and mineral levels (phosphorus and magnesium) 10 to 14 days after denosumab (Prolia) administration.
-
In patients with advanced chronic kidney disease (i.e., eGFR <30 mL/min/1.73 m2), monitor serum calcium weekly for the first month after denosumab (Prolia) administration and monthly thereafter.
-
When using denosumab for cancer-related indications, monitor calcium levels throughout therapy, especially in the first weeks of initiating therapy. Monitor calcium levels and calcium and vitamin D intake in patients with severe renal impairment or on dialysis and with inadequate or no calcium supplementation.
-
Monitor serum calcium closely with concomitant use of calcimimetic drugs.
-
When using denosumab for osteoporosis or bone loss indications, monitor for consequences of bone over-suppression.
-
Perform appropriate dental evaluations periodically during therapy and monitor for symptoms of osteonecrosis of the jaw.
Dispensing and Administration Precautions
-
Denosumab is commercially available as Prolia and Xgeva. These products are labeled by the FDA for different indications and should not be used concomitantly.
-
Denosumab prefilled syringe should be administered by a healthcare professional.
Other General Considerations
-
Supplementation with calcium and vitamin D may be required during denosumab treatment. All patients treated with denosumab for osteoporosis or bone loss indications should receive 1000 mg of calcium daily and ≥400 IU of vitamin D daily.
-
When used for treatment of glucocorticoid-induced osteoporosis, denosumab should be used in patients who are either initiating or expected to continue long-term (≥6 months) systemic glucocorticoid therapy in a dosage equivalent to ≥7.5 mg daily of prednisone.
Administration
Sub-Q Administration
Administer by sub-Q injection using single-dose prefilled syringes (Prolia) or single-use vials (Xgeva) into upper arm, upper thigh, or abdomen; do not administer IV, or by IM or intradermal injection.
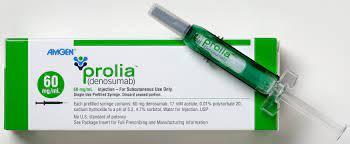
Available as 60-mg/mL solution (Prolia) in single-use prefilled syringes for treatment of osteoporosis (including glucocorticoid-induced osteoporosis) or treatment of bone loss associated with androgen deprivation or aromatase inhibitor therapy. Denosumab prefilled syringes should be administered by a health-care professional.
Available as 120-mg/1.7-mL solution (Xgeva) in single-use vials for cancer-related indications.
Prior to administration, may warm to room temperature by allowing drug to stand in original packaging at room temperature (≤25°C) for approximately 15–30 minutes. Do not warm using any other method.
Solution should appear clear, colorless to pale yellow; may contain trace amounts of translucent to white proteinaceous particles. Do not use if solution is discolored, cloudy, or contains many particles or foreign matter.
Single-use prefilled syringe: Remove gray needle cap and inject entire solution. After injection is complete, activate needle guard by pointing needle away from body and gently sliding green safety guard toward needle until locked securely in place.
Single-use vial: Use 27-gauge needle to withdraw and inject entire vial contents. Do not re-enter vial; discard any remaining solution along with the vial.
Dosage
Pediatric Patients
Giant Cell Tumor of Bone
Treatment in Skeletally Mature Adolescents (12-16 years of age)
Sub-QXgeva: 120 mg once every 4 weeks; during first month of treatment, give additional 120 mg dose on day 8 and day 15.
Supplement with calcium and vitamin D as needed to treat or prevent hypocalcemia.
Adults
Osteoporosis
Treatment in Postmenopausal Women at High Risk for Fracture
Sub-QProlia: 60 mg once every 6 months.
Administer a missed dose as soon as patient is available; schedule subsequent doses every 6 months from date of last dose.
Treatment in Men at High Risk for Fracture
Sub-QProlia: 60 mg once every 6 months.
Administer a missed dose as soon as patient is available; schedule subsequent doses every 6 months from date of last dose.
Glucocorticoid-induced Osteoporosis
Sub-Q
Prolia: 60 mg once every 6 months.
Administer a missed dose as soon as patient is available; schedule subsequent doses every 6 months from date of last dose.
Bone Loss Associated with Androgen Deprivation Therapy
Treatment in Men with Nonmetastatic Prostate Cancer at High Risk for Fracture
Sub-QProlia: 60 mg once every 6 months.
Administer a missed dose as soon as patient is available; schedule subsequent doses every 6 months from date of last dose.
Bone Loss Associated with Adjuvant Aromatase Inhibitor Therapy
Treatment in Women with Breast Cancer at High Risk for Fracture
Sub-QProlia: 60 mg once every 6 months.
Administer a missed dose as soon as patient is available; schedule subsequent doses every 6 months from date of last dose.
Multiple Myeloma and Bone Metastases from Solid Tumors
Prevention of Skeletal-related Events
Sub-QXgeva: 120 mg once every 4 weeks.
Supplement with calcium and vitamin D as needed to treat or prevent hypocalcemia.
Giant Cell Tumor of Bone
Sub-Q
Xgeva: 120 mg once every 4 weeks; during first month of treatment, give additional 120-mg dose on day 8 and day 15.
Supplement with calcium and vitamin D as needed to treat or prevent hypocalcemia.
Hypercalcemia Associated with Malignancy
Sub-Q
Xgeva: 120 mg once every 4 weeks; during first month of treatment, give additional 120-mg dose on day 8 and day 15.
Special Populations
Hepatic Impairment
No specific dosage recommendations.
Renal Impairment
No dosage adjustment necessary. However, patients with severe renal impairment (Clcr <30 mL/minute) or receiving dialysis are at greater risk of developing hypocalcemia.
Geriatric Use
No specific dosage recommendations.
Cautions for Denosumab
Contraindications
-
Hypocalcemia (correct preexisting hypocalcemia prior to initiating denosumab).
-
History of clinically important hypersensitivity (e.g., systemic hypersensitivity) to denosumab or any component in the formulation.
-
The preparation of denosumab labeled for use in the treatment of osteoporosis or bone loss (Prolia) is contraindicated in pregnant women.
Warnings/Precautions
Severe Hypocalcemia and Mineral Metabolism Changes
Severe, life-threatening (including fatalities) hypocalcemia reported; patients with advanced chronic kidney disease at greater risk (see Boxed Warning).
The presence of underlying chronic kidney disease-mineral bone disorder (CKD-MBD, renal osteodystrophy) markedly increases risk of hypocalcemia. Concomitant use of calcimimetic drugs may also worsen risk.
Pre-existing hypocalcemia must be corrected prior to initiating therapy. Monitor patients for hypocalcemia, and supplement calcium, vitamin D, and magnesium as clinically indicated.
In patients without advanced chronic kidney disease who are predisposed to hypocalcemia and disturbances of mineral metabolism (e.g. history of hypoparathyroidism, thyroid surgery, parathyroid surgery, malabsorption syndromes, excision of small intestine, treatment with other calcium-lowering drugs), assess serum calcium and mineral levels (phosphorus and magnesium) 10 to 14 days after denosumab (Prolia) injection for the treatment of osteoporosis or bone loss indications. In some cases, hypocalcemia lasted for weeks or months and required frequent monitoring and IV and/or oral calcium replacement therapy, with or without vitamin D.
In patients with advanced chronic kidney disease, evaluate for presence of CKD-MBD with intact parathyroid hormone (iPTH), serum calcium, 25(OH) vitamin D, and 1,25(OH)2 vitamin D prior to decisions regarding denosumab (Prolia) treatment. Consider also assessing bone turnover status (serum markers of bone turnover or bone biopsy) to evaluate the underlying bone disease that may be present. Treatment should be supervised by a healthcare provider with experience in the diagnosis and management of CKD-MBD.
Patients receiving denosumab for osteoporosis or bone loss indications: All patients should receive 1000 mg of calcium and ≥400 units of vitamin D daily.
Patients receiving denosumab for cancer-related indications: Monitor calcium concentrations throughout therapy, particularly during first weeks following treatment initiation; monitor more frequently in patients receiving concomitant therapy with other drugs that may also reduce serum calcium concentrations. Administer calcium, vitamin D, and magnesium supplementation as necessary.
Choice of Denosumab Products
Commercially available as Prolia and Xgeva; these products are labeled by FDA for different indications.
Do not use Prolia and Xgeva concomitantly.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm based on findings from animal studies and mechanism of action. Fetal loss, stillbirth, postnatal mortality, evidence of absent lymph nodes, abnormal bone growth, reduced bone strength, reduced hematopoiesis, dental dysplasia, tooth malalignment, and decreased neonatal growth reported in reproduction studies in monkeys; some bone abnormalities recovered once drug exposure ceased following birth.
Perform pregnancy testing prior to initiation of therapy in females of reproductive potential.
Denosumab for treatment of osteoporosis or bone loss (Prolia) is contraindicated for use during pregnancy.
Denosumab for cancer-related indications (Xgeva) has a warning associated with use in pregnancy; apprise pregnant women and females of reproductive potential of potential fetal risk if used during pregnancy or within 5 months before conception.
Advise females of reproductive potential to use effective contraceptive methods during denosumab therapy and for ≥5 months after the last dose. Condom use during sexual encounters not necessary in men receiving Prolia.
Sensitivity Reactions
Hypersensitivity
Systemic hypersensitivity reactions (e.g., anaphylaxis, hypotension, dyspnea, throat tightness, facial and upper airway edema, lip swelling, rash, pruritus, urticaria) reported.
If anaphylaxis or other clinically important hypersensitivity reactions occur, initiate appropriate therapy and discontinue denosumab permanently.
Osteonecrosis of the Jaw (ONJ)
ONJ reported. May occur spontaneously, but generally associated with tooth extraction and/or local infection with delayed healing. ONJ may manifest as jaw pain, osteomyelitis, osteitis, bone erosion, tooth or periodontal infection, toothache, gingival ulceration, gingival erosion, or slow healing or persistent pain of the mouth or jaw after dental surgery.
Risk factors for ONJ include invasive dental procedures (e.g., tooth extraction, dental implants, oral surgery), diagnosis of cancer, concomitant therapies (e.g., chemotherapy, immunosuppressive therapy, angiogenesis inhibitors, corticosteroids), poor oral hygiene, use of dental appliances, and comorbidities (e.g., preexisting dental disease, anemia, coagulopathy, diabetes mellitus, infection, ill-fitting dentures). In patients with cancer, longer durations of denosumab use associated with higher incidence of ONJ. Concomitant use of other drugs known to cause ONJ also may increase risk.
Perform routine oral examination and appropriate preventative dentistry prior to initiating denosumab, especially in patients with risk factors for ONJ. All patients should maintain good oral hygiene and receive appropriate preventive dentistry during denosumab treatment.
Avoid invasive dental procedures during denosumab treatment. Consider temporary discontinuance of denosumab therapy in patients requiring invasive dental procedures; however, the optimal duration of treatment interruption is unknown.
If ONJ develops or is suspected, refer patient to dentist or oral surgeon. Extensive dental surgery to treat ONJ may exacerbate the condition. Use clinical judgment and assess risks versus benefits. Consider discontinuing denosumab based on patient-specific risk-benefit assessment.
Atypical Subtrochanteric and Diaphyseal Femoral Fracture
Atypical femoral fractures reported. Such fractures can occur anywhere along the femoral shaft from just below lesser trochanter to above the supracondylar flare and have transverse or short oblique orientation without evidence of comminution.
May be bilateral and often occur with minimal or no trauma to affected area. Many patients report dull or aching thigh pain weeks to months before a complete fracture occurs. Some patients were also receiving glucocorticoid (e.g., prednisone) treatment at time of fracture.
Advise patients receiving denosumab to report new or unusual pain in the thigh, hip, or groin. Evaluate patients with such symptoms to rule out incomplete femur fracture; also evaluate contralateral limb for fracture.
Consider interrupting denosumab treatment pending assessment of risks and benefits of the drug for the individual patient.
Hypercalcemia Following Discontinuance of Therapy
Clinically significant hypercalcemia requiring hospitalization and complicated by acute renal injury reported following discontinuance of denosumab therapy in patients with giant cell tumor of bone and in pediatric patients with growing skeletons. Hypercalcemia reported within the first year following treatment discontinuance.
Following discontinuance of denosumab therapy, monitor patients for manifestations of hypercalcemia, periodically monitor serum calcium concentrations, reevaluate requirements for calcium and vitamin D supplementation, and manage patients as clinically appropriate.
Hypercalcemia in Pediatric Patients with Osteogenesis Imperfecta
Denosumab for osteoporosis or bone loss indications is not approved for use in pediatric patients. Cases of hypercalcemia, some requiring hospitalization, reported in pediatric patients with osteogenesis imperfecta treated with the drug.
Multiple Vertebral Fractures Following Discontinuance of Therapy
Cases of multiple vertebral fractures reported following discontinuance of denosumab therapy. New vertebral fractures reported as early as 7 months (average 19 months) after the last dose.
Patients with risk factors for, or a history of osteoporosis, or with prior vertebral fractures are at increased risk.
When denosumab is discontinued, the risk of fractures, including multiple vertebral fractures, increases. Following discontinuance, markers of bone resorption increase above pretreatment values 9 months after the last dose of the drug and then return to pretreatment values 24 months after the last dose of the drug; bone mineral density (BMD) returns to pretreatment values within 18 months after the last dose.
Assess benefits and risks prior to initiating therapy with denosumab for osteoporosis or bone loss indications; if denosumab is discontinued, transition to an alternative bone resorption inhibitor.
When therapy with denosumab for cancer-related indications is discontinued, evaluate patient’s risk for vertebral fractures.
Serious Infections
May increase risk of serious infections.
Serious skin infections (e.g., cellulitis, erysipelas), endocarditis, and infections of the abdomen, urinary tract, and ear reported in a clinical trial evaluating denosumab in postmenopausal women with osteoporosis; some infections required hospitalization.
Patients receiving concomitant immunosuppressive agents or with impaired immune systems may be at greater risk of serious infections; consider risks and benefits in such patients before starting denosumab. Assess need for continued denosumab treatment in patients who develop serious infections.
Dermatologic Reactions
Adverse epidermal and dermal events (e.g., dermatitis, eczema, rash) reported in a clinical trial evaluating denosumab in postmenopausal women with osteoporosis; most reactions were not specific to the injection site.
Consider discontinuing denosumab if severe dermatologic symptoms develop.
Musculoskeletal Pain
Severe and occasionally incapacitating bone, joint, and/or muscle pain reported in patients receiving denosumab. Symptoms reportedly recurred in some patients following rechallenge with the drug. Time to onset has ranged from 1 day to several months after treatment initiation.
Consider discontinuing denosumab if severe musculoskeletal pain develops.
Suppression of Bone Turnover
Significant suppression of bone remodeling was reported in clinical trials of denosumab in patients with osteoporosis.
Denosumab treatment results in reduction in biochemical bone turnover markers and bone formation rates (as shown by tetracycline labeling).
The significance and long-term effects of the degree of bone remodeling suppression seen with denosumab are unknown. Since these effects may contribute to adverse outcomes, such as ONJ, atypical fractures, and delayed fracture healing, monitor patients for such events.
Immunogenicity and Antibody Formation
Denosumab-binding antibodies were reported in <1% of patients receiving denosumab for periods of up to 5 years. Denosumab-neutralizing antibodies not reported to date and antibody formation does not appear to affect denosumab pharmacokinetics, toxicity, or efficacy.
Specific Populations
Pregnancy
Based on findings from animal studies and its mechanism of action, denosumab may cause fetal harm if administered to pregnant women.
Lactation
Not known whether denosumab distributes into human milk; effects of the drug on breast-fed infants or on milk production are also unknown.
Distributes into milk in monkeys in concentrations up to 0.5% of serum concentrations up to one month after the last dose.
Studies in pregnant mice indicate denosumab exposure during pregnancy may impair maternal mammary gland development and lactation; however, no such impairment observed in monkeys.
Do not breast-feed during treatment with denosumab for osteoporosis indications. When used for cancer-related indications, consider developmental and health benefits of breast-feeding along with the mother’s need for treatment and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Females and Males of Reproductive Potential
Confirm pregnancy status prior to initiation of therapy in females of reproductive potential.
Females of reproductive potential should use effective methods of contraception during denosumab therapy and for ≥5 months after the last dose.
Manufacturer states use of a condom during sexual encounters is not necessary in men receiving treatment with Prolia. Although denosumab is present in low concentrations in seminal fluid after administration of a single 60-mg dose, the manufacturer states that it is unlikely that a female partner or fetus would be exposed to pharmacologically relevant concentrations.
Pediatric Use
Safety and efficacy of denosumab (Xgeva) established for treatment of giant cell tumor of bone in skeletally mature adolescents (12–16 years of age). Safety and efficacy not established for any other indication in pediatric patients.
Safety and efficacy of denosumab (Prolia) not established in pediatric patients; not approved in pediatric patients. Cases of hypercalcemia (some requiring hospitalization and/or complicated by acute kidney injury) reported in clinical trials of pediatric patients with osteogenesis imperfecta treated with denosumab. In pediatric patients <4 years of age, denosumab may adversely affect long-bone growth and dentition based on evidence from animal studies.
Clinically important hypercalcemia reported following discontinuance of denosumab therapy in pediatric patients with growing skeletons who received the drug for treatment of giant cell tumor of bone or for other off-label uses. Based on animal data, denosumab may impair bone growth in children with open growth plates and may inhibit eruption of dentition.
Geriatric Use
No overall differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.
Hepatic Impairment
No pharmacokinetic studies performed in patients with hepatic impairment.
Renal Impairment
Pharmacokinetics not affected by renal impairment. Risk of hypocalcemia increases with increasing renal impairment; most common in patients with severe renal impairment (Clcr <30 mL/minute) or receiving dialysis and those receiving inadequate or no calcium supplementation. Marked elevations in serum parathyroid hormone (PTH) concentrations may also occur in patients with severe renal impairment or receiving dialysis.
Consider risks and benefits when using denosumab in patients with severe renal impairment or receiving dialysis. Monitor calcium, phosphorus, and magnesium levels, and calcium and vitamin D intake.
Common Adverse Effects
Adverse effects (>5%) in patients receiving denosumab for the treatment of osteoporosis: back pain, extremity pain, musculoskeletal pain, hypercholesterolemia, cystitis (in postmenopausal women) or back pain, arthralgia, nasopharyngitis (in men).
Adverse effects (>3%) in patients receiving denosumab for the treatment of glucocorticoid-induced osteoporosis: back pain, hypertension, bronchitis, headache.
Adverse effects (≥10%) in patients receiving denosumab for bone loss associated with androgen deprivation or aromatase inhibitor therapy: arthralgia, back pain. Musculoskeletal and extremity pain also reported.
Adverse effects (≥25%) in patients with bone metastases from solid tumors: fatigue/asthenia, hypophosphatemia, nausea.
Adverse effects (≥10%) in patients with multiple myeloma: diarrhea, nausea, anemia, back pain, thrombocytopenia, peripheral edema, hypocalcemia, upper respiratory infection, rash, headache.
Adverse effects (≥10%) in patients with giant cell tumor of bone: arthralgia, headache, nausea, back pain, fatigue, extremity pain.
Adverse effects (>20%) in patients with bisphosphonate-refractory hypercalcemia of malignancy: nausea, dyspnea, decreased appetite, headache, peripheral edema, vomiting, anemia, constipation, diarrhea.
Drug Interactions
Drugs Metabolized by Hepatic Microsomal Enzymes
Clinically important drug interactions not expected when denosumab used concomitantly with drugs metabolized by CYP3A4 in postmenopausal women with osteoporosis. Denosumab not expected to alter pharmacokinetics of these drugs.
Drugs Affecting Serum Calcium Concentrations
Monitor serum calcium concentrations more closely in patients receiving concomitant therapy with calcimimetics and other drugs that may also reduce serum calcium concentrations.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antineoplastic agents |
No evidence that chemotherapy and/or hormone therapy affect denosumab pharmacokinetics or pharmacodynamics |
|
|
Etanercept |
No effect on etanercept pharmacokinetics in postmenopausal women with rheumatoid arthritis and low BMD |
|
|
Immunosuppressive agents |
Possible increased risk of serious infections |
Assess risks and benefits of denosumab in patients receiving immunosuppressive agents |
|
Midazolam |
No clinically important effect on midazolam pharmacokinetics in postmenopausal women with osteoporosis |
Denosumab Pharmacokinetics
Absorption
Bioavailability
Approximately 62% following sub-Q administration.
Prolonged absorption phase; median time to peak serum concentrations after single 60-mg sub-Q dose is 10 days (range 3–21 days).
No accumulation observed at dosage of 60 mg every 6 months. At dosage of 120 mg every 4 weeks, accumulation is up to 2.8-fold and steady-state concentrations are achieved by 6 months. At dosage of 120 mg every 4 weeks, with additional 120-mg dose on day 8 and day 15 during first month of therapy, steady state achieved in 3 months.
Characterization of other monoclonal antibodies indicates that absorption is probably mediated by the lymphatic system.
Onset
Studies in postmenopausal women with osteoporosis indicate reduction in bone resorption biomarkers observed within 3 days after a 60-mg dose; maximal reductions observed by 1 month.
Duration
Studies in postmenopausal women with osteoporosis indicate effect on bone resorption markers partially attenuated at the end of each 6-month dosing interval. Bone mineral density (BMD) and levels of bone resorption markers return to baseline within 12 months after discontinuing denosumab.
Distribution
Extent
Not known whether distributed into human milk. Distributed into milk in monkeys (concentrations up to 0.5% of serum concentrations at up to 1 month after the last dose).
Present in seminal fluid in low concentrations (maximum concentration of approximately 2% of serum concentrations) following administration of a single 60-mg dose; maximum amount of denosumab delivered to a female partner during vaginal intercourse would result in exposure levels approximately 11,000 times lower than those in a patient receiving a 60-mg dose of the drug and at least 38 times lower than the observed no biologic effect level in monkeys.
Elimination
Elimination Route
Clearance may occur via reticuloendothelial system; renal excretion not expected.
Half-life
Approximately 25–28 days.
Special Populations
Pharmacokinetics not evaluated in patients with hepatic impairment; pharmacokinetics not affected by renal impairment.
Studies using denosumab dosage of 60 mg once every 6 months indicate pharmacokinetics not affected by body weight. Studies using dosage of 120 mg once every 4 weeks indicate steady-state exposure is lower in 120-kg patients compared with 66-kg patients.
Age, race, and gender do not affect pharmacokinetics. Pharmacokinetics similar between adults and skeletally-mature adolescents with giant cell tumor of bone at dosage of 120 mg once every 4 weeks with a 120-mg loading dose on days 8 and 15.
Stability
Storage
Parenteral
Injection for Sub-Q Use
Prolia single-use prefilled syringes and Xgevasingle-use vials: Store at 2–8ºC in original container; do not freeze.
Use within 14 days after removal from refrigerator; discard if not used within 14 days. After removal from refrigeration, do not expose to temperatures >25ºC, or to direct light or heat.
Do not shake vigorously.
Actions
-
Denosumab, a fully human monoclonal IgG2 antibody, is a bone resorption inhibitor.
-
Denosumab is specific for and binds to RANKL, and acts as a RANKL inhibitor preventing interaction with its receptor (RANK). The interaction between RANK and RANKL is integral to normal bone resorption process. As a result, denosumab inhibits osteoclast formation, function, and survival, ultimately decreasing bone resorption.
-
In postmenopausal women with osteoporosis, denosumab increases BMD and reduces incidence of vertebral, nonvertebral, and hip fractures.
-
In patients with bone loss associated with androgen deprivation or aromatase inhibitor therapy, denosumab increases BMD; also reduces incidence of vertebral fractures in men with prostate cancer receiving androgen deprivation therapy.
-
In patients with solid tumors and metastases to the bone, denosumab delays time to first skeletal-related event.
-
Effects of denosumab are considered reversible since bone turnover markers and BMD return to baseline within 12 months after the drug is discontinued.
-
In giant cell tumors of bone, stromal cells express RANKL and osteoclast-like giant cells express RANK receptor; signaling through the RANK receptor contributes to osteolysis and tumor growth. Denosumab prevents RANKL from activating the receptor on the surfaces of osteoclasts, their precursors, and osteoclast-like giant cells.
Advice to Patients
-
Inform patients to read the medication guide for denosumab prefilled syringe prior to initiating therapy and prior to each subsequent dose; provide the medication guide to the patient each time the drug is administered.
-
Advise patients that denosumab is commercially available as Prolia and Xgeva; patients should not receive concomitant treatment with both drugs.
-
Advise patients to adequately supplement with calcium and vitamin D during denosumab therapy, and instruct them on the importance of maintaining serum calcium levels during treatment. Instruct patients to seek medical attention if signs or symptoms of hypocalcemia develop (e.g., spasms, twitches, muscle cramps, numbness or tingling in fingers, toes, or near mouth).
-
Advise patients with advanced chronic kidney disease, including those who are dialysis-dependent, about the symptoms of hypocalcemia and the importance of maintaining serum calcium levels with adequate calcium and activated vitamin D supplementation. Advise these patients to have their serum calcium measured weekly for the first month after denosumab (Prolia) administration and monthly thereafter.
-
Advise patients to seek prompt medical attention if they develop symptoms of hypersensitivity (e.g., rash, urticaria, pruritus, swelling of face, lips, or tongue, shortness of breath, hypotension, throat tightness). Advise such patients they should not receive further doses of denosumab.
-
Advise patients to seek prompt medical attention if they develop signs or symptoms of infection (e.g., fever, chills, severe abdominal pain, frequent or urgent need to urinate or burning feeling when urinating, skin that is red, swollen, hot, or tender to touch, shortness of breath or cough that persists).
-
Advise patients to seek prompt medical attention if they develop signs or symptoms of dermatologic reactions (e.g., redness, itching, rash, dry skin, blisters that ooze or crust, peeling skin).
-
Advise patients to maintain good oral hygiene during denosumab treatment and to inform their dentist about denosumab treatment prior to dental procedures. Advise patients to avoid invasive dental procedures during treatment with denosumab single-use vial. Advise patients to inform clinician or dentist if persistent pain and/or slow healing of mouth or jaw occurs after dental surgery, or if symptoms of osteonecrosis of the jaw (pain, numbness, swelling of or drainage from the jaw, mouth, or teeth) occur at any time.
-
Advise patients to report new or unusual thigh, hip, or groin pain since these may be symptoms of atypical femoral fracture.
-
Advise patients that the risk for multiple vertebral fractures may be increased after denosumab therapy is discontinued, particularly in those with a history of osteoporosis or vertebral fractures. Advise patients not to interrupt denosumab therapy without consulting their clinician.
-
Advise patients of the potential for hypercalcemia following discontinuance of therapy with denosumab single-use vial in patients with giant cell tumor of bone and in pediatric patients with growing skeletons. Advise patients to report symptoms of hypercalcemia (e.g., nausea, vomiting, headache, decreased alertness) following denosumab discontinuance.
-
Advise patients to inform their clinician if severe bone, joint, and/or muscle pain occurs.
-
Inform patients receiving denosumab prefilled syringe that if a dose is missed, the injection should be given as soon as convenient, and subsequent doses should be scheduled every 6 months from the date of last dose.
-
Advise women to inform their clinician immediately if they are or plan to become pregnant or plan to breast-feed. Advise female patients of reproductive potential to complete a pregnancy test prior to initiation of denosumab, and to use effective methods of contraception during therapy and ≥5 months after the last dose. Advise patients not to use denosumab prefilled syringe while pregnant or breast-feeding. Advise patients who wish to begin breast-feeding after treatment with denosumab prefilled syringe to discuss the appropriate timing with their clinician.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
60 mg/mL |
Prolia (available as a single-dose prefilled syringe) |
Amgen |
|
120 mg/1.7 mL |
Xgeva (available as a single-dose vial) |
Amgen |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Biological Products Related to denosumab
Find detailed information on biosimilars for this medication.
Frequently asked questions
- How long should you take Xgeva for?
- How many years should you take Prolia?
- Is Xgeva a chemotherapy drug?
- Does Xgeva cause bone pain?
- Does Xgeva cause low blood pressure?
More about denosumab
- Check interactions
- Compare alternatives
- Reviews (396)
- Latest FDA alerts (1)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: miscellaneous bone resorption inhibitors
- Breastfeeding
- En español