Chlorthalidone (Monograph)
Drug class: Thiazide-like Diuretics
- Diuretics, Thiazide
VA class: CV701
Chlorthalidone (Systemic) is also contained as an ingredient in the following combinations:
Atenolol and Chlorthalidone
Introduction
Diuretic and antihypertensive agent, structurally and pharmacologically similar to thiazides.
Uses for Chlorthalidone
Hypertension
Used alone or in combination with other antihypertensive agents for all stages of hypertension.
Classified as a thiazide-like drug with regard to management of hypertension.
Thiazide-type diuretics are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include ACE inhibitors, angiotensin II receptor antagonists, and calcium-channel blockers. While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BPs to achieve with drug therapy and/or nonpharmacologic intervention) <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Previous hypertension guidelines have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the current ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient’s BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the current ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years of age are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg. Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Black hypertensive patients generally tend to respond better to monotherapy with thiazide diuretics or calcium-channel blockers than to other antihypertensive drug classes (e.g., ACE inhibitors, angiotensin II receptor antagonists). However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.
Thiazide-like diuretics may be preferred in hypertensive patients with osteoporosis. Secondary beneficial effect in hypertensive geriatric patients of reducing the risk of osteoporosis due to effect on calcium homeostasis and bone mineralization.
Edema (General)
Management of edema resulting from various causes; diagnose etiology before use.
Edema caused by renal disease or by corticosteroids or estrogens may be relatively resistant to treatment.
Ineffective in patients with Scr or BUN concentrations greater than twice normal.
May be ineffective in patients with a GFR of <15–25 mL/minute; even when GFR is 25–50 mL/minute, more potent (e.g., loop) diuretics may be indicated.
No substantial difference in clinical effects or toxicity of comparable thiazide or thiazide-like diuretics, except metolazone may be more effective in edema with renal impairment.
Edema in Pregnancy
Generally responds well to thiazides except when caused by renal disease.
Thiazides should not be used for routine therapy in pregnant women with mild edema who are otherwise healthy.
Edema in Heart Failure
Management of edema associated with heart failure.
Most experts state that all patients with symptomatic heart failure who have evidence for, or a history of, fluid retention generally should receive diuretic therapy in conjunction with moderate sodium restriction, an agent to inhibit the renin-angiotensin-aldosterone (RAA) system (e.g., ACE inhibitor, angiotensin II receptor antagonist, angiotensin receptor-neprilysin inhibitor [ARNI]), a β-adrenergic blocking agent (β-blocker), and in selected patients, an aldosterone antagonist.
Do not use diuretics as monotherapy in heart failure even if symptoms (e.g., peripheral edema, pulmonary congestion) are well controlled; diuretics alone do not prevent progression of heart failure.
Diuretics produce rapid symptomatic benefits, relieving pulmonary and peripheral edema more rapidly (within hours or days) than cardiac glycosides, ACE inhibitors, or β-blockers (in weeks or months).
Once fluid retention has resolved in heart failure, diuretic therapy should be maintained to prevent recurrence of fluid retention. Ideally, diuretic therapy should be adjusted according to changes in body weight (as an indicator of fluid retention) rather than maintained at a fixed dosage.
Diuretics should be continued in heart failure and comorbid conditions (e.g., hypertension) where ongoing therapy with the drugs is indicated.
Edema Secondary to Nephrotic Syndrome
May be useful if the patient fails to respond to corticosteroid therapy.
More likely to become refractory to thiazides than edema associated with heart failure, and more potent diuretics may be required.
Diabetes Insipidus
Has been used widely in the treatment of diabetes insipidus† [off-label].
Effective in both the neurohypophyseal and nephrogenic forms of the disease, decreasing urine volume by up to 50%.
Particularly useful in nephrogenic diabetes insipidus, since this form of the disease is unresponsive to vasopressin and chlorpropamide.
Useful in patients who are allergic or refractory to vasopressin and have been used in combination with one of these hormones and a low-salt diet in patients who excrete an exceptionally large volume of urine.
Renal Tubular Acidosis
Has been used with success in the treatment of electrolyte disturbances associated with renal tubular acidosis† [off-label].
Renal Calculus Formation
Has been used with success in the prophylaxis of renal calculus formation associated with hypercalciuria† [off-label].
Chlorthalidone Dosage and Administration
General
Monitoring and BP Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
Assess patient’s renal function and electrolytes 2–4 weeks after initiation of diuretic therapy. (See Electrolyte Imbalance under Cautions.)
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker). Many patients will require at least 2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved, add a third drug.
Administration
Administer orally.
Dosage
Individualize according to requirements and response.
If added to potent hypotensive agent regimen, initially reduce hypotensive dosage to avoid the possibility of severe hypotension.
For the management of fluid retention associated with heart failure, experts state that diuretics should be administered at a dosage sufficient to achieve optimal volume status and relieve congestion without inducing excessively rapid reduction in intravascular volume, which could result in hypotension, renal dysfunction, or both.
Pediatric Patients
Hypertension† [off-label]
Oral
Children: Initially, 0.3 mg/kg once daily recommended by some experts. May increase dosage every 2–4 weeks until BP controlled, maximum dosage reached (2 mg/kg [up to 50 mg] daily), or adverse effects occur.
Adults
Hypertension
Usual Dosage
OralManufacturer recommends initial dosage of 25 mg once daily; may be increased to 50 mg once daily.
Some experts recommend dosage of 12.5–25 mg once daily based on efficacy and tolerance demonstrated in clinical studies.
Dosages >100 mg daily usually do not increase efficacy.
Fixed-combination Therapy
OralInitially, administer each drug separately to adjust dosage; may use fixed combination if optimum maintenance dosage corresponds to drug ratio in combination preparation.
Manufacturer states that fixed-combination preparations containing chlorthalidone and atenolol should not be used for initial antihypertensive therapy; however, some experts state that use of a fixed-combination preparation may increase patient compliance.
Edema
Oral
Initial dosage: Usually, 50–100 mg daily in a single dose after breakfast.
Alternatively, initiate 100 mg every other day or 3 times a week; some patients require dosages of 150–200 mg daily or every other day.
Dosages >200 mg daily do not produce a greater response.
Maintenance dosage: Reduction of dosage to a lower level may be possible after several days or when nonedematous weight is attained.
Management of fluid retention associated with heart failure: Some experts recommend initiating chlorthalidone at a low dosage (e.g., 12.5–25 mg once daily) and increasing dosage until urine output increases and weight decreases, generally by 0.5–1 kg daily.
Prescribing Limits
Pediatric Patients
Hypertension† [off-label]
Oral
Maximum 2 mg/kg (up to 50 mg) once daily.
Adults
Hypertension
Oral
Dosages >100 mg daily do not produce a greater response.
Edema
Oral
Dosages >200 mg daily do not produce a greater response.
Management of fluid retention in heart failure: 100 mg maximum daily dose recommended by ACCF/AHA.
Special Populations
Hepatic Impairment
No specific dosage recommendations for hepatic impairment; caution because of risk of precipitating hepatic coma.
Renal Impairment
No specific dosage recommendations for renal impairment; caution because of risk of precipitating azotemia.
Cautions for Chlorthalidone
Contraindications
-
Anuria.
-
Known hypersensitivity to hydrochlorothiazide, other thiazides, or any ingredient in the formulation.
-
Although manufacturers state allergy to other sulfonamide derivatives is a contraindication, evidence to support cross-sensitivity is limited, and history of sensitivity to sulfonamide anti-infectives (“sulfa sensitivity”) should not be considered an absolute contraindication.
Warnings/Precautions
Warnings
Hypotensive Agents
May potentiate effects of other hypotensive agents. Although additive or potentiated antihypertensive effects usually are used to therapeutic advantage, hypotension could occur. (See Interactions.)
Lupus Erythematosus
Possible exacerbation or activation of systemic lupus erythematosus.
Sensitivity Reactions
Hypersensitivity
May occur with or without history of allergy or bronchial asthma.
Sulfonamide cross-sensitivity unlikely. (See Contraindications under Cautions.)
General Precautions
Electrolyte Imbalance
Monitor for fluid or electrolyte imbalance (hyponatremia, hypochloremic alkalosis, hypokalemia) prior to initiation of treatment and periodically thereafter.
Observe for signs of electrolyte imbalance (e.g., dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, , oliguria, muscle pains, cramps, muscular fatigue, hypotension, tachycardia, nausea, vomiting).
Perform periodic serum electrolyte determinations (particularly of potassium, sodium, chloride, and bicarbonate); institute measures to maintain normal serum concentrations if necessary.
Serum and urinary electrolyte measurements are especially important with diabetes mellitus, vomiting, diarrhea, parenteral fluid therapy, or expectations of excessive diuresis.
Weekly (or more frequent) electrolyte measurement early in treatment; possible to extend interval between measurements to ≥3 months when electrolyte response has stabilized.
Hypokalemia
May occur after brisk diuresis, when cirrhosis is present, or with prolonged therapy; inadequate oral electrolyte intake may contribute.
May cause cardiac arrhythmias, exaggerate cardiac response to cardiac glycoside toxicity (increase ventricular irritability).
Use potassium-sparing diuretics and/or potassium supplementation to avoid or treat hypokalemia.
Hypochloremia
Generally mild, usually does not require specific treatment except in renal or hepatic impairment.
Chloride replacement may be required for metabolic acidosis.
Hyponatremia
Dilutional hyponatremia may occur in edematous patients in hot weather; appropriate treatment usually is water restriction rather than salt administration except when hyponatremia is life-threatening.
In actual salt depletion, appropriate replacement is treatment of choice.
Gout
Hyperuricemia or, rarely, precipitation of gout may occur; generally avoid or use with caution in patients with history of gout unless patient is receiving uric acid lowering therapy.
Hyperglycemia
In diabetic patients, dosage adjustment of insulin or oral hypoglycemics may be required; hyperglycemia may occur and latent diabetes mellitus may become evident.
Sympathectomy
Antihypertensive effect may be enhanced after sympathectomy.
Hypomagnesemia
May increase magnesium urinary excretion, resulting in hypomagnesemia.
Hypercalcemia
May decrease calcium urinary excretion, cause slight intermittent serum calcium increase in absence of known calcium metabolism disorder; marked hypercalcemia may indicate hyperparathyroidism.
Discontinue prior to performing parathyroid tests.
Hyperlipidemia
May increase cholesterol and triglyceride concentrations.
Clinical importance of these changes is unknown. Diet low in saturated fat and cholesterol usually compensates.
Hypotensive Effects
Orthostatic hypotension rarely occurs.
Specific Populations
Pregnancy
Category B.
Diuretics are considered second-line agents for control of chronic hypertension in pregnant women; if initiation of antihypertensive therapy is necessary during pregnancy, other antihypertensives (i.e., methyldopa, nifedipine, labetalol) are preferred.
Edema associated with pregnancy generally responds well to thiazides except when caused by renal disease; however, do not use as routine therapy in pregnant women with mild edema who are otherwise healthy.
Diuretics are not recommended for prevention or management of gestational hypertension or preeclampsia.
Lactation
Distributed into milk. Manufacturer states to discontinue nursing or the drug; however, considered to be compatible with breast-feeding.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
Elderly may be at increased risk of dilutional hyponatremia, especially underweight females with poor oral fluid and electrolyte intake or excessive low-sodium nutritional supplement intake. (See Hyponatremia under Cautions.)
Hepatic Impairment
Use with caution in hepatic impairment or progressive liver disease (particularly with associated potassium deficiency); electrolyte imbalance may precipitate hepatic coma.
Discontinue immediately if signs of impending hepatic coma appear.
Renal Impairment
Use with caution in severe renal impairment; thiazides decrease GFR and may precipitate azotemia. Effects may be cumulative in impaired renal function.
Common Adverse Effects
Potassium depletion, hyperuricemia (usually asymptomatic; rarely leading to gout). Hypochloremic alkalosis in patients at risk (e.g., hypokalemic patients). Hyperglycemia and glycosuria in diabetics.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Increased risk of postural hypotension |
|
|
Amphetamine |
Thiazides may cause slightly more alkaline urinary pH; may decrease urinary excretion of some amines (e.g., amphetamine) with concurrent use |
Urine pH change is not great during thiazide use, and toxic blood concentrations of amines usually do not occur Monitor for signs of toxicity after initiation of thiazides in patients receiving amphetamine |
|
Amphotericin B |
Additive/potentiated potassium loss |
Severe potassium depletion may occur when used concomitantly |
|
Anticoagulants, oral |
Postulated that may antagonize oral anticoagulant effects |
Confirmatory evidence is lacking |
|
Antidiabetic agents (sulfonylureas) |
Thiazide hyperglycemic effect may exacerbate diabetes mellitus, increase antidiabetic agent requirements, and/or cause temporary loss of diabetic control or secondary failure to antidiabetic agent |
|
|
Barbiturates |
Increased risk of postural hypotension with thiazides |
|
|
Cholestyramine or colestipol resin |
May bind thiazides, reduce their GI absorption, with cholestyramine reportedly producing greater binding in vitro |
Administer thiazides at least 2 hours before cholestyramine or colestipol when used concomitantly |
|
Corticosteroids |
Additive/potentiated potassium loss |
Severe potassium depletion may occur when used concomitantly |
|
Corticotropin |
Additive/potentiated potassium loss |
Severe potassium depletion may occur when used concomitantly |
|
Diazoxide |
May potentiate diazoxide hyperglycemic, hypotensive, and hyperuricemic effects |
Use concomitantly with caution |
|
Digitalis glycosides |
Thiazide-induced electrolyte disturbances (principally hypokalemia, but also hypomagnesemia and hypercalcemia) may increase digitalis toxicity risk |
Perform periodic electrolyte determinations with concomitant use; correct hypokalemia if warranted |
|
Hypotensive agents |
Increased hypotensive effects of most other hypotensive agents Addition of thiazide to stabilized regimen with potent hypotensive agent (e.g., guanethidine, methyldopa, ganglionic blocking agent) may cause severe postural hypotension |
Usually used to therapeutic advantage |
|
Insulin |
May exacerbate diabetes mellitus, increase insulin requirements, cause temporary loss of diabetic control, or secondary failure to insulin. |
|
|
Lithium |
Thiazides (sometimes used with lithium to reduce lithium-induced polyuria) reduced renal lithium clearance within several days Can increase serum lithium concentrations and the risk of lithium intoxication |
Occasionally, used to therapeutic advantage to reduce lithium-induced polyuria, but reduce lithium dosage by about 50% and monitor serum lithium carefully. Generally, avoid concomitant use because of increased lithium toxicity risk. |
|
Methenamine |
Urinary alkalinization may decrease the effectiveness of methenamine compounds which require a urinary pH of ≤5.5 for optimal activity |
Monitor urine pH during concurrent therapy |
|
Neuromuscular blocking agents (e.g., tubocurarine chloride or gallamine triethiodide [both no longer commercially available in the US]) |
May cause prolonged neuromuscular blockade |
Confirmatory evidence lacking |
|
NSAIAs |
Increased risk of NSAIA-induced renal failure secondary to prostaglandin inhibition and decreased renal blood flow NSAIAs may interfere with the natriuretic, diuretic, and antihypertensive response to diuretics |
Monitor closely for possible adverse effects and/or attenuation of diuretic-induced therapeutic effects during concomitant use |
|
Opiates |
Increased risk of postural hypotension with thiazides |
|
|
Probenecid |
Blocks thiazide-induced uric acid retention Also blocks renal tubular secretion of thiazide, but effect on thiazide duration of action apparently not studied Apparently enhances excretion of calcium, magnesium, and citrate during thiazide therapy, but urinary calcium concentrations remain below normal Sodium, potassium, ammonia, chloride, bicarbonate, phosphate, and titratable acid excretion apparently not affected by concomitant probenecid and thiazide therapy |
Used to therapeutic advantage |
|
Quinidine |
Thiazides may cause slightly more alkaline urinary pH; may decrease urinary excretion of some amines (e.g., quinidine) with concurrent use |
Urine pH change is not great during thiazide use and, toxic blood concentrations of amines usually do not occur Monitor for signs of toxicity after initiation of thiazide |
|
Test, Amylase (serum) |
Values may be increased substantially in both asymptomatic patients and in patients developing acute pancreatitis who are receiving thiazides |
|
|
Test, Corticosteroids (urinary) (Glenn-Nelson technique) |
Decreased values by interfering in vitro with the absorbance in the modified Glenn-Nelson technique for urinary 17-hydroxycorticosteroids; may also decrease urinary cortisol excretion |
Importance on urinary corticosteroids is unclear |
|
Test, Histamine for pheochromocytoma |
False-negative results |
|
|
Test, Parathyroid function tests |
May elevate serum calcium in the absence of known disorders of calcium metabolism |
Discontinue thiazides prior to performing parathyroid function tests |
|
Test, Phenolsulfonphthalein (PSP) |
Thiazides compete with PSP for secretion by the proximal renal tubules |
Importance unknown |
|
Test, Phentolamine |
False-negative results |
|
|
Test, Protein-bound iodine (PBI) |
Values may be decreased, although usually not to subnormal |
|
|
Test, Triiodothyronine resin uptake |
Decreased slightly, but 24-hour I 131 uptake is not affected |
|
|
Test, Tyramine |
False-negative results |
|
|
Vasopressors (e.g., norepinephrine) |
Possible decreased arterial responsiveness to vasopressor amines |
Clinical importance not established; decrease in pressor response not sufficient to preclude vasopressor use |
Chlorthalidone Pharmacokinetics
Absorption
Bioavailability
Absorbed from the GI tract.
Onset
Diuretic action begins around 2.6 hours after dosing.
Duration
Up to 72 hours.
Distribution
Plasma Protein Binding
About 75%; 58% is bound to albumin.
Elimination
Elimination Route
30–60% excreted unchanged in urine.
Half-life
40–60 hours.
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 20–25°C.
Actions
-
Exact mechanism of diuretic action is unclear; may act by altering metabolism of the tubular cells.
-
Enhances excretion of sodium, chloride, and water by interfering with the transport of sodium ions across the renal tubular epithelium.
-
Primary site of diuretic action appears to be the cortical diluting segment of the nephron.
-
GFR decreases, but unclear whether secondary to a direct effect on renal vasculature or to the decrease in intravascular fluid volume or an increase in tubular pressure caused by the inhibition of sodium and water reabsorption. The fall in GFR is not important in the mechanism of action.
-
Enhances urinary excretion of potassium secondary to increased amount of sodium at distal tubular site of sodium-potassium exchange.
-
Increases urinary bicarbonate excretion (although to a lesser extent than chloride excretion) but change in urinary pH is usually minimal; diuretic efficacy is not affected by the acid-base balance of the patient.
-
Hypocalciuric effect is thought to result from a decrease in extracellular fluid (ECF) volume, although calcium reabsorption in the nephron may be increased; also, slight or intermittent elevations in serum calcium concentration.
-
Rate of uric acid excretion is decreased, probably because of competitive inhibition of uric acid secretion or a decrease in ECF volume and a secondary increase in uric acid reabsorption.
-
Hypotensive activity in hypertensive patients; also augments the action of other hypotensive agents. Precise mechanism of hypotensive action has not been determined, but postulated that part of this effect is caused by direct arteriolar dilation.
Advice to Patients
-
Advise patient of signs of electrolyte imbalance (e.g., dryness of the mouth, thirst, weakness, lethargy, drowsiness, restlessness, confusion, seizures, oliguria, muscle pains or cramps, muscular fatigue, hypotension, tachycardia, GI disturbances such as nausea and vomiting).
-
Advise patients of importance of compliance with scheduled determinations of serum electrolyte concentrations (particularly potassium, sodium, chloride, and bicarbonate).
-
Advise hypertensive patients of importance of continuing lifestyle/behavioral modifications that include weight reduction (for those who are overweight or obese), dietary changes to include foods that are rich in potassium and calcium and moderately restricted in sodium (adoption of the Dietary Approaches to Stop Hypertension [DASH] eating plan), increased physical activity, smoking cessation, and moderation of alcohol intake.
Advise that lifestyle/behavioral modifications reduce BP, enhance antihypertensive drug efficacy, and decrease cardiovascular risk and remain an indispensable part of the management of hypertension.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
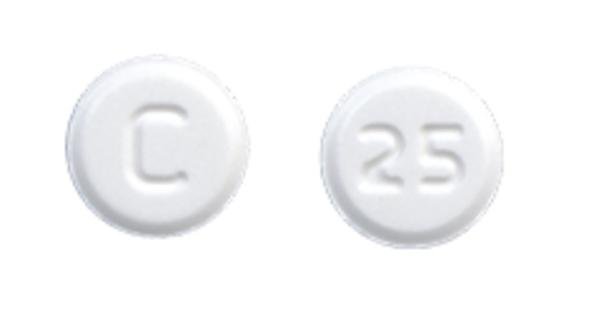
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg* |
Chlorthalidone Tablets |
|
|
50 mg* |
Chlorthalidone Tablets |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
Atenolol 50 mg and Chlorthalidone 25 mg* |
Atenolol and Chlorthalidone Tablets |
|
|
Tenoretic |
AstraZeneca |
|||
|
Atenolol 100 mg and Chlorthalidone 25 mg* |
Atenolol and Chlorthalidone Tablets |
|||
|
Tenoretic |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
More about chlorthalidone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (49)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: thiazide diuretics
- Breastfeeding
- En español