Cabotegravir and Rilpivirine (Monograph)
Brand name: Cabenuva
Drug class: HIV Integrase Inhibitors
Introduction
Cabotegravir, an HIV integrase strand transfer inhibitor (INSTI), and rilpivirine, an HIV non-nucleoside reverse transcriptase inhibitor (NNRTI), are used in combination as an antiretroviral agent.
Uses for Cabotegravir and Rilpivirine
Treatment of HIV Infection
Indicated as a complete regimen for the treatment of HIV-1 infection to replace the current antiretroviral regimen in adults and pediatric patients ≥12 years of age and weighing at least 35 kg who are virologically suppressed (HIV-1 RNA <50 copies per mL) on a stable antiretroviral regimen with no history of treatment failure and with no known or suspected resistance to either drug.
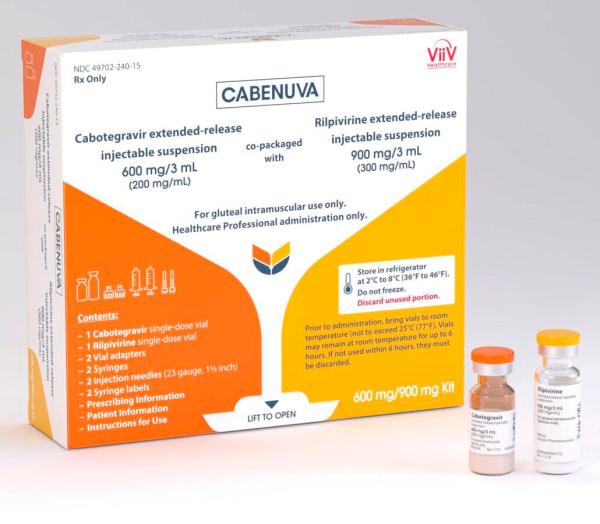
The combination regimen is commercially available as a copackaged product containing cabotegravir extended-release injectable suspension and rilpivirine extended-release injectable suspension.
Therapeutic options for treatment and prevention of HIV infection and recommendations concerning use of antiretrovirals are continuously evolving. Most appropriate antiretroviral regimen cannot be defined for every clinical scenario; select regimen based on antiretroviral potency, potential rate of resistance development, known toxicities, potential for pharmacokinetic interactions, and patient's virologic, immunologic, and clinical characteristics.
Cabotegravir and Rilpivirine Dosage and Administration
General
Pretreatment Screening
-
Carefully select patients who agree to the required monthly or every-2-month IM injection dosing and testing schedules.
Patient Monitoring
-
Periodically monitor liver function tests (i.e., AST, ALT).
-
Assess patient adherence to the prescribed therapy during scheduled dosing visits.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) list of error-prone abbreviations, symbols, and dose designations states that the use of abbreviations for antiretroviral medications (e.g., DOR, TAF, TDF) during the medication use process should be avoided as their use has been associated with serious medication errors.
Administration
Administer by IM injection only.
Commercially available as cabotegravir extended-release injectable suspension in a single-dose vial and rilpivirine extended-release injectable suspension in a single-dose vial copackaged for coadministration by IM injection.
Must administer by gluteal IM injection at separate sites (on opposite sides or at least 2 cm apart) by a healthcare provider during the same visit. Ventrogluteal site is recommended, but a dorsogluteal approach (upper outer quadrant) is acceptable, if preferred by the healthcare professional. Do not administer by any other route or anatomical site.
Consider BMI of the patient to ensure that needle length is sufficient to reach the gluteus muscle. Longer needle lengths may be required for patients with higher BMI (e.g., >30 kg/m2) to ensure that injections are administered IM as opposed to sub-Q. The administration order of the injections is not important.
Combined treatment may be initiated with oral cabotegravir and rilpivirine (oral lead-in daily dose is cabotegravir 30 mg and rilpivirine 25 mg with a meal for approximately 1 month [at least 28 days]) prior to beginning IM injections to assess tolerability or the patient may proceed directly to the injections without an oral lead-in.
Can be administered on a monthly or every 2 months dosing schedule. Discuss these dosing options with the patient prior to starting treatment to determine most appropriate option.
IM Injection
Remove vials from refrigerator and wait at least 15 minutes to allow them to come to room temperature. The vials may remain in the carton at room temperature for up to 6 hours; do not place back into refrigerator. Discard if not used within 6 hours.
Inspect vial contents visually for particulate matter and discoloration prior to administration. The cabotegravir vial has a brown tint to the glass that may limit visual inspection of the suspension. Discard if either vial exhibits particulate matter or discoloration.
Shake each vial vigorously to achieve uniform suspension before use; small air bubbles are expected and acceptable.
Once the drugs are drawn into the respective syringes, administer as soon as possible. Do not place filled syringes in the refrigerator. Discard unused filled syringes and needles after 2 hours.
Dosage
Pediatric Patients
Treatment of HIV Infection in Adolescents ≥12 Years of Age Weighing at Least 35 kg
IM
Prior to initiating treatment with injections, may use oral lead-in dosing regimen for approximately 1 month (at least 28 days) to assess the tolerability.
Monthly Schedule: Initiate injections on the last day of current antiretroviral therapy or oral lead-in, if used. Initiate parenteral regimen with single IM injections of cabotegravir 600 mg and rilpivirine 900 mg. After the initiation injections, the recommended monthly continuation injection doses are a single 400 mg IM injection of cabotegravir and a single 600 mg IM injection of rilpivirine at each visit (see Table 1). Patients may be given injections up to 7 days before or after the date the patient is scheduled to receive monthly injections.
|
Drug |
Oral lead-in for at least 28 days prior to starting injections (Optional) |
IM (Gluteal) Initiation Injections (One-Time Dosing) at Month 1 |
IM (Gluteal) Continuation Injections (Once-Monthly Dosing) after Initiation Injection |
|---|---|---|---|
|
Cabotegravir |
30 mg once daily with a meal |
600 mg |
400 mg |
|
Rilpivirine |
25 mg once daily with a meal |
900 mg |
600 mg |
Every 2 Months Schedule Initiate injections on the last day of current antiretroviral therapy or oral lead-in, if used. The recommended initiation injection doses are a single 600 mg IM injection of cabotegravir and a single 900 mg IM injection of rilpivirine 1 month apart for 2 consecutive months. Patients may be given these injections up to 7 days before or after the date the patient is scheduled to receive the second initiation injections. After the 2 initiation doses given consecutively 1 month apart (Months 1 and 2), the recommended continuation injection doses (Month 4 onwards) are a single 600 mg IM injection of cabotegravir and a single 900 mg IM injection of rilpivirine administered every 2 months (see Table 2). Patients may be given injections up to 7 days before or after the date the patient is scheduled to receive the injections.
|
Drug |
Oral lead-in for at least 28 days prior to starting injections (Optional) |
IM (Gluteal) Continuation Injections at Month 1, Month 2, and then Every 2 Months Onwards (starting at Month 4) |
|---|---|---|
|
Cabotegravir |
30 mg once daily with a meal |
600 mg |
|
Rilpivirine |
25 mg once daily with a meal |
900 mg |
Adults
Treatment of HIV Infection
IM
Prior to initiating treatment with parenteral cabotegravir and rilpivirine, use oral lead-in dosing regimen of cabotegravir and rilpivirine for approximately 1 month (at least 28 days) to assess tolerability.
Continuation injections (monthly): On the last day of oral lead-in dosing regimen, initiate parenteral regimen with single IM injections of cabotegravir 600 mg and rilpivirine 900 mg. After the initiation injections, the recommended monthly continuation injection doses are a single 400 mg IM injection of cabotegravir and a single 600 mg IM injection of rilpivirine at each visit (see Table 1). Patients may be given these injections up to 7 days before or after the date the patient is scheduled to receive monthly injections.
Every 2 Months Schedule Initiate injections on the last day of current antiretroviral therapy or oral lead-in, if used. The recommended initiation injection doses are a single 600 mg IM injection of cabotegravir and a single 900 mg IM injection of rilpivirine 1 month apart for 2 consecutive months. Patients may be given these injections up to 7 days before or after the date the patient is scheduled to receive the second initiation injections. After the 2 initiation doses given consecutively 1 month apart (Months 1 and 2), the recommended continuation injection doses (Month 4 onwards) are a single 600 mg IM injection of cabotegravir and a single 900 mg IM injection of rilpivirine administered every 2 months (see Table 2). Patients may be given these injections up to 7 days before or after the date the patient is scheduled to receive the injections.
Recommended Dosing Schedule for Missed Injections
Monthly Dosing Schedule (Planned Missed Injections): If a patient plans to miss a scheduled injection visit by >7 days, oral cabotegravir in combination with oral rilpivirine may be administered once daily for up to 2 months to replace missed injection visits, or any other fully suppressive oral antiretroviral regimen until injections are resumed. Recommended oral daily dose is cabotegravir 30 mg and rilpivirine 25 mg taken at approximately the same time each day with a meal. The first dose of oral therapy should be taken 1 month (+/-7 days) after the last injection dose and continued until the day injection dosing is restarted. For oral therapy durations >2 months, an alternative oral regimen is recommended.
Monthly Dosing Schedule (Unplanned Missed Injections): If monthly injections are missed or delayed by >7 days and oral therapy has not been taken in the interim, clinically reassess the patient to determine if resumption of injection dosing remains appropriate. If injection dosing will be continued, see Table 3 for dosing recommendations.
|
Time since Last Injection |
Recommendation |
|---|---|
|
≤2 months |
Resume with 400 mg cabotegravir and 600 mg rilpivirine IM monthly injections as soon as possible. |
|
>2 months |
Re-initiate the patient with 600 mg cabotegravir and 900 mg rilpivirine IM injections then continue to follow the 400 mg cabotegravir and 600 mg rilpivirine IM monthly injection dosing schedule. |
Every 2 Months Schedule (Planned Missed Injections) If a patient plans to miss a scheduled injection visit by >7 days, oral cabotegravir in combination with oral rilpivirine once daily may be administered for up to 2 months to replace 1 missed injection visit, or any other fully suppressive oral antiretroviral regimen may be used until injections are resumed. The recommended oral daily dose is cabotegravir 30 mg and rilpivirine 25 mg, administered at approximately the same time each day with a meal. The first dose of oral therapy should be taken approximately 2 months after the last injection dose and continued until the day injection dosing is restarted. Refer to Table 4 for injection dosing recommendations. For oral therapy durations greater than 2 months, an alternative oral regimen is recommended.
Every-2-Month Schedule (Unplanned Missed Injections): If a scheduled every 2 months injection visit is missed or delayed by >7 days and oral therapy has not been taken in the interim, clinically reassess the patient to determine if resumption of injection dosing remains appropriate. If the every 2 month dosing schedule will be continued, see Table 4 for dosing recommendations
|
Missed Injection (Visit) |
Time since Last Injection |
Recommendation |
|---|---|---|
|
Injection 2 (Month 2) |
≤2 months |
Resume with 600 mg cabotegravir and 900 mg rilpivirine IM injections as soon as possible, then continue to follow the every 2 month injection dosing schedule. |
|
Injection 2 (Month 2) |
>2 months |
Re-initiate the patient with 600 mg cabotegravir and 900 mg rilpivirine IM injections, followed by the second initiation injection dose 1 month later. Then continue to follow the every 2 month injection dosing schedule thereafter. |
|
Injection 3 or later (Month 4 onwards) |
≤3 months |
Resume with 600 mg cabotegravir and 900 mg rilpivirine IM injections as soon as possible and continue with the every 2 month injection dosing schedule. |
|
Injection 3 or later (Month 4 onwards) |
>3 months |
Re-initiate the patient with 600-mg cabotegravir and 900-mg rilpivirine IM injections, followed by the second initiation injection dose 1 month later. Then continue with the every 2 month injection dosing schedule thereafter. |
Transitioning between Monthly and Every 2 Month Schedules
Patients switching from a monthly continuation injection schedule to an every 2 months continuation injection dosing schedule should receive a single 600-mg IM injection of cabotegravir and a single 900-mg IM injection of rilpivirine administered 1 month after the last monthly continuation injections and then every 2 months thereafter.
Patients switching from an every 2 months continuation injection schedule to a monthly continuation dosing schedule should receive a single 400 mg IM injection of cabotegravir and a single 600 mg IM injection of rilpivirine 2 months after the last every 2 months continuation injection and then monthly thereafter.
Special Populations
Hepatic Impairment
Dosage adjustment not necessary for patients with mild or moderate hepatic impairment (Child-Pugh A or B). Effect of severe hepatic impairment (Child-Pugh C) on pharmacokinetics of cabotegravir or rilpivirine unknown.
Renal Impairment
Dosage adjustment not necessary for patients with mild (Clcr 60 to <90 mL/minute) or moderate (Clcr30 to <60 mL/minute) renal impairment. Increase monitoring for adverse effects in patients with severe renal impairment (Clcr 15 to <30 mL/minute) or end-stage renal disease (Clcr <15 mL/minute). In patients with end-stage renal disease not on dialysis, effects on the pharmacokinetics are unknown. Dialysis not expected to alter exposures of cabotegravir or rilpivirine.
Geriatric Use
Exercise caution when using the drug in elderly patients.
Cautions for Cabotegravir and Rilpivirine
Contraindications
-
Previous hypersensitivity reaction to cabotegravir or rilpivirine.
-
Coadministration with drugs for which significant decreases in cabotegravir plasma concentrations may occur due to uridine diphosphate glucuronosyl transferase (UGT)1A1 enzyme induction and/or CYP3A enzyme induction, which may result in loss of virologic response (e.g., anticonvulsants [carbamazepine, oxcarbazepine, phenobarbital, phenytoin], antimycobacterials [rifampin, rifabutin, rifapentine], systemic glucocorticoids [dexamethasone; more than a single dose treatment], and herbal products [St. John's wort]).
Warnings/Precautions
Hypersensitivity Reactions
Serious or severe hypersensitivity reactions, including cases of drug reaction with eosinophilia and systemic symptoms (DRESS), Stevens-Johnson syndrome, and toxic epidermal necrolysis reported. While some skin reactions were accompanied by constitutional symptoms such as fever, other skin reactions were associated with organ dysfunctions, including elevations in hepatic serum biochemistries. Administration of oral lead-in dosing was used in clinical studies to help identify patients who may be at risk of a hypersensitivity reaction.
Discontinue immediately if signs or symptoms of hypersensitivity reactions develop (including, but not limited to, severe rash, or rash accompanied by fever, general malaise, fatigue, muscle or joint aches, blisters, mucosal involvement [oral blisters or lesions], conjunctivitis, facial edema, hepatitis, eosinophilia, angioedema, difficulty breathing). Monitor clinical status and perform hepatic function tests as clinically indicated; initiate appropriate therapy as indicated.
Post-injection Reactions
Serious post-injection reactions reported in clinical studies within minutes after the injection of rilpivirine. These events included symptoms such as dyspnea, bronchospasm, agitation, abdominal cramping, rash/urticaria, dizziness, flushing, sweating, oral numbness, changes in blood pressure, and pain (e.g., back and chest). Events reported in <1% of subjects and began to resolve within minutes after the injection, with some patients receiving supportive care. Events may have been associated with accidental IV administration during the IM injection procedure.
Carefully follow instructions for preparation and administration of the injections. Inject the suspensions slowly via IM injection, and take care to avoid accidental IV administration. Observe patients briefly (approximately 10 minutes) after the injection. If a patient experiences a post-injection reaction, monitor and treat as clinically indicated.
Hepatotoxicity
Hepatotoxicity has been reported in patients with or without known pre-existing hepatic disease or identifiable risk factors. Patients with underlying liver disease or marked elevations in transaminases prior to treatment may be at increased risk for worsening or development of transaminase elevations.
Monitor liver chemistries and discontinue treatment if hepatotoxicity is suspected.
Depressive Disorders
Depressive disorders (including depressed mood, depression, major depression, mood altered, mood swings, dysphoria, negative thoughts, suicidal ideation or attempt) reported with combination therapy or the individual drug products. Promptly evaluate symptoms to assess if related to cabotegravir and rilpivirine and to determine whether risks of continued therapy outweigh benefits.
Risk of Adverse Reactions or Loss of Virologic Response due to Drug Interactions
Concomitant use with other drugs may result in known or potentially significant drug interactions, some of which may lead to adverse events, loss of virologic response, and possible development of viral resistance.
Use with caution in combination with drugs with a known risk of torsade de pointes.
Long-acting Properties and Potential Associated Risks with Cabotegravir and Rilpivirine
Residual concentrations of both drugs may remain in the systemic circulation of patients for prolonged periods (up to ≥12 months) after administration of the injection.
Carefully select patients who agree to the required monthly or every-2-month injection dosing schedule because non-adherence or missed doses could lead to loss of virologic response and development of resistance.
Initiate an alternative, fully suppressive antiretroviral regimen no later than 1 month after the final injections when dosed monthly and no later than 2 months after the final injections when dosed every 2 months. If virologic failure is suspected, switch the patient to an alternative regimen as soon as possible.
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry at 800-258-4263 or [Web].
Data insufficient to adequately assess a drug-associated risk of birth defects and miscarriage. Discuss the risks and benefits of using cabotegravir and rilpivirine with individuals of childbearing potential or during pregnancy.
The Health and Human Services Panel on Treatment of Pregnant Women with HIV Infection and Prevention of Perinatal Transmission states data are not available regarding use of cabotegravir for the treatment of HIV-1 infection during pregnancy and, therefore is not recommended as a complete treatment regimen in pregnant females or females of reproductive potential trying to conceive. The Panel recommends that pregnant individuals who present to care on this regimen should be switched to an appropriate 3-drug antiretroviral regimen recommended for use in pregnancy.
Lower exposures with oral rilpivirine observed during pregnancy. Monitor viral load closely during pregnancy. Cabotegravir and rilpivirine are detected in systemic circulation for up to ≥12 months after discontinuing extended-release injections; therefore, give consideration to the potential for fetal exposure during pregnancy.
Lactation
Rilpivirine is present in human milk. No data on the presence of cabotegravir in human milk; however, it is present in animal milk. When a drug is present in animal milk, it is likely present in human milk. If cabotegravir and/or rilpivirine are present in human milk, residual exposures may remain for ≥12 months after administration of the last extended-release injections. Unknown if cabotegravir and rilpivirine affect milk production or have effects on breastfed infant.
The HHS perinatal HIV transmission guideline provides updated recommendations on infant feeding. The guideline states that patients with HIV should receive evidence-based, patient-centered counseling to support shared decision making about infant feeding. During counseling, patients should be informed that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates the risk of postnatal HIV transmission to the infant. Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces the risk of breastfeeding HIV transmission to <1%, but does not completely eliminate the risk. Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.
Pediatric Use
Safety and effectiveness established in pediatric patients ≥12 years of age and weighing at least 35 kg.
Safety, efficacy, and pharmacokinetics not established in pediatric patients <12 years of age or weighing <35 kg.
Geriatric Use
Clinical trials did not include sufficient numbers of patients ≥65 years of age to determine whether they respond differently from younger subjects. Elderly patients may have greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Hepatic Impairment
No dosage adjustment is necessary with mild or moderate hepatic impairment (Child-Pugh A or B). Unknown effects of severe hepatic impairment (Child-Pugh C).
Renal Impairment
No dosage adjustment necessary for mild (Clcr ≥60 to <90 mL/minute) or moderate (Clcr ≥30 to <60 mL/minute) renal impairment. Increase monitoring in patients with severe renal impairment (Clcr 15 to <30 mL/minute) or end-stage renal disease (Clcr <15 mL/minute). Unknown effects in end-stage renal disease not on dialysis. Dialysis is not expected to alter exposures since >99% protein bound.
Common Adverse Effects
Common adverse reactions (≥2%): injection site reactions, pyrexia, fatigue, headache, musculoskeletal pain, nausea, sleep disorders, dizziness, rash.
Drug Interactions
Cabotegravir is metabolized primarily by uridine diphosphate-glucuronosyltransferase (UGT) 1A1, with minor metabolism by UGT1A9. Rilpivirine is metabolized principally by CYP 3A enzymes.
Concomitant Use with Other Antiretroviral Medicines
Because cabotegravir and rilpivirine is a complete regimen, coadministration with other antiretroviral medications for the treatment of HIV-1 infection is not recommended.
Use of Other Antiretroviral Drugs after Discontinuation of Long-Acting Cabotegravir and Rilpivirine Injection
Residual concentrations may remain in the systemic circulation of patients for ≥12 months. Residual concentrations are not expected to affect the exposures of antiretroviral drugs initiated after discontinuation of cabotegravir/rilpivirine.
Drugs Affecting or Metabolized by Uridine Diphosphate-glucuronosyltransferases (UGT)
Drugs that are strong inducers of UGT1A1 or UGT1A9 are expected to decrease cabotegravir plasma concentrations and may result in loss of virologic response; therefore, coadministration with these drugs is contraindicated.
Drugs Affecting or Metabolized by CYP3A
Drugs that induce CYP3A may result in decreased plasma concentrations of rilpivirine and loss of virologic response and possible resistance to rilpivirine or to the class of NNRTIs. Coadministration of the combined injection and drugs that inhibit CYP3A may result in increased plasma concentrations of rilpivirine; therefore, coadministration with these drugs is contraindicated. .
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticonvulsants (carbamazepine, oxcarbazepine, phenobarbital, or phenytoin) |
Coadministration may cause significant decreases in cabotegravir and rilpivirine plasma concentrations due to UGT1A1 and CYP3A enzyme induction, which may result in loss of virologic response. |
Concomitant use is contraindicated |
|
Antimycobacterials rifampin, rifabutin, or rifapentine) |
Coadministration may cause significant decreases in cabotegravir and rilpivirine plasma concentrations due to UGT1A1 and CYP3A enzyme induction, which may result in loss of virologic response. |
Concomitant use is contraindicated |
|
Glucocorticoid (systemic) |
Coadministration with systemic glucocorticoids such as dexamethasone for more than a single-dose treatment may cause significant decrease in rilpivirine plasma concentrations due to CYP3A enzyme induction, which may result in loss of virologic response. |
Concomitant use is contraindicated |
|
Macrolide antibiotics (clarithromycin, erythromycin) |
Coadministration is expected to increase concentrations of rilpivirine and are associated with a risk of torsade de pointes. |
Consider therapeutic alternatives, such as azithromycin, which increase rilpivirine concentrations less than other macrolides |
|
Methadone |
Coadministration may decrease methadone concentrations. |
No dose adjustment of methadone is required when starting coadministration, but clinical monitoring is recommended as methadone maintenance therapy may need to be adjusted in some patients |
|
QT-Prolonging Drugs |
Rilpivirine may prolong the QTc interval. |
Coadministration of the combined regimen should be used with caution in combination with drugs with a known risk of torsade de pointes |
|
St. John's Wort (Hypericum perforatum) |
Concomitant use may result in substantially decreased rilpivirine concentrations due to potent CYP3A induction by St. John's wort, which may lead to loss of virologic response and possible resistance to rilpivirine or to the class of NNRTIs. |
Concomitant use is contraindicated |
Cabotegravir and Rilpivirine Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations of cabotegravir and rilpivirine occur approximately 7 and 3-4 days, respectively, after the injected dose.
Cabotegravir: Peak plasma concentrations similar between monthly and every 2-month injection schedule.
Rilpivirine: Peak plasma concentrations similar between monthly and every 2-month injection schedule.
Special Populations
Renal Impairment: No clinically significant pharmacokinetic differences of cabotegravir in patients with mild, moderate, or severe renal impairment; not studied in patients with end-stage renal disease not on dialysis. Oral rilpivirine population pharmacokinetic analyses indicated that mild renal impairment had no clinically relevant effect; limited or no information regarding pharmacokinetics in patients with moderate or severe renal impairment or end-stage renal disease not on dialysis.
Hepatic Impairment: No clinically significant pharmacokinetic differences of cabotegravir are expected in mild to moderate (Child-Pugh A or B) hepatic impairment; effect of severe hepatic impairment (Child-Pugh C) not studied. No clinically significant pharmacokinetic differences of rilpivirine were observed in mild to moderate (Child-Pugh A or B) hepatic impairment; effect of severe hepatic impairment (Child-Pugh C) not studied.
Geriatric Patients: Pharmacokinetics of cabotegravir (oral or injectable) and of injectable rilpivirine not studied.
Pediatric Patients: No clinically relevant differences in exposure between HIV-1–infected adolescents and HIV-1–infected and uninfected adult participants from the cabotegravir or rilpivirine development program.
Distribution
Plasma Protein Binding
Cabotegravir: >99.8%.
Rilpivirine: 99.7%.
Elimination
Metabolism
Cabotegravir: Metabolized primarily by UGT 1A1, with some minor metabolism by UGT1A9.
Rilpivirine: Metabolized principally by CYP3A.
Half-life
Cabotegravir: 5.6–11.5 weeks respectively; driven by slow absorption rate from the IM injection site.
Rilpivirine: 13–28 weeks; driven by slow absorption rate from the IM injection site.
Stability
Storage
Parenteral
Extended-release injection, for IM use
Store dosing kits at 2–8°C in the original carton until ready to use; do not freeze.
Actions and Spectrum
-
Contains 2 long-acting HIV-1 antiretroviral drugs, cabotegravir and rilpivirine.
-
Cabotegravir is a HIV integrase strand transfer inhibitor (INSTI) and inhibits HIV integrase by binding to the integrase active site and blocking the strand transfer step of retroviral DNA integration, which is essential for the HIV replication cycle.
-
Rilpivirine is a diarylpyrimidine NNRTI of HIV-1 and inhibits HIV-1 replication by non-competitive inhibition of HIV-1 reverse transcriptase.
-
Cabotegravir- and rilpivirine-resistant HIV-1 has been produced in vitro and has also emerged during combined therapy. Virologic failures reported.
-
Cross-resistance between cabotegravir plus rilpivirine to other INSTIs and NNRTIs has been reported.
Advice to Patients
-
Advise patients to immediately contact their healthcare provider if they develop a rash after receiving the combined regimen. Instruct patients to not receive further doses and to immediately seek medical attention if they develop a rash associated with any of the following symptoms, as it may be a sign of a more serious reaction such as DRESS or severe hypersensitivity: fever; generally ill feeling; extreme tiredness; muscle or joint aches; blisters; oral blisters or lesions; eye inflammation; facial swelling; swelling of the eyes, lips, tongue, or mouth; difficulty breathing; and/or signs and symptoms of liver problems (e.g., yellowing of the skin or whites of the eyes; dark or tea-colored urine; pale-colored stools or bowel movements; nausea; vomiting; loss of appetite; or pain, aching, or sensitivity on the right side below the ribs).
-
Advise patients that injection site reactions have been reported in the majority of patients receiving the combined regimen. These reactions typically consist of one or more of the following: pain, erythema, tenderness, pruritus, and local swelling. Systemic reactions have also been reported, such as fever, musculoskeletal pain, and sciatica pain. Serious post-injection reactions also were reported within minutes after the injection of rilpivirine, including dyspnea, bronchospasm, agitation, abdominal cramping, rash/urticaria, dizziness, flushing, sweating, oral numbness, changes in blood pressure, and back pain (e.g., back and chest). Advise patients that they will be observed briefly (approximately 10 minutes) after the injection.
-
Inform patients that hepatotoxicity has been reported. Inform patients that monitoring for liver transaminases is recommended.
-
Advise patients that depressive disorders (including depressed mood, depression, major depression, mood altered, mood swings, unusual mood, feeling tense, negative thoughts, suicidal ideation or attempt) have been reported with at least one of the components of the combined regimen. Instruct patients to seek prompt medical evaluation if they experience depressive symptoms.
-
Instruct patients about the importance of continued medication adherence and scheduled visits to help maintain viral suppression and to reduce risk of loss of virologic response and development of resistance.
-
Advise patients that the combined regimen can be injected monthly or every 2 months after oral lead-in with cabotegravir and rilpivirine to assess tolerability. Discuss the two injection dosing frequency options with patients prior to starting this medication regimen and decide which injection dosing frequency would be the most appropriate option.
-
Inform patients that cabotegravir and rilpivirine can remain in the body for up to >12 months after receiving their last extended-release injections. Advise patients that they should contact their healthcare provider if they miss or plan to miss a scheduled injection visit and that oral therapy with cabotegravir and rilpivirine may be used up to 2 months to replace missed injection visits, or any other fully suppressive oral antiretroviral regimen may be used until injections are resumed. Advise patients that if they stop treatment with the combined regimen of cabotegravir and rilpivirine extended-release injection, they will need to take other medicines to treat their HIV-1 infection.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements (e.g., St. John's wort), as well as any concomitant illnesses. The combined regimen of cabotegravir and rilpivirine extended-release injection may be systemically present for ≥12 months. These residual concentrations are not expected to affect the exposures of other antiretroviral drugs that are initiated after discontinuation of this medication.
-
Advise patients to inform clinicians if they are or plan to become pregnant. Inform patients that there is an antiretroviral pregnancy registry to monitor fetal outcomes in those exposed to the combined regimen of cabotegravir and rilpivirine extended-release injection during pregnancy. Patients who are of reproductive potential should be informed of the long duration of exposure of the combined regimen of cabotegravir and rilpivirine extended-release injection and that there is very limited clinical experience in human pregnancy.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Kit |
Cabotegravir 200 mg/mL (400 mg) and rilpivirine 300 mg/mL (600 mg) Each kit contains 1 single-dose vial of cabotegravir extended-release injectable suspension and 1 single-dose vial of rilpivirine extended-release injectable suspension |
Cabenuva 400 mg/600 mg |
ViiV Healthcare Company |
|
Cabotegravir 200 mg/mL (600 mg) and rilpivirine 300 mg/mL (900 mg) Each kit contains 1 single-dose vial of cabotegravir extended-release injectable suspension and 1 single-dose vial of rilpivirine extended-release injectable suspension |
Cabenuva 600 mg/900 mg |
ViiV Healthcare Company |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions September 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about cabotegravir / rilpivirine
- Check interactions
- Compare alternatives
- Reviews (29)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antiviral combinations
- En español