Acarbose (Monograph)
Drug class: alpha-Glucosidase Inhibitors
VA class: HS502
Chemical name: O-4,6-dideoxy-4-[[[1S-(1α,4α,5β,6α)]-4,5,6-trihydroxy-3-(hydroxymethyl)-2-cyclohexen-1-yl]amino]-α-d -glucopyranosyl-(1→4)-O-α-d-glucopyranosyl-(1→4)-d-glucose
Molecular formula: C25H43NO18
CAS number: 56180-94-0
Introduction
Antidiabetic agent; an α-glucosidase inhibitor.
Uses for Acarbose
Type 2 Diabetes Mellitus
Used as monotherapy as an adjunct to diet and exercise for the management of type 2 diabetes mellitus in patients whose hyperglycemia cannot be controlled by diet and exercise alone.
Also used as adjunct to diet and exercise in combination with metformin, a sulfonylurea, or insulin for management of type 2 diabetes mellitus in patients whose hyperglycemia cannot be controlled with monotherapy with these agents, diet, and exercise.
Current guidelines for the treatment of type 2 diabetes mellitus generally recommend metformin as first-line therapy in addition to lifestyle modifications in patients with recent-onset type 2 diabetes mellitus or mild hyperglycemia because of its well-established safety and efficacy (i.e., beneficial effects on glycosylated hemoglobin [hemoglobin A1c; HbA1c], weight, and cardiovascular mortality).
In patients with metformin contraindications or intolerance (e.g., risk of lactic acidosis, GI intolerance) or in selected other patients, some experts suggest that initial therapy with a drug from another class of antidiabetic agents (e.g., a glucagon-like peptide-1 [GLP-1] receptor agonist, sodium-glucose cotransporter 2 [SGLT2] inhibitor, dipeptidyl peptidase-4 [DPP-4] inhibitor, sulfonylurea, thiazolidinedione, basal insulin) may be acceptable based on patient factors.
May need to initiate therapy with 2 agents (e.g., metformin plus another drug) in patients with high initial HbA1c (>7.5% or ≥1.5% above target). In such patients with metformin intolerance, some experts suggest initiation of therapy with 2 drugs from other antidiabetic drug classes with complementary mechanisms of action.
An α-glucosidase inhibitor (acarbose, miglitol) generally not recommended as second-line therapy after failure of metformin monotherapy because of comparatively lesser efficacy, frequent adverse GI effects, and greater cost, but may be appropriate therapy in selected patients.
Consider early initiation of combination therapy for the treatment of type 2 diabetes mellitus to extend the time to treatment failure and more rapidly attain glycemic goals.
For patients with inadequate glycemic control on metformin monotherapy, consider patient comorbidities (e.g., atherosclerotic cardiovascular disease [ASCVD], established kidney disease, heart failure), hypoglycemia risk, impact on weight, cost, risk of adverse effects, and patient preferences when selecting additional antidiabetic agents for combination therapy.
Consider early introduction of insulin for severe hyperglycemia (e.g., blood glucose ≥300 mg/dL or HbA1c >9–10%), especially if accompanied by catabolic manifestations (e.g., weight loss, hypertriglyceridemia, ketosis) or symptoms of hyperglycemia.
Acarbose Dosage and Administration
General
-
Individualize treatment and adjust target blood glucose and HbA1c concentrations based on patient’s understanding and adherence to the treatment regimen, the risk of severe hypoglycemia, and other factors that may increase risk or decrease benefit (e.g., very young or old age, comorbid conditions, other diseases that materially shorten life expectancy).
-
Goal of therapy is to reduce both postprandial blood (or plasma) glucose and hemoglobin values to normal or near normal using lowest effective dosage of acarbose as monotherapy or combined with a sulfonylurea antidiabetic agent, metformin, or insulin. During therapy initiation and dosage titration, obtain 1-hour postprandial glucose concentration to determine therapeutic response and minimum effective dosage. Monitor HbA1c values at approximately every 3 months to evaluate long-term glycemic control. Monitor glucose concentrations 1–2 hours after the start of a meal in those who have elevated HbA1c despite adequate preprandial glucose concentrations.
Administration
Oral Administration
Administer orally at the beginning (with the first bite) of each main meal.
To minimize adverse GI effects, closely follow diabetic diet as prescribed. (See Adherence to Prescribed Diet under Cautions.)
Dosage
Adults
Type 2 Diabetes Mellitus
Oral
Initially, 25 mg at the beginning of each main meal (with first bite) 3 times daily. In patients with adverse GI effects, initiate at 25 mg once daily and increase dosage gradually as necessary to 25 mg 3 times daily.
Once dosage of 25 mg 3 times daily has been reached, increase dosage at intervals of 4–8 weeks as tolerated to achieve the desired 1-hour postprandial glucose concentration (i.e., <180 mg/dL) or until maximum dosage (according to weight) is reached. (See Prescribing Limits under Dosage and Administration.) Maintenance dosage ranges from 50–100 mg 3 times daily.
Dosages higher than 100 mg 3 times daily are not recommended since such dosages have been associated with an increased risk of elevated serum aminotransferase concentrations. If no further therapeutic benefit occurs at the maximum recommended dosage, consider lowering the dosage.
Prescribing Limits
Adults
Type 2 Diabetes Mellitus
Oral
Patients ≤60 kg: maximum 50 mg 3 times daily.
Patients >60 kg: maximum 100 mg 3 times daily.
Cautions for Acarbose
Contraindications
-
Known hypersensitivity to the drug.
-
Diabetic ketoacidosis.
-
Cirrhosis.
-
Inflammatory bowel disease, colonic ulceration, existing partial intestinal obstruction or predisposition to this condition.
-
Chronic intestinal diseases associated with marked disorders of digestion or absorption.
-
Co-existing conditions that may deteriorate as a result of increased intestinal gas formation.
Warnings/Precautions
General Precautions
Metabolic Effects
Should not cause hypoglycemia when administered alone in the fasted or postprandial state. However, hypoglycemia (rarely hypoglycemic shock) may occur when used concomitantly with a sulfonylurea antidiabetic agent and/or insulin. If hypoglycemia occurs, adjust dosage of these agents appropriately. Use oral glucose (dextrose) for the treatment of mild to moderate hypoglycemia instead of sucrose (table sugar); the absorption of oral glucose is not inhibited by acarbose. Severe hypoglycemia may require the use of either IV glucose or parenteral glucagon.
Insulin may be required for correction of temporary hyperglycemia that is not controlled by dietary regulation or oral antidiabetic agents during periods of severe stress (e.g., acute infection, trauma, surgery, fever).
Hepatic Effects
Elevations in serum aminotransferase (i.e., ALT, AST) concentrations and, in rare instances, hyperbilirubinemia may occur, particularly with dosages exceeding 150 mg daily (50 mg 3 times daily). Jaundice and fatal hepatitis reported during postmarketing experience.
Determine serum aminotransferase concentrations every 3 months during the first year of therapy and periodically thereafter. If elevations in serum aminotransferase concentrations occur, reduce dosage. May be necessary to withdraw the drug, particularly if elevated serum aminotransferase concentrations persist.
Adherence to Prescribed Diet
If prescribed diet not followed closely, adverse GI effects may be intensified. If symptoms are strongly distressing despite adherence to prescribed diabetic diet, temporarily or permanently reduce acarbose dosage.
Specific Populations
Pregnancy
Category B.
Lactation
Distributed into milk in rats. Not known whether distributed into human milk. Use not recommended in nursing women.
Pediatric Use
Safety and efficacy in children <18 years of age not established.
Geriatric Use
Safety and efficacy in those ≥65 years of age similar to that in younger adults. (See Special Populations under Pharmacokinetics: Absorption.)
Hepatic Impairment
Contraindicated in patients with cirrhosis. Not studied in other conditions associated with hepatic impairment.
Renal Impairment
Not recommended for use in diabetic patients with appreciable renal impairment (Scr >2 mg/dL).
Common Adverse Effects
Flatulence, diarrhea, abdominal discomfort/pain.
Digestive Enzyme Supplements
Possible reduction in the glycemic effects of acarbose. Avoid concomitant use.
Intestinal Adsorbents
Possible reduction in the glycemic effects of acarbose. Avoid concomitant use.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
1,5-Anhydroglucitol assay |
Unreliable results in patients taking acarbose |
Manufacturer recommends use of alternative method to monitor glycemic control |
|
Amylase (digestive enzyme preparation) |
Possible reduction in glycemic effects of acarbose |
Avoid concomitant use |
|
Calcium-channel blocking agents |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control No effect of acarbose on the pharmacokinetic or pharmacodynamics of nifedipine |
Monitor for loss of glycemic control When calcium-channel blocking agents are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia |
|
Charcoal (intestinal adsorbent) |
Possible reduction in glycemic effects of acarbose |
Avoid concomitant use |
|
Corticosteroids |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When corticosteroids are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia |
|
Contraceptives, oral |
Potential exacerbation of hyperglycemia/loss of glycemic control |
Monitor for loss of glycemic control When oral contraceptives are withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia |
|
Digoxin |
Decreased blood concentrations of digoxin |
May require increased digoxin dosage |
|
Diuretics (e.g., thiazides) |
Potential exacerbation of hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When diuretics are withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia |
|
Estrogens |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When estrogens are withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia |
|
Glyburide |
No effect on absorption or disposition of concomitant glyburide |
Pharmacokinetic interaction with glyburide unlikely |
|
Insulin |
Increased risk of hypoglycemia, rarely hypoglycemic shock, with concomitant insulin |
If hypoglycemia occurs, reduce insulin dosage |
|
Isoniazid |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When isoniazid is withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia |
|
Metformin |
Possible decreased peak plasma concentration of metformin |
Pharmacokinetic interaction not considered clinically important |
|
Nicotinic acid |
Potential to exacerbate diabetes mellitus, resulting in loss of glycemic control |
Monitor for loss of glycemic control When nicotinic acid is withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia |
|
Pancreatin (digestive enzyme preparation; no longer commercially available in the US) |
Possible reduction in glycemic effects of acarbose |
Avoid concomitant use |
|
Phenothiazines |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When phenothiazines are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia |
|
Phenytoin |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When phenytoin is withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia |
|
Pramlintide |
Delayed gastric emptying caused by α-glucosidase inhibitors may alter effects of pramlintide on GI absorption of nutrients |
Avoid concomitant pramlintide; safety/efficacy of combination therapy not established |
|
Propranolol |
Pharmacokinetic or pharmacodynamic interaction unlikely |
|
|
Ranitidine |
Pharmacokinetic or pharmacodynamic interaction unlikely |
|
|
Rosiglitazone |
Reduced extent of absorption and prolonged half-life of rosiglitazone Potential for altered glycemic control is uncertain |
Pharmacokinetic interaction not considered clinically important |
|
Sulfonylureas |
Increased risk of hypoglycemia, hypoglycemic shock with sulfonylureas |
If hypoglycemia occurs, reduce sulfonylurea dosage |
|
Sympathomimetic agents |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When sympathomimetic agents are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia. |
|
Thyroid agents |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control |
Monitor for loss of glycemic control When thyroid agents are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia |
Acarbose Pharmacokinetics
Absorption
Bioavailability
Low systemic bioavailability of parent compound; <2% of dose is absorbed as active drug (parent compound and active metabolite). Peak plasma concentrations of active drug attained at approximately 1 hour. Approximately 34% of dose absorbed as numerous metabolites.
Onset
Satisfactory control of blood glucose concentrations achieved within a few days after dosage adjustment; however maximum response may be delayed for up to 2 weeks.
Special Populations
In geriatric patients, mean AUC and peak blood concentrations of the drug were higher compared with younger adults; differences not statistically significant.
In individuals with severe renal impairment (CLcr <25 mL/minute), peak plasma drug concentrations and AUC increased compared with those values in individuals with normal renal function.
Distribution
Extent
Distributed into milk in rats.
Elimination
Metabolism
Metabolized exclusively in GI tract, principally by intestinal bacteria but also by digestive enzymes to numerous metabolites, one of which is active.
Elimination Route
Excreted principally in feces (51% of dose) as unabsorbed drug and in urine as metabolites (34% of dose). No accumulation with recommended dosing frequency.
Half-life
Approximately 2 hours.
Stability
Storage
Oral
Tablets
≤25°C. Protect from moisture.
Actions
-
Small inhibitory effect on α-glucosidase enzymes (e.g., glucoamylase, sucrase, maltase, isomaltase) that hydrolyze oligosaccharides, trisaccharides, and disaccharides to glucose and other monosaccharides in the intestinal brush-border. Small inhibitory effect on pancreatic α-amylase, which hydrolyzes starch into maltose, maltotriose, and dextrins in the lumen of the small intestine. No inhibitory effect on lactase and would not be expected to produce lactose intolerance.
-
Delays carbohydrate breakdown and glucose absorption and reduces postprandial hyperglycemia in diabetic patients.
-
Reduces fluctuations in the daily blood glucose concentration-time profile in patients with type 2 diabetes mellitus and in lean or obese nondiabetic individuals. Fasting blood glucose concentrations either not affected or mildly decreased.
-
In contrast to sulfonylurea antidiabetic agents, acarbose does not enhance insulin secretion. Does not produce hypoglycemia when given as monotherapy in fasting individuals.
-
When used in combination with sulfonylurea antidiabetic agents are used in combination, acarbose reduces the insulinotropic and weight-increasing effects of sulfonylureas. No clinically important loss of calories or weight loss occurs in either diabetic or nondiabetic individuals.
Advice to Patients
-
Importance of adherence to diet and exercise regimen.
-
Importance of adherence to dietary precautions designed to minimize adverse GI effects. Importance of consulting a clinician for dosage adjustments if adverse GI effects occur despite adherence to such dietary precautions. (See Adherence to Prescribed Diet under Cautions.)
-
Importance of regular monitoring of blood glucose concentrations.
-
Importance of avoiding infection.
-
Provide instruction on the management of hyperglycemia or hypoglycemia. Advise of the risk of hypoglycemia, its symptoms, and conditions that predispose to the development of hypoglycemia. Importance of keeping a readily available source of glucose (dextrose) to treat symptoms of hypoglycemia when used in combination with a sulfonylurea agent or insulin.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
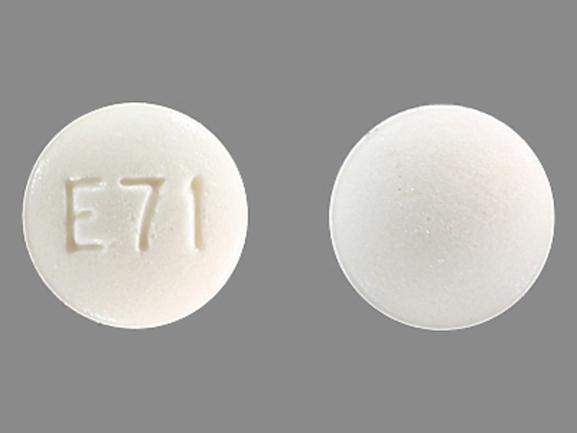
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg* |
Acarbose Tablets |
|
|
50 mg* |
Acarbose Tablets |
|||
|
100 mg* |
Acarbose Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 21, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about acarbose
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (4)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: alpha-glucosidase inhibitors
- Breastfeeding
- En español