Acarbose (Monograph)
Drug class: alpha-Glucosidase Inhibitors
VA class: HS502
Chemical name: O-4,6-dideoxy-4-[[[1S-(1α,4α,5β,6α)]-4,5,6-trihydroxy-3-(hydroxymethyl)-2-cyclohexen-1-yl]amino]-α-d -glucopyranosyl-(1→4)-O-α-d-glucopyranosyl-(1→4)-d-glucose
Molecular formula: C25H43NO18
CAS number: 56180-94-0
Introduction
Antidiabetic agent; an α-glucosidase inhibitor.1 6 30 52
Uses for Acarbose
Type 2 Diabetes Mellitus
Used as monotherapy as an adjunct to diet and exercise for the management of type 2 diabetes mellitus in patients whose hyperglycemia cannot be controlled by diet and exercise alone.1 6 14 47
Also used as adjunct to diet and exercise in combination with metformin, a sulfonylurea, or insulin for management of type 2 diabetes mellitus in patients whose hyperglycemia cannot be controlled with monotherapy with these agents, diet, and exercise.1 3 6 14 23 26 44 47
Current guidelines for the treatment of type 2 diabetes mellitus generally recommend metformin as first-line therapy in addition to lifestyle modifications in patients with recent-onset type 2 diabetes mellitus or mild hyperglycemia because of its well-established safety and efficacy (i.e., beneficial effects on glycosylated hemoglobin [hemoglobin A1c; HbA1c], weight, and cardiovascular mortality).698 704 705
In patients with metformin contraindications or intolerance (e.g., risk of lactic acidosis, GI intolerance) or in selected other patients, some experts suggest that initial therapy with a drug from another class of antidiabetic agents (e.g., a glucagon-like peptide-1 [GLP-1] receptor agonist, sodium-glucose cotransporter 2 [SGLT2] inhibitor, dipeptidyl peptidase-4 [DPP-4] inhibitor, sulfonylurea, thiazolidinedione, basal insulin) may be acceptable based on patient factors.698 704
May need to initiate therapy with 2 agents (e.g., metformin plus another drug) in patients with high initial HbA1c (>7.5% or ≥1.5% above target).698 704 In such patients with metformin intolerance, some experts suggest initiation of therapy with 2 drugs from other antidiabetic drug classes with complementary mechanisms of action.698 704
An α-glucosidase inhibitor (acarbose, miglitol) generally not recommended as second-line therapy after failure of metformin monotherapy because of comparatively lesser efficacy, frequent adverse GI effects, and greater cost, but may be appropriate therapy in selected patients.110 698
Consider early initiation of combination therapy for the treatment of type 2 diabetes mellitus to extend the time to treatment failure and more rapidly attain glycemic goals.704
For patients with inadequate glycemic control on metformin monotherapy, consider patient comorbidities (e.g., atherosclerotic cardiovascular disease [ASCVD], established kidney disease, heart failure), hypoglycemia risk, impact on weight, cost, risk of adverse effects, and patient preferences when selecting additional antidiabetic agents for combination therapy.698 699 704 705 706
Consider early introduction of insulin for severe hyperglycemia (e.g., blood glucose ≥300 mg/dL or HbA1c >9–10%), especially if accompanied by catabolic manifestations (e.g., weight loss, hypertriglyceridemia, ketosis) or symptoms of hyperglycemia.698 704
Acarbose Dosage and Administration
General
-
Individualize treatment and adjust target blood glucose and HbA1c concentrations based on patient’s understanding and adherence to the treatment regimen, the risk of severe hypoglycemia, and other factors that may increase risk or decrease benefit (e.g., very young or old age, comorbid conditions, other diseases that materially shorten life expectancy).1 62
-
Goal of therapy is to reduce both postprandial blood (or plasma) glucose and hemoglobin values to normal or near normal using lowest effective dosage of acarbose as monotherapy or combined with a sulfonylurea antidiabetic agent, metformin, or insulin.1 During therapy initiation and dosage titration, obtain 1-hour postprandial glucose concentration to determine therapeutic response and minimum effective dosage.1 14 23 52 62 Monitor HbA1c values at approximately every 3 months to evaluate long-term glycemic control.1 14 23 52 62 Monitor glucose concentrations 1–2 hours after the start of a meal in those who have elevated HbA1c despite adequate preprandial glucose concentrations.62
Administration
Oral Administration
Administer orally at the beginning (with the first bite) of each main meal.1 23
To minimize adverse GI effects, closely follow diabetic diet as prescribed.1 (See Adherence to Prescribed Diet under Cautions.)
Dosage
Adults
Type 2 Diabetes Mellitus
Oral
Initially, 25 mg at the beginning of each main meal (with first bite) 3 times daily.1 23 In patients with adverse GI effects,2 12 23 34 initiate at 25 mg once daily and increase dosage gradually as necessary to 25 mg 3 times daily.1
Once dosage of 25 mg 3 times daily has been reached, increase dosage at intervals of 4–8 weeks as tolerated to achieve the desired 1-hour postprandial glucose concentration (i.e., <180 mg/dL) or until maximum dosage (according to weight) is reached.1 23 34 41 52 62 (See Prescribing Limits under Dosage and Administration.) Maintenance dosage ranges from 50–100 mg 3 times daily.1 6 47
Dosages higher than 100 mg 3 times daily are not recommended since such dosages have been associated with an increased risk of elevated serum aminotransferase concentrations.1 10 18 19 20 22 23 25 27 30 37 43 52 If no further therapeutic benefit occurs at the maximum recommended dosage, consider lowering the dosage.1
Prescribing Limits
Adults
Type 2 Diabetes Mellitus
Oral
Patients ≤60 kg: maximum 50 mg 3 times daily.1 23 34 41 52
Patients >60 kg: maximum 100 mg 3 times daily.1
Cautions for Acarbose
Contraindications
-
Known hypersensitivity to the drug.1
-
Diabetic ketoacidosis.1
-
Cirrhosis.1
-
Inflammatory bowel disease, colonic ulceration, existing partial intestinal obstruction or predisposition to this condition.1
-
Chronic intestinal diseases associated with marked disorders of digestion or absorption.1
-
Co-existing conditions that may deteriorate as a result of increased intestinal gas formation.1
Warnings/Precautions
General Precautions
Metabolic Effects
Should not cause hypoglycemia when administered alone in the fasted or postprandial state.1 However, hypoglycemia (rarely hypoglycemic shock) may occur when used concomitantly with a sulfonylurea antidiabetic agent and/or insulin.1 If hypoglycemia occurs, adjust dosage of these agents appropriately.1 Use oral glucose (dextrose) for the treatment of mild to moderate hypoglycemia instead of sucrose (table sugar);1 the absorption of oral glucose is not inhibited by acarbose.1 Severe hypoglycemia may require the use of either IV glucose or parenteral glucagon.1
Insulin may be required for correction of temporary hyperglycemia that is not controlled by dietary regulation or oral antidiabetic agents during periods of severe stress (e.g., acute infection, trauma, surgery, fever).1 57 59
Hepatic Effects
Elevations in serum aminotransferase (i.e., ALT, AST) concentrations and, in rare instances, hyperbilirubinemia may occur, particularly with dosages exceeding 150 mg daily (50 mg 3 times daily).1 23 Jaundice and fatal hepatitis reported during postmarketing experience.1
Determine serum aminotransferase concentrations every 3 months during the first year of therapy and periodically thereafter.1 If elevations in serum aminotransferase concentrations occur, reduce dosage.1 May be necessary to withdraw the drug, particularly if elevated serum aminotransferase concentrations persist.1
Adherence to Prescribed Diet
If prescribed diet not followed closely, adverse GI effects may be intensified.1 If symptoms are strongly distressing despite adherence to prescribed diabetic diet, temporarily or permanently reduce acarbose dosage.1
Specific Populations
Pregnancy
Category B.1
Lactation
Distributed into milk in rats.1 Not known whether distributed into human milk.1 Use not recommended in nursing women.1
Pediatric Use
Safety and efficacy in children <18 years of age not established.1 23
Geriatric Use
Safety and efficacy in those ≥65 years of age similar to that in younger adults.1 (See Special Populations under Pharmacokinetics: Absorption.)
Hepatic Impairment
Contraindicated in patients with cirrhosis.1 23 52 Not studied in other conditions associated with hepatic impairment.1 23 52
Renal Impairment
Not recommended for use in diabetic patients with appreciable renal impairment (Scr >2 mg/dL).1 23
Common Adverse Effects
Flatulence, diarrhea, abdominal discomfort/pain.1
Digestive Enzyme Supplements
Possible reduction in the glycemic effects of acarbose.1 Avoid concomitant use.1
Intestinal Adsorbents
Possible reduction in the glycemic effects of acarbose.1 Avoid concomitant use.1
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
1,5-Anhydroglucitol assay |
Unreliable results in patients taking acarbose1 |
Manufacturer recommends use of alternative method to monitor glycemic control 1 |
|
Amylase (digestive enzyme preparation) |
Possible reduction in glycemic effects of acarbose1 |
Avoid concomitant use1 |
|
Calcium-channel blocking agents |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 No effect of acarbose on the pharmacokinetic or pharmacodynamics of nifedipine1 |
Monitor for loss of glycemic control1 When calcium-channel blocking agents are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia1 |
|
Charcoal (intestinal adsorbent) |
Possible reduction in glycemic effects of acarbose1 |
Avoid concomitant use1 |
|
Corticosteroids |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When corticosteroids are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia1 |
|
Contraceptives, oral |
Potential exacerbation of hyperglycemia/loss of glycemic control1 |
Monitor for loss of glycemic control1 When oral contraceptives are withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia1 |
|
Digoxin |
Decreased blood concentrations of digoxin1 |
May require increased digoxin dosage1 |
|
Diuretics (e.g., thiazides) |
Potential exacerbation of hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When diuretics are withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia1 |
|
Estrogens |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When estrogens are withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia1 |
|
Glyburide |
No effect on absorption or disposition of concomitant glyburide1 |
Pharmacokinetic interaction with glyburide unlikely1 |
|
Insulin |
Increased risk of hypoglycemia, rarely hypoglycemic shock, with concomitant insulin1 |
If hypoglycemia occurs, reduce insulin dosage1 |
|
Isoniazid |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When isoniazid is withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia1 |
|
Metformin |
Possible decreased peak plasma concentration of metformin1 |
Pharmacokinetic interaction not considered clinically important1 |
|
Nicotinic acid |
Potential to exacerbate diabetes mellitus, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When nicotinic acid is withdrawn in patients receiving concurrent sulfonylureas or insulin, observe for evidence of hypoglycemia1 |
|
Pancreatin (digestive enzyme preparation; no longer commercially available in the US) |
Possible reduction in glycemic effects of acarbose1 |
Avoid concomitant use1 |
|
Phenothiazines |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When phenothiazines are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia1 |
|
Phenytoin |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When phenytoin is withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia1 |
|
Pramlintide |
Delayed gastric emptying caused by α-glucosidase inhibitors may alter effects of pramlintide on GI absorption of nutrients112 |
Avoid concomitant pramlintide; safety/efficacy of combination therapy not established112 |
|
Propranolol |
Pharmacokinetic or pharmacodynamic interaction unlikely1 |
|
|
Ranitidine |
Pharmacokinetic or pharmacodynamic interaction unlikely1 |
|
|
Rosiglitazone |
Reduced extent of absorption and prolonged half-life of rosiglitazone113 Potential for altered glycemic control is uncertain114 |
Pharmacokinetic interaction not considered clinically important113 |
|
Sulfonylureas |
Increased risk of hypoglycemia, hypoglycemic shock with sulfonylureas1 |
If hypoglycemia occurs, reduce sulfonylurea dosage1 |
|
Sympathomimetic agents |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When sympathomimetic agents are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia.1 |
|
Thyroid agents |
Potential to exacerbate hyperglycemia, resulting in loss of glycemic control1 |
Monitor for loss of glycemic control1 When thyroid agents are withdrawn in patients receiving concurrent sulfonylureas or insulin, monitor for evidence of hypoglycemia1 |
Acarbose Pharmacokinetics
Absorption
Bioavailability
Low systemic bioavailability of parent compound; <2% of dose is absorbed as active drug (parent compound and active metabolite).1 Peak plasma concentrations of active drug attained at approximately 1 hour.1 Approximately 34% of dose absorbed as numerous metabolites.1
Onset
Satisfactory control of blood glucose concentrations achieved within a few days after dosage adjustment; however18 23 maximum response may be delayed for up to 2 weeks.18 23
Special Populations
In geriatric patients, mean AUC and peak blood concentrations of the drug were higher compared with younger adults;1 differences not statistically significant.1
In individuals with severe renal impairment (CLcr <25 mL/minute), peak plasma drug concentrations and AUC increased compared with those values in individuals with normal renal function.1
Distribution
Extent
Distributed into milk in rats.1
Elimination
Metabolism
Metabolized exclusively in GI tract, principally by intestinal bacteria but also by digestive enzymes to numerous metabolites, one of which is active.1
Elimination Route
Excreted principally in feces (51% of dose) as unabsorbed drug and in urine as metabolites (34% of dose).1 No accumulation with recommended dosing frequency.1
Half-life
Approximately 2 hours.1
Stability
Storage
Oral
Tablets
≤25°C.1 Protect from moisture.1
Actions
-
Small inhibitory effect on α-glucosidase enzymes (e.g., glucoamylase, sucrase, maltase, isomaltase) that hydrolyze oligosaccharides, trisaccharides, and disaccharides to glucose and other monosaccharides in the intestinal brush-border.2 6 14 24 29 30 52 Small inhibitory effect on pancreatic α-amylase, which hydrolyzes starch into maltose, maltotriose, and dextrins in the lumen of the small intestine.2 14 30 33 No inhibitory effect on lactase and would not be expected to produce lactose intolerance.1
-
Delays carbohydrate breakdown and glucose absorption and reduces postprandial hyperglycemia in diabetic patients.1 2 6 7 10 14 23 24 30
-
Reduces fluctuations in the daily blood glucose concentration-time profile in patients with type 2 diabetes mellitus and in lean or obese nondiabetic individuals.1 2 3 6 7 19 20 21 23 24 35 37 39 47 Fasting blood glucose concentrations either not affected or mildly decreased.1 2 3 6 7 19 20 21 23 24 35 37 39 47
-
In contrast to sulfonylurea antidiabetic agents, acarbose does not enhance insulin secretion.1 Does not produce hypoglycemia when given as monotherapy in fasting individuals.1
-
When used in combination with sulfonylurea antidiabetic agents are used in combination, acarbose reduces the insulinotropic and weight-increasing effects of sulfonylureas.1 No clinically important loss of calories or weight loss occurs in either diabetic or nondiabetic individuals.2 6 13 14 18 21 23 28 35 37 39
Advice to Patients
-
Importance of adherence to diet and exercise regimen.1 23 54
-
Importance of adherence to dietary precautions designed to minimize adverse GI effects.1 108 Importance of consulting a clinician for dosage adjustments if adverse GI effects occur despite adherence to such dietary precautions.1 (See Adherence to Prescribed Diet under Cautions.)
-
Importance of regular monitoring of blood glucose concentrations.1 14 23 52 62
-
Importance of avoiding infection.23
-
Provide instruction on the management of hyperglycemia or hypoglycemia.23 62 Advise of the risk of hypoglycemia, its symptoms, and conditions that predispose to the development of hypoglycemia.1 Importance of keeping a readily available source of glucose (dextrose) to treat symptoms of hypoglycemia when used in combination with a sulfonylurea agent or insulin.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of advising patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
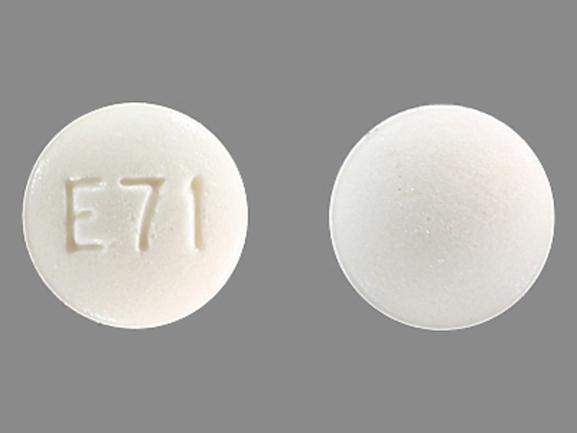
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg* |
Acarbose Tablets |
|
|
50 mg* |
Acarbose Tablets |
|||
|
100 mg* |
Acarbose Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 21, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Mylan. Acarbose tablets prescribing information. Morgantown, WV; 2015 Apr.
2. Clissold SP, Edwards C. Acarbose: a preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential. Drugs. 1988; 35:214-43. https://pubmed.ncbi.nlm.nih.gov/3286212
3. Anon. Acarbose–an α-glucosidase inhibitor. Int Pharm J. 1994; 8:11-12.
6. Santeusanio F, Compagnucci P. A risk-benefit appraisal of acarbose in the management of non-insulin-dependent diabetes mellitus. Drug Saf. 1994; 11:432-44. https://pubmed.ncbi.nlm.nih.gov/7727053
7. Jenkins DJA, Taylor RH, Goff DV et al. Scope and specificity of acarbose in slowing carbohydrate absorption in man. Diabetes. 1981; 30:951-4. https://pubmed.ncbi.nlm.nih.gov/7028548
10. Hayakawa T, Kondo T, Okumura N et al. Enteroglucagon release in disaccharide malabsorption induced by intestinal α-glucosidase inhibition. Am J Gastroenterol. 1989; 84:523-6. https://pubmed.ncbi.nlm.nih.gov/2655436
11. Bristol-Myers Squibb, Princeton, NJ: personal communication on metformin.
12. Scheppach W, Fabian C, Ahrens F et al. Effect of starch malabsorption on colonic function and metabolism in humans. Gastroenterology. 1988; 95:1549-55. https://pubmed.ncbi.nlm.nih.gov/3053313
13. Fölsch UR, Ebert R, Creutzfeldt W. Response of serum levels of gastric inhibitory polypeptide and insulin to sucrose ingestion during long-term application of acarbose. Scand J Gastroenterol. 1981; 16:629-32. https://pubmed.ncbi.nlm.nih.gov/7034156
14. Balfour JA, McTavish D. Acarbose: an update of its pharmacology and therapeutic use in diabetes mellitus. Drugs. 1993; 46:1025-54. https://pubmed.ncbi.nlm.nih.gov/7510610
16. Carlisle BA, Kroon LA, Koda-Kimble MA. Diabetes mellitus. In: Koda-Kimble MA, Young LY, eds. Applied therapeutics: the clinical use of drugs. 8th ed. Philadelphia, PA: Lippincott Williams &Wilkins; 2005: 50-1–50-86.
18. Coniff RF, Shapiro JA, Seaton TB. Long-term efficacy and safety of acarbose in the treatment of obese subjects with non-insulin-dependent diabetes mellitus. Arch Intern Med. 1994; 154:2442-8. https://pubmed.ncbi.nlm.nih.gov/7979840
19. Coniff RF, Shapiro JA, Seaton TB et al. Multicenter, placebo-controlled trial comparing acarbose (BAY g 5421) with placebo, tolbutamide, and tolbutamide-plus-acarbose in non-insulin-dependent diabetes mellitus. Am J Med. 1995; 98:443-51. https://pubmed.ncbi.nlm.nih.gov/7733122
20. Coniff RF, Shapiro JA, Robbins D et al. Reduction of glycosylated hemoglobin and postprandial hyperglycemia by acarbose in patients with NIDDM: a placebo-controlled dose-comparison study. Diabetes Care. 1995; 18:817-24. https://pubmed.ncbi.nlm.nih.gov/7555508
21. Hoffmann J, Spengler M. Efficacy of 24-week monotherapy with acarbose, glibenclamide, or placebo in NIDDM patients: the Essen Study. Diabetes Care. 1994; 17:561-6. https://pubmed.ncbi.nlm.nih.gov/8082525
22. Chiasson J-L, Josse RG, Hunt JA et al. The efficacy of acarbose in the treatment of patients with non-insulin-dependent diabetes mellitus. Ann Intern Med. 1994; 121:928-35. https://pubmed.ncbi.nlm.nih.gov/7734015
23. Bayer, West Haven, CT: Personal communication.
24. Toeller M. Nutritional recommendations for diabetic patients and treatment with α-glucosidase inhibitors. Drugs. 1992; 44(Suppl 3):13- 20. https://pubmed.ncbi.nlm.nih.gov/1280573
25. Coniff RF, Shapiro JA, Seaton TB et al. A double-blind placebo- controlled trial evaluating the safety and efficacy of acarbose for the treatment of patients with insulin-requiring type II diabetes. Diabetes Care. 1995; 18:928-32. https://pubmed.ncbi.nlm.nih.gov/7555551
26. Zimmerman BR. Preventing long term complications: implications for combination therapy with acarbose. Drugs. 1992; 44(Suppl 3):54-60. https://pubmed.ncbi.nlm.nih.gov/1280578
27. Anon. Round-table discussion. Drugs. 1992; 44(Suppl 3):61-5. https://pubmed.ncbi.nlm.nih.gov/1283586
28. Hollander P. Safety profile of acarbose, an α-glucosidase inhibitor. Drugs. 1992; 44(Suppl 3):47-53. https://pubmed.ncbi.nlm.nih.gov/1280577
29. William-Olsson T, Krotkiewski M, Sjöström L. Relapse- reducing effects of acarbose after weight reduction in severely obese subjects. J Obesity Weight Regulation. 1985; 4:20-32.
30. William-Olsson T. α-glucosidase inhibition in obesity. Acta Med Scand Suppl. 1985; 706:1-39. https://pubmed.ncbi.nlm.nih.gov/3914827
31. Shichiri M, Kishikawa H, Ohkubo Y et al. Long-term results of the Kumamoto study on optimal diabetes control in type 2 diabetic patients.Diabetes Care. 2000; 23 (Suppl 2):B21-9. https://pubmed.ncbi.nlm.nih.gov/10860187
33. Hiele M, Ghoos Y, Rutgeerts P et al. Effects of acarbose on starch hydrolysis: study in healthy subjects, ileostomy patients, and in vitro. Dig Dis Sci. 1992; 37:1057-64. https://pubmed.ncbi.nlm.nih.gov/1618053
34. Rodier M, Richard JL, Monnier L et al. Effect of long term acarbose (Bay g 5421) therapy on metabolic control of non insulin dependent (Type II) diabetes mellitus. Diabete Metab. 1988; 14:12-4. https://pubmed.ncbi.nlm.nih.gov/3292303
35. Couet C, Ulmer M, Hamdaoui M et al. Metabolic effects of acarbose in young healthy men. Eur J Clin Nutr. 1989; 43:187-96. https://pubmed.ncbi.nlm.nih.gov/2659314
36. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993; 329:977-86. https://pubmed.ncbi.nlm.nih.gov/8366922
37. Hanefeld M, Fischer S, Schulze J et al. Therapeutic potentials of acarbose as first-line drug in NIDDM insufficiently treated with diet alone. Diabetes Care. 1991; 14:732-7. https://pubmed.ncbi.nlm.nih.gov/1954810
39. Baron AD, Eckel RH, Schmeiser L et al. The effect of short-term alpha-glucosidase inhibition on carbohydrate and lipid metabolism in type II (noninsulin-dependent) diabetics. Metab Clin Exp. 1987; 36:409-15. https://pubmed.ncbi.nlm.nih.gov/3553848
40. Sailer D, Röder G. Treatment of non-insulin dependent diabetic adults with a new glycoside hydrolase inhibitor (Bay g 5421). Arzneimittelforschung. 1980; 30:2182-5. https://pubmed.ncbi.nlm.nih.gov/7194082
41. Ahr HJ, Boberg M, Krause HP et al. Pharmacokinetics of acarbose: Part I: absorption, concentration in plasma, metabolism and excretion after single administration of [14C]acarbose to rats, dogs and man. Arzneimittelforschung. 1989; 39:1254-60. https://pubmed.ncbi.nlm.nih.gov/2610717
42. Klein R, Klein BEK, Moss SE et al. Glycosylated hemoglobin predicts the incidence and progression of diabetic retinopathy. JAMA. 1988; 260:2864-71. https://pubmed.ncbi.nlm.nih.gov/3184351
43. Scheen AJ, Castillo MJ, Lefèbvre PJ. Combination of oral antidiabetic drugs and insulin in the treatment of non-insulin-dependent diabetes. Acta Clin Belg. 1993; 48:259-68. https://pubmed.ncbi.nlm.nih.gov/8212978
44. Reaven GM, Lardinois CK, Greenfield MS et al. Effect of acarbose on carbohydrate and lipid metabolism in NIDDM patients poorly controlled by sulfonylureas. Diabetes Care. 1990; 13(Suppl 3):32-6. https://pubmed.ncbi.nlm.nih.gov/2209341
45. Gérard J, Luyckx AS, Lefebvre PJ. Improvement of metabolic control in insulin dependent diabetics treated with the α-glucosidase inhibitor acarbose for two months. Diabetologia. 1981; 21:446-51. https://pubmed.ncbi.nlm.nih.gov/7028558
46. Rybka J, Gregorová A, Zmydlená A et al. Clinical study of acarbose. Drug Invest. 1990; 2:264-7.
47. Santeusanio F, Ventura MM, Contadini S et al. Efficacy and safety of two different dosages of acarbose in non-insulin dependent diabetic patients treated by diet alone. Diabetes Nutr Metab. 1993; 6:147-54.
48. Dimitriadis GD, Tessari P, Go VLW et al. α-Glucosidase inhibition improves postprandial hyperglycemia and decreases insulin requirements in insulin-dependent diabetes mellitus. Metabolism. 1985; 34:261-5. https://pubmed.ncbi.nlm.nih.gov/3883097
49. Sachse G, Willms B. Effect of the α-glucosidase-inhibitor BAY-g- 5421 on blood glucose control of sulphonylurea-treated diabetics and insulin- treated diabetics. Diabetologia. 1979; 17:287-90. https://pubmed.ncbi.nlm.nih.gov/387504
51. Calle-Pascual AL, Garcia-Honduvilla J, Martin-Alvarez PJ et al. Comparison between acarbose, metformin, and insulin treatment in type 2 diabetic patients with secondary failure to sulfonylurea treatment. Diabete Metab. 1995; 21:256-60. https://pubmed.ncbi.nlm.nih.gov/8529760
52. Bayer. Product information form for American hospital formulary service: Precose (acarbose tablets). West Haven, CT; 1996 Apr.
54. National Institutes of Health Office of Medical Applications of Research. Consensus development conference statement: diet and exercise in noninsulin-dependent diabetes mellitus. Bethesda, MD: 1986(Dec 10); 6:1-7. Available at National Institutes of Health website. Accessed 2007 Feb 5. http://consensus.nih.gov/1986/1986DietExerciseDiabetesII060html.htm
57. Bailey CJ, Turner RC. Metformin. N Engl J Med. 1996; 334:574-9. https://pubmed.ncbi.nlm.nih.gov/8569826
59. American Diabetes Association. Office guide to diagnosis and classification of diabetes mellitus and other categories of glucose intolerance. Diabetes Care. 1995; 18(Suppl 1):4.
62. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2006;29 (Suppl 1):S4-42.
63. Knudson PE, Weinstock RS, Henry JB. Carbohydrates. In: Henry JB, ed. Todd-Sanford-Davidsohn clinical diagnosis and management by laboratory methods. 20th ed. Philadelphia: W.B. Saunders Company; 2001:211-23.
64. Polonsky KS, Sturis J, Bell GI. Non-insulin-dependent diabetes mellitus—a genetically programmed failure of the beta cell to compensate for insulin resistance. N Engl J Med. 1996; 334:777-83. https://pubmed.ncbi.nlm.nih.gov/8592553
68. U. K. Prospective Diabetes Study Group. U. K. prospective diabetes study 16: overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes. 1995; 44:1249-58. https://pubmed.ncbi.nlm.nih.gov/7589820
70. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837-53. https://pubmed.ncbi.nlm.nih.gov/9742976
71. American Diabetes Association. Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care. 1999; 22(Suppl 1):27-31. https://pubmed.ncbi.nlm.nih.gov/10333899
72. Matthews DR, Cull CA, Stratton RR et al. UKPDS 26: sulphonylurea failure in non-insulin-dependent diabetic patients over 6 years. Diabet Med. 1998; 15:297-303. https://pubmed.ncbi.nlm.nih.gov/9585394
75. Genuth S, Brownless MA, Kuller LH et al. Consensus development conference on insulin resistance: Novermber 5-6 1997. Diabetes Care. 1998; 21:310-4. https://pubmed.ncbi.nlm.nih.gov/9540000
78. Nathan DM. Some answers, more controversy, from UKDS. Lancet. 1998; 352:832-3. https://pubmed.ncbi.nlm.nih.gov/9742972
82. UK Prospective Diabetes Study (UKPDS) Group. ffect of intensive blood-glucose control with metfromin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998; 352:854-65. https://pubmed.ncbi.nlm.nih.gov/9742977
90. American Diabetes Association. Type 2 diabetes in children and adolescents. Pediatrics. 2000; 105:671-80. https://pubmed.ncbi.nlm.nih.gov/10699131
92. United Kingdom Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998; 317:703-13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC28659/ https://pubmed.ncbi.nlm.nih.gov/9732337
93. UK Prospective Diabetes Study (UKPDS) Group. Efficacy of atenolol and captopril in reducing risk of macrovascular complications in type 2 diabetes mellitus: UKPDS 39. BMJ. 1998; 317:713-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC28660/ https://pubmed.ncbi.nlm.nih.gov/9732338
99. Buse J. Combining insulin and oral agents. Am J Med. 2000; 108(Suppl 6A):23S-32S. https://pubmed.ncbi.nlm.nih.gov/10764847
101. Yki-Jarvinen H, Dressler A, Ziemen M et al. Less nocturnal hypoglycemia and better post-dinner glucose control with bedtime insulin glargine compared with bedtime HPH insulin during insulin combination therapy in type 2 diabetes. Diabetes Care. 2000; 23:1130-6 (IDIS 451244) https://pubmed.ncbi.nlm.nih.gov/10937510
102. Eli Lilly and Company. Humalog (insulin lispro, rDNA origin) injection prescribing information. Indianapolis, IN; 2000 May 1.
104. Florence JA, Yeager BF. Treatment of type 2 diabetes mellitus. Am Fam Physician. 1999; 59:2835-44. https://pubmed.ncbi.nlm.nih.gov/10348076
105. Bastyr EJ, Johnson ME, Trautman ME et al. Insulin lispro in the treatment of patients with type 2 diabetes mellitus after oral agent failure. Clin Ther. 1999; 21:1703-4. https://pubmed.ncbi.nlm.nih.gov/10566566
106. DeFronzo RA. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med. 1999; 131:281-303. https://pubmed.ncbi.nlm.nih.gov/10454950
108. Bayer. Managing you diabetes with Precose. Questions/answers to help you get the most out of your diabetes treatment plan. West Haven, CT; 2001 May.
109. American Diabetes Association. Preconception care of women with diabetes. Diabetes Care. 2004; 27(Suppl 1):S76-78.
110. Nathan DM, Buse JB, Davidson MB et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. A consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009; 32:193-203. https://pubmed.ncbi.nlm.nih.gov/18945920
111. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2003 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2003; 27 (Suppl 2):S1-152.
112. Amylin Pharmaceuticals. Symlin (pramlintide acetate) injection prescribing information. San Diego, CA; 2005 Mar.
113. GlaxoSmithKline. Avandia (rosiglitazone maleate) tablets prescribing information. Research Triangle Park, NC; 2006 Jun.
114. SmithKline Beecham Pharmaceuticals, Philadelphia, PA: Personal communication.
698. Garber AJ, Handelsman Y, Grunberger G et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm 2020 executive summary. Endocr Pract. 2020; 26:107-139. https://pubmed.ncbi.nlm.nih.gov/32022600
699. Zelniker TA, Wiviott SD, Raz I et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019; 139(17):2022-2031. https://pubmed.ncbi.nlm.nih.gov/30786725
704. American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020; 43:S98-S110. https://pubmed.ncbi.nlm.nih.gov/31862752
705. American Diabetes Association. 10. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020; 43:S111-S134. https://pubmed.ncbi.nlm.nih.gov/31862753
706. American Diabetes Association. 11. Microvascular complications and foot care: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020; 43:S135-S151. https://pubmed.ncbi.nlm.nih.gov/31862754
Related/similar drugs
More about acarbose
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (5)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: alpha-glucosidase inhibitors
- Breastfeeding
- En español