Upper Respiratory Infection in Children
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
AMBULATORY CARE:
An upper respiratory infection
is also called a cold. It can affect your child's nose, throat, ears, and sinuses. Most children get about 5 to 8 colds each year. Children get colds more often in winter.
Causes of a cold:
A cold is caused by a virus. Many viruses can cause a cold, and each is contagious. A virus may be spread to others through coughing, sneezing, or close contact. A virus can also stay on objects and surfaces. Your child can become infected by touching the object or surface and then touching his or her eyes, mouth, or nose.
Signs and symptoms of a cold
will be worst for the first 3 to 5 days. Your child may have any of the following:
- Runny or stuffy nose
- Sneezing and coughing
- Sore throat or hoarseness
- Red, watery, and sore eyes
- Tiredness or fussiness
- Chills and a fever that usually lasts 1 to 3 days
- Headache, body aches, or sore muscles
Seek care immediately if:
- Your child's temperature reaches 105°F (40.6°C).
- Your child has trouble breathing or is breathing faster than usual.
- Your child's lips or nails turn blue.
- Your child's nostrils flare when he or she takes a breath.
- The skin above or below your child's ribs is sucked in with each breath.
- Your child's heart is beating much faster than usual.
- You see pinpoint or larger reddish-purple dots on your child's skin.
- Your child stops urinating or urinates less than usual.
- Your baby's soft spot on his or her head is bulging outward or sunken inward.
- Your child has a severe headache or stiff neck.
- Your child has chest or stomach pain.
- Your baby is too weak to eat.
Call your child's doctor if:
- Your child has a rectal, ear, or forehead temperature higher than 100.4°F (38°C).
- Your child has an oral or pacifier temperature higher than 100°F (37.8°C).
- Your child has an armpit temperature higher than 99°F (37.2°C).
- Your child is younger than 2 years and has a fever for more than 24 hours.
- Your child is 2 years or older and has a fever for more than 72 hours.
- Your child has had thick nasal drainage for more than 2 days.
- Your child has ear pain.
- Your child has white spots on his or her tonsils.
- Your child coughs up a lot of thick, yellow, or green mucus.
- Your child is unable to eat, has nausea, or is vomiting.
- Your child has increased tiredness and weakness.
- Your child's symptoms do not improve or get worse within 3 days.
- You have questions or concerns about your child's condition or care.
Treatment for your child's cold:
Colds are caused by viruses and do not get better with antibiotics. Most colds in children go away without treatment in 1 to 2 weeks. Do not give over-the-counter (OTC) cough or cold medicines to children younger than 4 years. Your child's healthcare provider may tell you not to give these medicines to children younger than 6 years. OTC cough and cold medicines can cause side effects that may harm your child. Your child may need any of the following to help manage his or her symptoms:
- Decongestants help reduce nasal congestion in older children and help make breathing easier. If your child takes decongestant pills, they may make him or her feel restless or cause problems with sleep. Do not give your child decongestant sprays for more than a few days.
- Cough suppressants help reduce coughing in older children. Ask your child's healthcare provider which type of cough medicine is best for your child.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Care for your child:
- Have your child rest. Rest will help your child get better.
- Give your child more liquids as directed. Liquids will help thin and loosen mucus so your child can cough it up. Liquids will also help prevent dehydration. Liquids that help prevent dehydration include water, fruit juice, and broth. Do not give your child liquids that contain caffeine. Caffeine can increase your child's risk for dehydration. Ask your child's healthcare provider how much liquid to give your child each day.
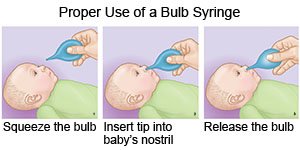
- Clear mucus from your child's nose. Use a bulb syringe to remove mucus from a baby's nose. Squeeze the bulb and put the tip into one of your baby's nostrils. Gently close the other nostril with your finger. Slowly release the bulb to suck up the mucus. Empty the bulb syringe onto a tissue. Repeat the steps if needed. Do the same thing in the other nostril. Make sure your baby's nose is clear before he or she feeds or sleeps. Your child's healthcare provider may recommend you put saline drops into your baby's nose if the mucus is very thick.
- Soothe your child's throat. If your child is 8 years or older, have him or her gargle with salt water. Make salt water by dissolving ¼ teaspoon salt in 1 cup warm water.
- Soothe your child's cough. You can give honey to children older than 1 year. Give ½ teaspoon of honey to children 1 to 5 years. Give 1 teaspoon of honey to children 6 to 11 years. Give 2 teaspoons of honey to children 12 or older.
- Use a cool-mist humidifier. This will add moisture to the air and help your child breathe easier. Make sure the humidifier is out of your child's reach.
- Apply petroleum-based jelly around the outside of your child's nostrils. This can decrease irritation from blowing his or her nose.
- Keep your child away from cigarette and cigar smoke. Do not smoke near your child. Do not let your older child smoke. Nicotine and other chemicals in cigarettes and cigars can make your child's symptoms worse. They can also cause infections such as bronchitis or pneumonia. Ask your child's healthcare provider for information if you or your child currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you or your child use these products.
Prevent the spread of a cold:
- Have your child wash his or her hands often. Teach your child to use soap and water every time. Show your child how to rub his or her soapy hands together, lacing the fingers. Your child should use the fingers of one hand to scrub under the nails of the other hand. Your child needs to wash his or her hands for at least 20 seconds. This is about the time it takes to sing the happy birthday song 2 times. Your child should rinse his or her hands with warm, running water for several seconds, then dry them with a clean towel. Tell your child to use hand sanitizer gel if soap and water are not available. Teach your child not to touch his or her eyes or mouth without washing first.

- Show your child how to cover a sneeze or cough. Use a tissue that covers your child's mouth and nose. Teach your child to put the used tissue in the trash right away. Use the bend of your arm if a tissue is not available. Wash your hands well with soap and water or use a hand sanitizer. Do not stand close to anyone who is sneezing or coughing.
- Keep your child home as directed. This is especially important during the first 2 to 3 days when the virus is more easily spread. Wait until a fever, cough, or other symptoms are gone before letting your child return to school, daycare, or other activities.
- Do not let your child share items while he or she is sick. This includes toys, pacifiers, and towels. Do not let your child share food, eating utensils, drinks, or cups with anyone.
Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Upper Respiratory Infection
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
