Reactive Airways Disease
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is reactive airways disease (RAD)?
RAD is a term used to describe breathing problems in children up to 5 years old. The signs and symptoms of RAD are similar to asthma, such as wheezing and shortness of breath. RAD symptoms can occur because of airway swelling. A child's airways are small and narrow, making it easy for them to fill and get blocked with mucus. These factors make it hard for healthcare providers to know what is causing your child's symptoms, or the best way to treat them.
What increases my child's risk for RAD?
- A family history of asthma or allergies
- Not being breastfed, or only being breastfed for fewer than 3 months
- A lung infection caused by a virus, such as respiratory syncytial virus (RSV)
- Treatment in the hospital for bronchiolitis
- Being around secondhand smoke, or his or her mother smoked while she was pregnant
- Being around anything that can trigger an allergic response, such as pollen and pets
What signs and symptoms may mean that my child has RAD?
The signs and symptoms of RAD are similar to asthma. Your child may have any of the following:
- Wheezing or crackles when your child breathes
- Trouble breathing
- A cough that does not go away
- A fast heartbeat
- A runny nose
- Symptoms worsen at night, during sickness or exercise, when laughing or crying, or when around triggers
How is RAD diagnosed?
Healthcare providers will ask you about your child's symptoms. Tell them if your child's symptoms get worse when he or she is around a trigger, such as pets or smoke. Tell them if the symptoms get worse at night, or in cold air. Tell them if your infant grunts or sucks poorly when he or she is feeding. If your older child has to miss school, often feels ill, or is too tired to exercise, tell healthcare providers. Your child may need one or more of the following tests to find the cause of his or her symptoms:
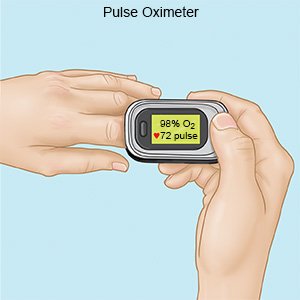
- A pulse oximeter is a device that measures the amount of oxygen in your child's blood.
- A spirometer measures how well your older child can breathe. He or she will take a deep breath and then push the air out as fast as possible. This test measures how much air your child is able to push out. This is called forced expiratory volume (FEV). The test results show healthcare providers how small your child's airways have become.
- Mucus samples from your child's nose or throat may be collected and tested. The results may tell healthcare providers what is causing your child's symptoms.
- Blood tests may be used to check for signs of infection or another cause for your child's symptoms.
- X-rays may be used to check your child's heart, lungs, and chest wall. It can help healthcare providers diagnose your child's symptoms, or suggest or monitor treatment for medical conditions.
Related medications
How is RAD treated?
Healthcare providers may treat your child's symptoms with medicines. They may follow up with your child as he or she gets older to see if his or her symptoms go away. Your child may need to use medicines every day or only when needed. He or she may need one or more of the following:
- Short-acting bronchodilators help open the airways quickly. They relieve sudden, severe symptoms and start to work right away.
- Long-acting bronchodilators help prevent breathing problems. They control breathing problems by keeping the airways open over time.
- Corticosteroids help decrease swelling and open the airway to make breathing easier. Your child may breathe the medicine in or swallow it as a liquid, pill, or chewable tablet.
- Breathing treatments open your child's airways so he or she can breathe more easily. Your child may need to use a nebulizer or an inhaler to help him or her breathe in the medicine. Ask healthcare providers for more information about these devices, and to show you and your child how to use them.
- Oxygen may be given to help your child breathe easier. He or she may need a nasal cannula (small tubes placed in the nose) or mask.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What can I do to help my child prevent flares?
- Keep your child away from cigarette smoke. Cigarette smoke can harm your child's lungs and cause breathing problems. Ask your healthcare provider for more information if you currently smoke and want help to quit.
- Keep all follow-up visits. Tell healthcare providers about your child's symptoms. For example, tell them how often and how badly your child is wheezing or coughing. Make sure your child gets all of the vaccines suggested by his or her healthcare provider.
- Help your child avoid triggers. A trigger is anything that starts your child's symptoms or makes them worse. If you know that your child is allergic to a certain food, do not let him or her have it. The allergy can cause his or her airways to close. This can be life-threatening. Avoid areas where there is pollution, perfume, or dust. Remove pets from your home.
- Avoid spreading illness. Keep your child away from others if he or she has a fever or other symptoms. Do not send your child to school or daycare until his or her fever is gone and he or she is feeling better. Keep your child away from large groups of people or others who are sick. This decreases his or her chance of getting sick.
- Make changes to your home. Your child's signs and symptoms may get worse when he or she is around dust mites, cockroaches, or mold. You can help keep your home free from these triggers. Keep the humidity (moisture level in the air) low. Fix leaks, and remove carpets where possible. Use mattress covers, and wash bedding every 1 to 2 weeks in hot water. Wash tables and other surfaces with weak bleach (1 tablespoon of bleach in a gallon of water).
- Ask healthcare providers to create an asthma action plan. An asthma action plan may help you and your child manage RAD symptoms at home. The plan will include signs to watch for that mean your child's symptoms are getting worse. The plan will state what to do if this occurs, and list emergency phone numbers. Your child's triggers will be on the plan so that you both know what to avoid. The plan will list any medicines your child takes. It will also state when your child should see his or her healthcare provider for a follow-up visit.
What can I do to help my child develop a strong immune system?
- Breastfeed your child, if possible. Breast milk helps protect him or her from allergies that can trigger wheezing and other problems.
- Help your child get enough exercise and eat healthy foods. Your child's healthcare provider can teach you how to manage your child's cough or shortness of breath while he or she is active. If symptoms get worse with exercise, your child may need to take medicine through an inhaler 10 to 15 minutes before exercise. Give your child healthy foods. Ask your child's healthcare provider what a healthy weight is for your child. If your child weighs more than his or her provider says is healthy, symptoms of RAD may get worse.

When should I seek immediate care?
- Your child's wheezing or cough is getting worse.
- Your child has trouble breathing, or his or her lips or fingernails are blue.
- Your older child cannot talk in full sentences because he or she is trying to breathe.
- Your child looks restless and is breathing fast.
- Your child's nostrils flare out as he or she tries to breathe. His or her stomach muscles or the skin over his or her ribs may move in deeply while he or she tries to breathe.
- Your child goes from being restless to being confused or sleepy.
When should I call my child's doctor?
- Your child is shaky, nervous, or has a headache.
- Your child is hoarse, or has a sore throat or upset stomach.
- Your infant often throws up when he or she coughs.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Reactive Airways Disease
Treatment options
- Medications for Allergic Asthma
- Medications for Asthma
- Medications for Infection
- Medications for Pleuropulmonary Infection
- Medications for Pulmonary Impairment
Care guides
- Asthma
- Bronchiolitis
- COPD (Chronic Obstructive Pulmonary Disease)
- Exercise-Induced Bronchoconstriction
- Foreign Body Ingestion
- Mers (Middle East Respiratory Syndrome)
- Moderate and Severe Persistent Asthma
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
