Reactive Airways Disease
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
Reactive airways disease (RAD) is a term used to describe breathing problems in children up to 5 years old. The signs and symptoms of RAD are similar to asthma, such as wheezing and shortness of breath.
DISCHARGE INSTRUCTIONS:
Return to the emergency department if:
- Your child's wheezing or cough is getting worse.
- Your child has trouble breathing, or his or her lips or fingernails are blue.
- Your older child cannot talk in full sentences because he or she is trying to breathe.
- Your child looks restless and is breathing fast.
- Your child's nostrils flare out as he or she tries to breathe. His or her stomach muscles or the skin over his or her ribs may move in deeply while he or she tries to breathe.
- Your child goes from being restless to being confused or sleepy.
Call your child's doctor if:
- Your child is shaky, nervous, or has a headache.
- Your child is hoarse, or has a sore throat or upset stomach.
- Your infant throws up when he or she coughs.
- You have questions or concerns about your child's condition or care.
Medicines:
Your child may need any of the following:
- Short-acting bronchodilators help open the airways quickly. They relieve sudden, severe symptoms and start to work right away.
- Long-acting bronchodilators help prevent breathing problems. They control breathing problems by keeping the airways open over time.
- Corticosteroids help decrease swelling and open the airway to make breathing easier. Your child may breathe the medicine in or swallow it as a liquid, pill, or chewable tablet.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Drugs used to treat this and similar conditions
Nucala
Nucala is used to treat severe eosinophilic asthma, chronic rhinosinusitis with nasal polyps ...
Dupixent
Dupixent is used to treat eczema, eosinophilic or oral-corticosteroid-dependent asthma, chronic ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Xolair
Xolair injection (omalizumab) is used to reduce the risk of severe food allergy reactions ...
Albuterol
Albuterol is a bronchodilator that relaxes muscles in the airways and increases air flow to the ...
Omalizumab
Omalizumab (Xolair) injection is used to reduce the risk of severe food allergy reactions ...
Dupilumab
Dupilumab (Dupixent) is used to treat eczema, eosinophilic or oral-corticosteroid-dependent asthma ...
Budesonide
Budesonide systemic is used for asthma, asthma, maintenance, autoimmune hepatitis, crohn's disease ...
Mepolizumab
Mepolizumab (Nucala) is a prescription medication FDA-approved for several eosinophil-related ...
Prednisone
Prednisone is used to treat allergic disorders, ulcerative colitis, psoriasis and arthritis. Learn ...
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Inhalers:
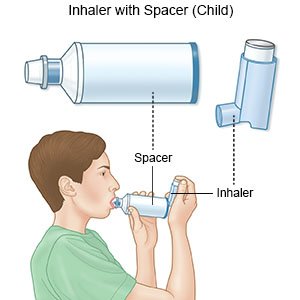
- A metered dose inhaler is a small, tube-shaped device. Your child holds the open end inside his or her mouth. The medicine comes out as a mist when he or she presses a switch. He or she may use a spacer with this inhaler. A spacer is a large tube that holds the mist before your child breathes it in.
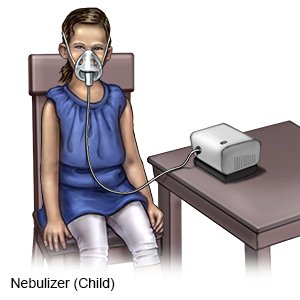
- A nebulizer has a long tube that goes from the machine to a small round container that holds asthma medicine. The liquid turns into a mist when the machine is turned on. Your child breathes in this mist through a mouthpiece.
- A dry powder inhaler is a small tube or disc-shaped device that contains powder asthma medicine. Your child holds the open end inside his or her mouth. The powder is released when he or she presses a switch. With this type of inhaler, your child must breathe in hard to suck in the powder.
Help your child prevent flares:
- Use a humidifier. A humidifier will increase air moisture in your home. This may make it easier for your child to breathe. Keep humidifiers out of the reach of children.
- Keep your child away from cigarette smoke. Cigarette smoke can harm your child's lungs and cause breathing problems. Ask your healthcare provider for more information if you currently smoke and want help to quit.
- Help your child avoid triggers. Triggers include certain foods, pollution, perfume, mold, pets, or dust.
- Manage your child's symptoms. Follow directions for how to manage your child's cough or shortness of breath while he or she is active. If symptoms get worse with exercise, your child may need to take medicine through an inhaler 10 to 15 minutes before exercise.
- Avoid spreading illness. Keep your child away from others if he or she has a fever or other symptoms. Do not send your child to school or daycare until his or her fever is gone and he or she is feeling better. Keep your child away from large groups of people or others who are sick. This decreases his or her chance of getting sick.
Help your child develop a strong immune system:
- Breastfeed your child, if possible. Breast milk helps protect him or her from allergies that can trigger wheezing and other problems.
- Help your child get enough exercise and eat healthy foods. Your child's healthcare provider can teach you how to manage your child's cough or shortness of breath while he or she is active. If symptoms get worse with exercise, your child may need to take medicine through an inhaler 10 to 15 minutes before exercise. Give your child healthy foods. Ask your child's healthcare provider what a healthy weight is for your child. If your child weighs more than his or her provider says is healthy, symptoms of RAD may get worse.

Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Reactive Airways Disease
Treatment options
- Medications for Allergic Asthma
- Medications for Asthma
- Medications for Infection
- Medications for Pleuropulmonary Infection
- Medications for Pulmonary Impairment
Care guides
- Asthma
- Bronchiolitis
- COPD (Chronic Obstructive Pulmonary Disease)
- Exercise-Induced Bronchoconstriction
- Foreign Body Ingestion
- Mers (Middle East Respiratory Syndrome)
- Moderate and Severe Persistent Asthma
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
