Type 1 Diabetes in Children
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is type 1 diabetes?
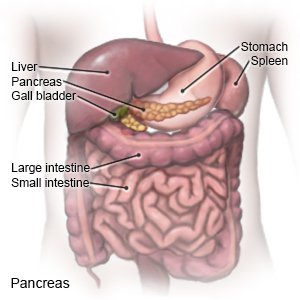
Type 1 diabetes is a disease that affects how your child's body makes insulin and uses glucose (sugar). When the blood sugar level increases, the pancreas should make more insulin. Insulin helps move sugar out of the blood so it can be used for energy. Type 1 diabetes develops because the immune system destroys cells in the pancreas that make insulin. The pancreas cannot make enough insulin, so the blood sugar level continues to rise. A family history of type 1 diabetes may increase your child's risk for diabetes. Type 1 diabetes cannot be cured, but it can be managed.
 |
What are the signs and symptoms of type 1 diabetes?
- More thirst than usual
- Urinating more often or bedwetting
- Feeling hungry most of the time
- Weight loss without trying
How is type 1 diabetes diagnosed?
- An A1c test shows the average amount of sugar in your child's blood over the past 2 to 3 months. An A1c goal for most children is less than 7%. Your child's diabetes care provider may tell you an A1c goal specific to your child. The goal may change as your child gets older.
- A fasting plasma glucose test checks your child's blood sugar level after he or she has fasted for 8 hours. Fasting means he or she has not eaten anything or had anything to drink except water.
- A 2-hour plasma glucose test starts with a blood sugar level check after your child has not eaten for 8 hours. Your child is then given a glucose drink. Your child's blood sugar level is checked after 2 hours.
- A random glucose test may be done any time of day, no matter how long it has been since your child ate.
- Blood tests may be used to check for certain antibodies linked to type 1 diabetes. The amount of insulin your child's body makes may be measured. Genetic tests may be used if your child has a family history of diabetes. Your child may also be checked for other autoimmune disorders, such as celiac disease.
How is type 1 diabetes treated?
The goal is to teach you and your child how to manage diabetes. Management can prevent your child from having complications (health problems) from diabetes.
- Your child will need insulin several times each day. Give your child insulin as directed. Too much insulin may cause his or her blood sugar level to go too low.
- You will be taught how to adjust each insulin dose your child takes with meals. Always check his or her blood sugar level before the meal. The dose will be based on his or her blood sugar level, carbohydrates in the meal, and activity after the meal.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What is diabetes education?
Diabetes education will start right away. Your child will have a diabetes care team. His or her care team may include physicians, nurse practitioners, and physician assistants. It may also include nurses, dietitians, exercise specialists, pharmacists, and a dentist. You, your child, and other family members will also be part of the team. The team will make goals and plans to manage diabetes and other health problems. The plans and goals will be specific to your child's needs. Members of your child's diabetes care team will teach you and your child the following:
- About your child's blood sugar level: You will be given information on when and how to check your child's blood sugar level. Your healthcare provider will help you and your child create a blood sugar level range. The goal is to keep your child's blood sugar within the range so it does not go too high or too low. Write down the times of your child's checks and the levels. Take them to all follow-up appointments.
- A glucose meter is a device that uses a test strip to check your child's blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your child's blood.

- A continuous glucose monitor (CGM) uses a sensor to check your child's blood sugar level. The sensor is placed on your child's abdomen or arm. A transmitter on the sensor gets a glucose reading. CGM data may be linked to an insulin pump. The data will help your child's provider see how much time your child's blood sugar level stayed in range. The provider may recommend nutrition, physical activity, or medicine changes if the levels were often above or below range.

- A glucose meter is a device that uses a test strip to check your child's blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your child's blood.
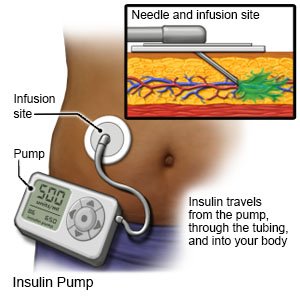
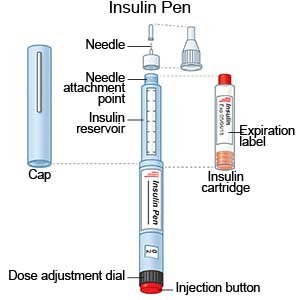
- About insulin: You will learn how much insulin your child needs and when to use it. You will also be taught how to match insulin with blood sugar levels, activity, and carbohydrates. Insulin may be given through a pump or pen, or injected. You, your child, and the diabetes care team will discuss the best method for your child:
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
- An insulin pen is a device prefilled with insulin. Most insulin pens are disposable. You throw the pen away after it is empty or used for a certain amount of time. Some pens have a replaceable cartridge filled with insulin. You keep the pen and only throw away the cartridge.
- Insulin injections are given with a needle and syringe. Your child's provider will tell you if this is the best method for your child. You, your child, and family members will be taught how to draw up and give insulin. You will also be taught how to dispose of used needles and syringes.
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
- About nutrition: A dietitian will help you make a meal plan to keep your child's blood sugar level steady. The plan will be made for your child's and family's needs. You and your child will learn how food affects his or her blood sugar levels. You and your child will meet with the dietitian at least 1 time each year.
- About physical activity and diabetes: You and your child will learn why physical activity, such as exercise, is important. A plan will be made for your child's activity. A goal of 60 minutes of moderate to intense aerobic activity every day will be in the plan. Your child can choose from activities such as brisk walking, dancing, running, or jumping rope. The provider will also recommend flexibility and resistance training as your child gets older. Your child may need to have a snack before activity to prevent low blood sugar levels. Do not allow exercise if your child's blood sugar level is 350 mg/dL or higher. Your child's level may need to be checked before, during, and after exercise.


- About sick day management: Blood sugar levels can be too high or too low when your child is sick. Your child's care team will give you information about managing your child's diabetes during sick days.
- About complications of diabetes: You and your child will learn about complications, such as diabetic ketoacidosis (DKA), neuropathy, and retinopathy. You will learn how to prevent and recognize some of these complications. You will also learn about conditions that may happen with diabetes, such as high blood pressure and high cholesterol.
When do I check my child's blood sugar level?
You will need to check your child's blood sugar level 6 to 10 times each day. Ask your child's care team provider when and how often to check during the day. Before meals , your child's blood sugar level should be between 90 and 130 mg/dL. At bedtime , it should be between 90 and 150 mg/dL. You may need to check for ketones in your child's urine or blood if his or her level is higher than directed. Write down the results and show them to your child's provider. The provider may use the results to make changes to your child's medicine, food, or activity schedules.
Drugs used to treat this and similar conditions
Humalog
Humalog (insulin lispro) is used to treat type 1 (insulin-dependent) diabetes in adults. Includes ...
Lantus
Lantus is a long acting form of insulin used to treat type 1 or type 2 diabetes. Learn about side ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Novolog
NovoLog is a fast-acting insulin used to treat diabetes to control blood sugar levels in adults and ...
Lantus SoloStar
Lantus SoloStar is used for diabetes, type 1, type 2 diabetes
Levemir
Levemir (insulin detemir) is a long acting insulin used to treat diabetes in adults and children ...
NovoLog FlexPen
NovoLog FlexPen is used for diabetes, type 1, diabetic ketoacidosis, nonketotic hyperosmolar ...
Tresiba
Tresiba (insulin degludec) is used to treat diabetes mellitus. Includes Tresiba side effects ...
Apidra
Apidra is used to treat type 1 (insulin-dependent) diabetes in adults. Learn about side effects ...
What should I do if my child's blood sugar level is too low?
- Your child's blood sugar level is too low if it goes below 70 mg/dL. If the level is too low, have your child eat or drink 15 grams of fast-acting carbohydrate. These are found naturally in fruits and dairy products. Fast-acting carbohydrates will raise your child's blood sugar level quickly. Examples of 15 grams of fast-acting carbohydrate include the following:
- 4 ounces (½ cup) of fruit juice or 4 ounces of regular soft drink
- 2 tablespoons of raisins
- A tube of glucagon gel or 3 to 4 glucose tablets
-
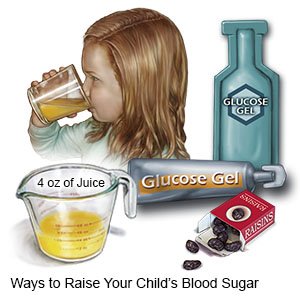
- Check your child's blood sugar level 15 minutes later. If the level is still low (less than 100 mg/dL), give another 15 grams of carbohydrate. When the level returns to 100 mg/dL, have your child eat a snack or meal that contains carbohydrate and protein. This will help prevent another drop in blood sugar. Always carefully follow your child's care team provider's instructions on how to treat low blood sugar levels.
What do I need to know about nutrition for my child?
A dietitian will help you and your child create a meal plan. The plan will help keep your child's blood sugar level steady. The plan may change as your child grows and wants different foods. Do not let your child skip meals. Your child's blood sugar level may drop too low if he or she takes insulin and does not eat.
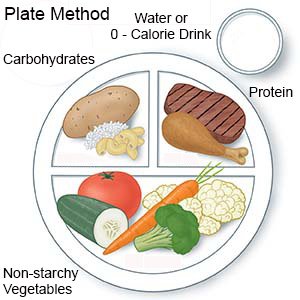 |
- Keep track of carbohydrates (sugar and starchy foods). Your child's blood sugar level can get too high if he or she eats too many carbohydrates. The dietitian will help you plan meals and snacks that have the right amount of carbohydrates.
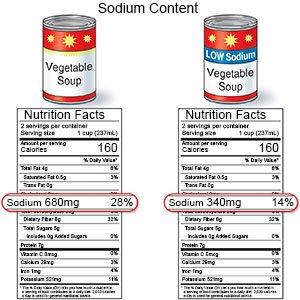
- Give your child low-fat and low-sodium foods. Examples of low-fat foods are lean meat, fish, skinless chicken or turkey, and low-fat milk. Limit high-sodium foods, such as potato chips and soup. Do not add salt to food you cook. Limit your child's use of table salt.
- Give your child high-fiber foods. Foods that are a good source of fiber include vegetables, whole-grain bread, and beans.

What else can I do to help my child manage type 1 diabetes?
- Talk to your child's care team provider if you or your child become stressed about diabetes care. Learning about diabetes care can be stressful. The stress can cause your child not to want to help in his or her own care. The stress can also cause you to feel overwhelmed. Your child's provider can help by offering tips about self-care. The provider may suggest you and your child talk to a mental health provider. He or she can listen and offer help with self-care issues and feelings of being overwhelmed. You and your child may choose to see the mental health provider at separate times or together.
- Make sure your child always wears medical alert jewelry or carries a card that says he or she has diabetes. Ask your child's provider where to get these items.

- Give instructions to your child's school and care providers. Make sure your child's teachers and care providers know he or she has diabetes. Provide written instructions about what to do if your child has symptoms of high or low blood sugar levels.
- Do not smoke around your child. Do not let others smoke around him or her. Do not let your older child smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Cigarette smoke can worsen diabetes problems. Ask your child's provider for information if you or your child currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to the provider before you or your child use these products.
- Get your child's eyes checked as directed. Your child will need an eye exam every 1 to 2 years. The provider will check for changes in your child's sight. He or she will also check for retinopathy (damage to the retina). Your child is at risk for retinopathy when puberty starts and after having type 1 diabetes 5 to 10 years.
- Bring your child in for screenings as directed. Your child will need to be screened for complications of diabetes and other conditions that may develop. Examples include kidney problems, high cholesterol, high blood pressure, blood vessel problems, eye problems, and eating disorders. Some screenings may begin right away and some may happen within the first 5 years of diagnosis. Your child will need to continue screenings through his or her lifetime. Keep your child's follow-up appointments with all providers.
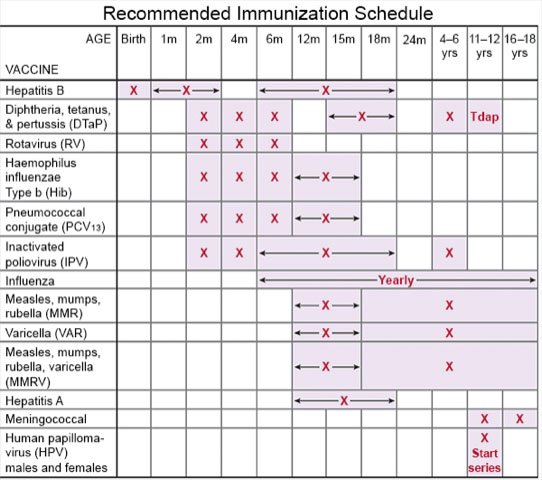
- Ask about vaccines your child may need. Your child has a higher risk for serious illness if he or she gets the flu, COVID-19, or pneumonia. Ask if your child should get vaccines to prevent these or other diseases, and when to get the vaccines.
- Talk to your child's provider about weight loss medicines, if needed. Certain medicines are given along with insulin to children 10 years or older who have obesity or overweight. These medicines are not used to lower blood sugar, but your child's level may decrease from weight loss. The provider will tell you how long your child should continue the medicine after reaching a healthy weight.
What can happen if my child's diabetes is not controlled?
Diabetes that is not controlled can damage your child's nerves and arteries. Long-term high blood sugar levels can damage his or her eyes and kidneys. Your child may develop thyroid disease. Diabetes is life-threatening if it is not controlled. Help your child control his or her blood sugar levels to lower the risk for health problems.
When should I call my child's diabetes care team provider immediately?
- Your child has a low blood sugar level and it does not improve with treatment.
- Your child's blood sugar level is above 240 mg/dL and does not come down after a dose of insulin.
- Your child has ketones in his or her urine or blood.
- Your child has a fever.
- Your child has nausea or is vomiting and cannot keep any food or liquid down.
- Your child has symptoms of a low blood sugar level, such as trouble thinking, sweating, or a pounding heartbeat.
- Your child has blurred or double vision.
- Your child's breath has a fruity, sweet smell, or his or her breathing is deep and labored.
- Your child's heartbeat is fast and weak.
When should I call my child's doctor or care team provider?
- Your child's blood sugar levels are higher than his or her target goals.
- Your child often has low blood sugar levels.
- Your child has abdominal pain, diarrhea, or is vomiting.
- Your child has numbness in his or her arms or legs.
- Your child has warm, red patches of skin or a wound that does not heal.
- Your child gets easily irritated.
- Your child is anxious or depressed.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Type 1 Diabetes
- Diabetes Medications and Alcohol Interactions
- OneTouch Blood Glucose Meters
- Top 10 Diabetes Treatments You May Have Missed
Treatment options
Care guides
- Diabetes and your Skin
- Diabetic Hyperglycemia
- How to Draw Up Insulin
- Type 1 Diabetes in Adults: New Diagnosis
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
