Syncope in Older Adults
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is syncope?
Syncope is also called fainting or passing out. Syncope is a sudden, temporary loss of consciousness, followed by a fall from a standing or sitting position. A syncope episode is usually short.
What causes or increases my risk for syncope?
Syncope is caused by a decrease in blood flow to the brain. When blood flow to the brain decreases, oxygen to the brain also decreases. Any of the following conditions may cause syncope:
- Medicines such as blood pressure medicine or antidepressants, or use of multiple medicines
- A medical condition such as severe anemia, a nerve disorder, asthma, or hyperventilation (breathing too quickly)
- A heart condition, such as a narrow artery or an irregular heartbeat
- Dehydration
- Problems with the blood vessels of your brain
- Bleeding, especially in your stomach or intestines, or a blood clot that passes through your lungs
- A rapid drop in blood pressure after a body position change, such as moving from lying to sitting or standing
- Straining during bowel movements, a cough or sneeze, or a stressful or fearful situation
What signs and symptoms may occur before syncope?
- Cold, clammy, and sweaty skin
- Fast breathing and a racing, pounding heartbeat
- Feeling more tired than usual
- Nausea, a warm feeling, sweating, and lightheadedness
- A headache or dizziness
- Tingling sensation or numbness
- Spots in front of your eyes, blurred vision, or double vision
How is the cause of syncope diagnosed?
Your healthcare provider will examine you and ask about your symptoms. Tell your provider everything you know about your syncope episode. Include where you were when you fainted and what you were doing before symptoms started. Your provider will ask about your medical history, including any heart conditions in your family. Ask anyone who saw you faint to come with you to tell the provider details of what happened. Your provider may order the following tests to find out what is causing your symptoms:
- Blood tests may be done to find the cause of your syncope.
- Telemetry is continuous monitoring of your heart rhythm. Sticky pads placed on your skin connect to an EKG machine that records your heart rhythm.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your heart.
- A stress test may show the changes that take place in your heart while it is under stress. Stress may be placed on your heart with exercise or medicine. Ask for more information about this test.
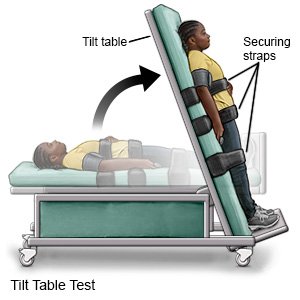
- A tilt table test is used to check your heart and your blood pressure when you change positions.
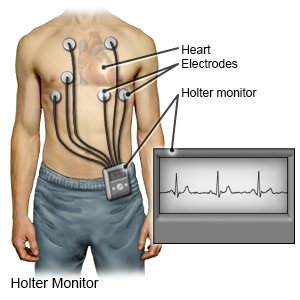
- A Holter monitor is also called a portable electrocardiography (EKG) monitor. It shows your heart's electrical activity while you do your usual activities. The monitor is a small battery-operated device that you wear. It will show how fast your heart beats and if it beats in a regular pattern. Your provider may recommend this if you have syncope often over 2 to 3 days.
How is syncope treated?
Treatment depends on the cause of your syncope. To prevent syncope from happening again, you may need any of the following:
- Medicines may be needed to help your heart pump strongly and regularly. Your healthcare provider may also make changes to any medicines that are causing syncope.
- Tilt training involves training yourself to stand for 10 to 30 minutes each day against a wall. This helps your body decrease the effects of posture changes and reduces the number of fainting spells.
What can I do to manage syncope?
- Keep a record of your syncope episodes. Include your symptoms and your activity before and after the episode. The record can help your healthcare provider find the cause of your syncope and help you manage episodes.
- Sit or lie down when needed. This includes when you feel dizzy, your throat is getting tight, and your vision changes. Raise your legs above the level of your heart. Your provider may also recommend that you keep the head of your bed elevated. This can help keep your blood pressure from dropping too low.
- Check your blood pressure often. This is important if you take medicine to lower your blood pressure. Check your blood pressure when you are lying down and when you are standing. Ask how often to check during the day. Keep a record of your blood pressure numbers. Your provider may use the record to help plan your treatment.

- Use assistive devices as directed. Your provider may suggest that you use a cane or walker to help you keep your balance. You may need to have grab bars put in your bathroom near the toilet or in the shower.
What can I do to prevent a syncope episode?
- Know and avoid your triggers. Certain events may bring on syncope. These events may cause you to feel under pressure, upset, or fearful. When you feel the symptoms, you can make movements to prevent a syncope episode. For example, make a fist, cross your legs, squeeze your thighs together, or tighten your arm muscles.
- Move slowly and let yourself get used to one position before you move to another position. This is very important when you change from a lying or sitting position to a standing position. Take some deep breaths before you stand up from a lying position. Stand up slowly. Sudden movements may cause a fainting spell. Sit on the side of the bed or couch for a few minutes before you stand up. If you are on bedrest, try to be upright for about 2 hours each day, or as directed. Do not lock your legs if you are standing for a long period of time. Move your legs and bend your knees to keep blood flowing.
- Follow your healthcare provider's recommendations. Your provider may recommend that you drink more liquids to prevent dehydration. You may also need to have more salt to keep your blood pressure from dropping too low and causing syncope. Your provider will tell you how much liquid and sodium to have each day. Your provider will also tell you how much physical activity is safe for you. This will depend on what is causing your syncope.
- Watch for signs of low blood sugar. These include hunger, nervousness, sweating, and fast or fluttery heartbeats. Talk with your provider about ways to keep your blood sugar level steady.
- Do not strain if you are constipated. You may faint if you strain to have a bowel movement. Walking is the best way to get your bowels moving. Eat foods high in fiber to make it easier to have a bowel movement. Good examples are high-fiber cereals, beans, vegetables, and whole-grain breads. Prune juice may help make bowel movements softer.

- Be careful in hot weather. Heat can cause a syncope episode. Limit activity done outside on hot days. Physical activity in hot weather can lead to dehydration. This can cause an episode.
Drugs used to treat this and similar conditions
Orvaten
Orvaten is used for dysautonomia, hypotension, postural orthostatic tachycardia syndrome
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Northera
Northera (droxidopa) is used to treat neurogenic orthostatic hypotension. Includes Northera side ...
Call your local emergency number (911 in the US) or have someone call if:
- You suddenly have double vision, trouble speaking, numbness, and cannot move your arms or legs.
- You have chest pain and trouble breathing.
When should I seek immediate care?
- You are bleeding because you accidently hit your head after fainting.
- You vomit blood or material that looks like coffee grounds.
- You see blood in your bowel movement.
When should I call my doctor?
- You have another fainting spell.
- You have a headache, fast heartbeat, or feel too dizzy to stand up.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
