Right Hemispheric Stroke
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a right hemispheric stroke?
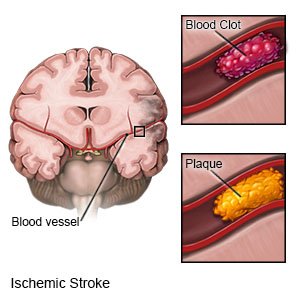
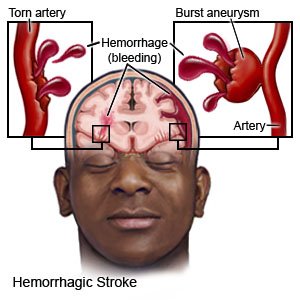
A right hemispheric stroke happens when blood cannot flow to the right hemisphere (side) of your brain. A stroke caused by a blood clot is called an ischemic stroke. A stroke caused by a burst or torn blood vessel is called a hemorrhagic stroke. A stroke is a medical emergency that needs immediate treatment.
 |
 |
What are the warning signs of a stroke?
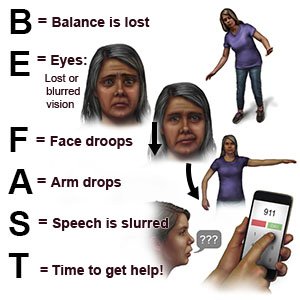
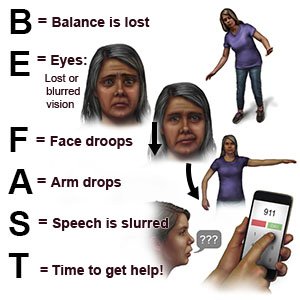
The words BE FAST can help you remember and recognize warning signs of a stroke:
- B = Balance: Sudden loss of balance
- E = Eyes: Loss of vision in one or both eyes
- F = Face: Face droops on one side
- A = Arms: Arm drops when both arms are raised
- S = Speech: Speech is slurred or sounds different
- T = Time: Time to get help immediately
 |
What are the signs and symptoms of a right hemispheric stroke?
The right hemisphere of your brain controls the left side of your body. It may also affect your speech and language abilities. You may also have any of the following:
- Trouble remembering, impulsive behavior, or mood changes
- Trouble paying attention or solving problems
- Paralysis or weakness on the left side of your body
- Loss of vision in one or both eyes
- Trouble walking, or falling toward your left side
- Not knowing how close an object is to your body
- Lack of awareness of the left side of your body
- Trouble swallowing, speaking, reading, writing, or understanding language
What increases my risk for a right hemispheric stroke?
- Age 55 or older
- A family history of stroke
- Not enough physical activity or obesity
- High cholesterol, high blood pressure, or diabetes
- Smoking cigarettes or using illegal drugs
- A heart condition such as atrial fibrillation, myocardial infarction, or valve disease
- Oral birth control pills, especially in women older than 35 who smoke cigarettes
- Hormone replacement therapy
How is a right hemispheric stroke diagnosed?
Your healthcare provider will examine you and ask about your symptoms and when they started. He or she will ask if you have any medical conditions. You may need any of the following:
- Blood tests may be used to check how well your blood clots or to check your blood sugar level.
- CT or MRI pictures may show where the stroke happened and any damage to your brain. You may be given contrast liquid to help your skull and brain show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- An arteriography is used to take x-rays of your arteries to look for blood flow blockage.
How is a right hemispheric stroke treated?
Treatment depends on the type of stroke you had. You may need any of the following:
- Medicines may help improve your blood's ability to clot and stop the bleeding. You may instead need medicine to break up blood clots, or to prevent them from forming. Healthcare providers will talk to you or your family members about the risks and benefits of each medicine. You may also need medicine to treat pain, high blood pressure, high cholesterol, or diabetes.
- Thrombolysis is a procedure used to break apart clots in an artery. A catheter is guided into the artery until it is near the clot. Medicine is put through the catheter that will help break apart the clot. The clot may be pulled out of the artery during the procedure.
- Surgery may be used to remove a blood clot or to relieve pressure within your brain. You may also need surgery to remove plaque buildup from your carotid arteries. Surgery may instead be needed to stop the bleeding or remove blood that has leaked out of the blood vessels.
Drugs used to treat this and similar conditions
Benicar
Benicar is used to treat high blood pressure (hypertension). Learn about side effects, interactions ...
Cozaar
Cozaar (losartan) is used to treat high blood pressure (hypertension). Includes Cozaar side ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Toprol-XL
Toprol-XL (metoprolol) is a beta-blocker used to treat angina and high blood pressure. Includes ...
Spironolactone
Spironolactone is a potassium-sparing diuretic that is primarily used to treat heart failure, high ...
Valsartan
Valsartan is an angiotensin II receptor blocker (ARB) that may be used to treat high blood pressure ...
Hydrochlorothiazide/lisinopril
Hydrochlorothiazide/lisinopril systemic is used for heart failure, high blood pressure
Diovan
Diovan is used to treat high blood pressure (hypertension) or heart failure. Learn about side ...
Carvedilol
Carvedilol (Coreg) is used to treat heart failure and hypertension (high blood pressure). Includes ...
Furosemide
Furosemide is a loop diuretic used to treat fluid retention and high blood pressure by increasing ...
What can I do to care for myself after a stroke?
- Go to stroke rehabilitation (rehab) as directed. Rehab is a program run by specialists who will help you recover abilities you may have lost. Specialists include physical, occupational, and speech therapists. Physical therapists help you gain strength or keep your balance. Occupational therapists teach you new ways to do daily activities. Your therapy may include movements for everyday activities. An example is being able to raise yourself from a chair. A speech therapist helps you improve your ability to talk and swallow.
- Make your home safe. Remove anything you might trip over. Tape electrical cords down. Keep paths clear throughout your home. Make sure your home is well lit. Put nonslip materials on surfaces that might be slippery. An example is your bathtub or shower floor. A cane or walker may help you keep your balance as you walk.

What do I need to know about depression?
Talk to your healthcare provider if you have depression that continues or is getting worse. Your provider may be able to help treat your depression. Your provider can also recommend support groups for you to join. A support group is a place to talk with others who have had a stroke. It may also help to talk to friends and family members about how you are feeling. Tell your family and friends to let your healthcare provider know if they see any signs of depression:
- Extreme sadness
- Avoiding social interaction with family or friends
- A lack of interest in things you used to enjoy
- Irritability
- Trouble sleeping
- Low energy levels
- A change in eating habits or sudden weight gain or loss
How can I lower my risk for another stroke?
- Manage health conditions. A condition such as diabetes can increase your risk for a stroke. Control your blood sugar level if you have hyperglycemia or diabetes. Take your prescribed medicines and check your blood sugar level as directed.

- Check your blood pressure if directed. High blood pressure can increase your risk for a stroke. Follow your healthcare provider's directions for controlling your blood pressure.

- Eat a variety of healthy foods. Healthy foods include whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Eat at least 5 servings of fruits and vegetables each day. Choose foods that are low in fat, cholesterol, salt, and sugar. Eat foods that are high in potassium, such as potatoes and bananas. A dietitian can help you create healthy meal plans.

- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan, if needed. He or she can help you create small goals if you have a lot of weight to lose.
- Exercise as directed. Exercise can lower your blood pressure, cholesterol, weight, and blood sugar levels. Healthcare providers will help you create exercise goals. They can also help you make a plan to reach your goals. For example, you can break exercise into 10 minute periods, 3 times in the day. Find an exercise that you enjoy. This will make it easier for you to reach your exercise goals.
- Do not drink alcohol. Alcohol can increase your risk for a stroke. Alcohol may also increase your blood pressure or thin your blood. Blood thinning can increase your risk for hemorrhagic stroke.
- Do not use nicotine products or illegal drugs. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage. Nicotine and illegal drugs both increase your risk for a stroke. Ask your healthcare provider for information if you currently smoke or use drugs and need help to quit. E- cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Where can I find support and more information?
- American Stroke Association
Phone: 1- 888 - 478-7653
Web Address: http://www.stroke.org
Call your local emergency number (911 in the US) or have someone else call if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
-
- You have a seizure.
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have loss of balance or coordination.
- You have double vision or vision loss.
- You have unusual or heavy bleeding.
- You have trouble swallowing.
When should I call my doctor?
- Your blood pressure or blood sugar level is higher or lower than you were told it should be.
- You have trouble having a bowel movement or urinating.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
