Primary Ciliary Dyskinesia in Children
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is primary ciliary dyskinesia (PCD)?
PCD is a disorder that affects the cilia in your child's body. Cilia are hair-like structures around cells that normally move like waves. Cilia in the lungs, ears, and sinuses normally carry mucus out. When mucus cannot be carried out, it sits in your child's airway. Bacteria in the mucus increase, leading to lung infections or respiratory failure. Your child may have fertility problems (trouble having children) later in life. PCD can keep certain parts of the reproductive system from working correctly. PCD is a genetic disorder (passed from both parents to the child).
What are the signs and symptoms of PCD?
- Respiratory distress in newborns
- Respiratory infections that start early in life and continue into adulthood
- Daily, year-round cough that produces mucus, and congestion in your child's sinuses
- In young children, pneumonia that happens more than one time, and damage to the airways
- Painful ear infections that may include fluid draining from the ear (usually before 13 years old)
- Hearing problems from fluid in the ears and ear infections, or abnormal sinuses
- Abdominal organs that are on the opposite side of the body than usual, more than 1 spleen, or no spleen
- Congenital heart disease
How is PCD diagnosed?
Your child's healthcare provider will ask about your child's signs and symptoms and when they began. PCD might be diagnosed based on your child's signs and symptoms. Examples are a constant cough or infections that antibiotics do not clear up. Tell your child's provider if he or she had respiratory distress as a newborn. Some conditions can look like PCD, such as cystic fibrosis. Children are sometimes given tests to rule this out. Tests may be available to help confirm PCD:
- Nasal nitric oxide (NO) measurement is a test to find the amount in your child's body. PCD can cause the NO level to be lower than normal.
- Transmission electron microscopy is sometimes used to find any problems with the cilia that can prevent them from moving correctly. Cells that have cilia are taken from inside your child's nose or airway.
- CT scan or x-ray pictures may show a lung infection or other lung problem.
- Genetic testing may be used to check for genes that cause PCD.
How is PCD treated?
PCD cannot be cured, but treatment can help your child control signs and symptoms.
- Medicine may be used to help fight or prevent an infection caused by bacterial, or to help thin mucus. Medicines to open your child's airway or lower inflammation may be given if he or she has asthma along with PCD. Do not give your child cough suppressants (medicine to prevent coughing). It is important that your child cough out mucus and irritants to prevent respiratory infections.
- An incentive spirometer helps your child take slow, deep breaths to expand and fill his or her lungs with air. For younger children, jumping and blowing games can help with breathing.
- Chest physiotherapy (CPT) helps loosen mucus. During CPT, a healthcare provider lightly claps on your child's back and chest with his or her hands. This brings up mucus from the lungs and makes it easier to cough up.
- Suction may be used to help remove mucus that your child is not able to cough up.
- Oxygen may be given to help your child breathe easier. Oxygen can also decrease the strain on your child's heart and help prevent more problems.
- Sinus surgery may be used to drain your child's sinuses.
What can I do to manage my child's symptoms?
Tell your child's healthcare provider right away when he or she has signs of a respiratory infection. Early treatment may help control the infection so it does not become severe. The following can help you and your child manage PCD and protect his or her airway:
- Take your child to pulmonary rehabilitation (rehab) as directed. Pulmonary rehab is a program that can help your child learn how to prevent breathing problems. The rehab team includes lung and ear, nose, and throat specialists, and respiratory therapists. The team will help your child create an aerobic exercise plan. Aerobic exercise is one of the best ways to manage PCD. Exercises such as walking, swimming, or riding a bicycle help strengthen your child's heart and lungs. The rehab program will change as your child gets older and becomes responsible for his or her own care.
- Keep your child's airway clear and open. Have your child do airway clearance techniques as needed. Healthcare providers will show your child how to do these in pulmonary rehab. Help thin mucus by having your child drink more liquids or use a cool mist humidifier.
- Prevent infections. Keep your child away from people who are sick. Have your child wash his or her hands often. Use soap and water, or a gel hand sanitizer if soap and water are not available.

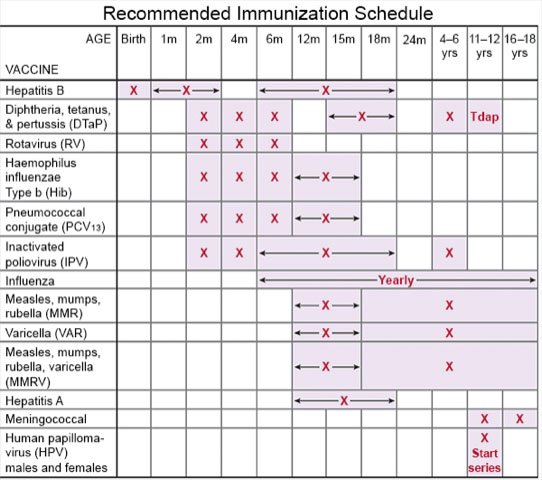
- Talk to your child's healthcare provider about vaccines. Children get vaccines on a regular schedule. Your child's provider can help you schedule catch-up doses if your child has not received all the recommended vaccines. Take your child to get a flu vaccine every year as soon as it becomes available. Your child may also need a vaccine to help prevent pneumonia.
- Do not smoke around your child or let others smoke around him or her. Do not let your adolescent smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage and make breathing problems worse. Ask your adolescent's healthcare provider for information if he or she currently smokes and needs help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to healthcare providers before he or she uses these products.
Call your local emergency number (911 in the US) if:
- Your child has sudden chest pain.
- Your child has sudden or more severe trouble breathing.
- Your child is confused or feels faint.
When should I call my child's pediatrician?
- Your child's lips or fingernails turn gray or blue.
- Your child coughs up blood.
- Your child has a fever.
- Your child coughs more than usual or wheezes.
- Your child's medicines do not relieve his or her symptoms.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
