Pancreatic Islet Cell Autotransplantation
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about pancreatic islet cell autotransplantation?
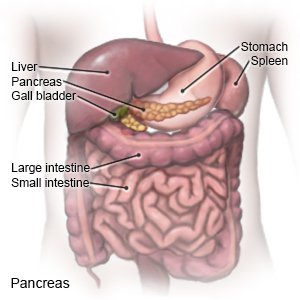
A total pancreatectomy and auto islet transplant is surgery for chronic pancreatitis. Chronic pancreatitis causes abdominal pain that affects your quality of life. The pancreas contains clusters of cells called islets. Certain islet cells produce insulin, a hormone that lowers blood glucose (sugar) so the amount does not get too high. Islet cell autotransplantation is used to keep your islet cells so you will not develop brittle diabetes. Brittle diabetes means your blood glucose level swings between too high and too low. Another name for this surgery is autologous islet transplantation. Autologous means the transplanted tissue comes from your body instead of from a donor. Your immune system will not reject the tissue because it is from your body.
 |
How do I prepare for surgery?
- You will meet with a team of specialists before surgery. The team will help you be ready to care for yourself at home. A gastroenterologist will manage your digestive tract. An endocrinologist will manage your islet cells. A dietitian will help you with nutrition. A pain management specialist will help you stop using pain medicine safely. Your doctor is also part of your team. He or she will manage your overall health. You will continue to meet with your diabetes management team after surgery.
- You will get diabetes management education before surgery. The purpose of education is to make sure you know how to manage your blood glucose levels. You can develop serious health problems if your blood glucose level gets too high or too low. Your healthcare providers will tell you what your levels should be. You will be given information on when to check your levels. You will learn what to do if your level is too high or too low.
- Your surgeon will tell you how to prepare for surgery. Tell your surgeon about all medicines you take. Include over-the-counter medicines, vitamins, and herbal medicines. You may need to stop taking some medicines days or weeks before surgery. Examples include blood thinners and NSAID pain medicine. Tell your surgeon if you have ever had an allergic reaction to anesthesia or antibiotics.
- You may be told not to eat or drink anything after midnight on the night before surgery. Your surgeon will tell you which medicines to take or not take on the day of surgery. Your surgeon will tell you how long you may need to stay in the hospital after surgery. It is common to stay for about a week.
Related medications
What will happen during surgery?
- You will be given general anesthesia to keep you asleep and pain-free during surgery. You will be given insulin through your IV during surgery. A nasogastric (NG) tube will be guided into your nose and down to your stomach. The tube keeps fluid out of your stomach during surgery. A Foley catheter will be guided into your bladder through your urethra. The catheter keeps urine out of your bladder during surgery.
- Your surgeon will make an incision in your abdomen. He or she will remove your pancreas. You will stay in the operating room while the pancreas is taken to the lab. Islet clusters will be separated from your pancreas. This procedure takes 2 to 4 hours. The cells are placed in an IV bag that is taken back to the operating room. The islets are then injected back to you through the portal vein. The islets will graft onto your liver over the next few months.
What should I expect after surgery?
- You will be taken to the intensive care unit (ICU) to be monitored after surgery.
- It is normal to have some discomfort or pain in the surgery area. You may also have pain at your right shoulder tip if your diaphragm is irritated during surgery. Medicine may be used to control your pain.
- Healthcare providers may want you to walk around as soon as possible after surgery. This will help prevent blood clots. They will help you safely stand up and walk.
- You may have a jejunostomy tube (J-tube) for tube feeding until you can start eating. A J-tube is put through the skin of your abdomen and into your small intestine.
- You may continue to get insulin through your IV until you are ready to start eating again. Then you will start having insulin injections.
- The first 8 weeks after your islet transplant are especially critical to your islet cells. The cells will make a home (engraft) within your liver during this time. Healthcare providers will check your blood glucose levels often. It is critical to control blood glucose levels in the first few weeks after islet transplantation.
What are the risks of this surgery?
You may bleed more than expected during surgery, or while you are recovering. You may also develop an infection. A blood clot may develop in your portal vein. Your transplanted islet cells may not produce enough insulin to control your blood glucose levels. You will need to keep taking insulin injections if this happens. You will need to take insulin for the rest of your life if your body cannot produce enough.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
