Long Covid
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
Long COVID
is a term used to describe ongoing effects of COVID-19 infection. Signs and symptoms are considered long COVID if they begin or continue at least 4 weeks after the infection. Experts believe the immune system in some people overreacts to the virus that causes COVID-19. The immune system attacks the virus, but it also attacks healthy nerves, blood vessels, and organs. It is not yet known how long symptoms could continue. Anyone who had COVID-19 can develop long COVID, even if symptoms were mild or never developed at all. Long COVID may also be called post-COVID conditions, post-acute COVID, or chronic COVID. Long-term effects caused by the virus may also be called post-acute sequelae of SARS-CoV-2 (PASC).
Signs and symptoms of long COVID
may happen sometimes or all the time. Some may get better and then return or worsen later. Some may be worse with physical or mental activities. You may have any of the following:
- Fatigue (feeling mentally and physically tired), trouble being as physically active as before, or trouble sleeping
- Headaches, dizziness, or brain fog (trouble concentrating, or being forgetful or confused)
- Chest pain, a fast or pounding heartbeat, a cough, or shortness of breath
- Joint or muscle pain
- Changes from feeling hot to feeling cold that happen often
- Depression, anxiety, or mood swings
- Not being able to smell or taste anything
- A skin rash, especially on your toes
- A fever that does not get better with medicine or returns several times
- Blood clots
- Hallucinations or paranoia
Call your local emergency number (911 in the US) if:
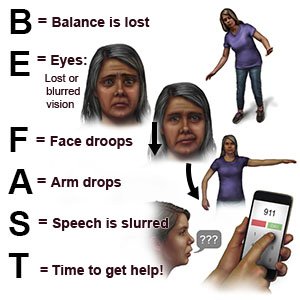
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have a seizure (and do not have a known seizure disorder).
- You are confused.
- You have sudden trouble breathing, or you cough up blood.
- Your legs start to feel numb, or you have trouble moving them.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You feel short of breath even at rest.
- You have newly weak muscles.
- You have vision or hearing changes.
Call your doctor or specialist if:
- You have a fever.
- You have questions or concerns about your condition or care.
Treatment:
No specific treatment is available for long COVID. Your healthcare provider may recommend any of the following, depending on your symptoms:
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Antibiotics help prevent or treat a bacterial infection.
- Deep breathing exercises can help improve your oxygen levels.
- A sniff board may help if you lost the ability to smell. The board has several oils on it. You breathe in deeply through your nose to help your sense of smell return. Loss of smell is usually a temporary effect of long COVID. The sniff board may help the sense come back faster.
- Taste stimulation or retraining may help if you lost the ability to taste. You will be given strong flavors to help your sense of taste return.
Manage your symptoms:
- Rest as needed. Take naps and change your schedule to fit your energy level. You may need to take 5 to 10 minute rest periods every hour or more. Try to go to bed and wake up at the same times every day.
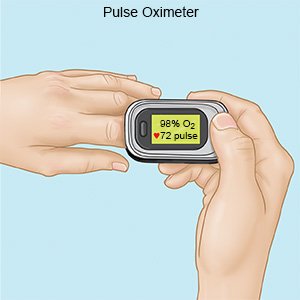
- Manage any other health conditions you have. Some health conditions can cause symptoms that are similar to COVID-19 or that can make other symptoms worse. For example, an asthma or COPD exacerbation can cause breathing problems that may worsen long COVID breathing problems. You may need to check your blood oxygen level with a device called a pulse oximeter. The device shows your heart rate and the percentage of oxygen in your blood. Your healthcare provider can tell you how often to check during the day.
- Ask about vaccines you may need. Get the influenza (flu) vaccine as soon as recommended each year, usually starting in September or October. Get the pneumonia and respiratory syncytial virus (RSV) vaccines, if recommended. Get an updated COVID-19 vaccine, as directed. Your healthcare provider can tell you if you should also get other vaccines, and when to get them.
- Eat a variety of healthy foods. Healthy foods include vegetables, fruit, lean meat, poultry, fish, low-fat dairy, nuts, whole-grain breads, and cooked beans. Talk to your healthcare provider if you have a loss of appetite or any problems eating. Your provider or a dietitian can help you create healthy meals and snacks.

- Be as physically active as you are able to be. Light physical activity, such as walking, can help with many symptoms. For example, activity can help your lungs work better, improve your sleep, and relieve depression or anxiety. Start with light activity most days of the week. You can work up to more activity as you feel better. Talk to your healthcare provider if you do not feel able to get any physical activity. Your provider may recommend that you work with a physical or occupational therapist. A physical therapist can help you work up to more activity. An occupational therapist can help you plan activities around your symptoms.
- Keep a record of your activities and symptoms each day. This record will help you learn when you have the most energy. You will also be able to follow your progress. Bring this record with you to your follow-up visits.
- Get support. Ask your healthcare provider about support groups in your area. A support group is a place to talk with others who also have long COVID. You can talk about your feelings and get advice for managing symptoms. Talk therapy with a mental health professional can also help you and your family members manage the stress of long COVID.
- Limit or do not drink alcohol. Ask your healthcare provider if it is okay for you to drink any alcohol. Your provider can help you set limits for the number of drinks you have in 24 hours and in a week. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Do not smoke. Nicotine and other chemicals in cigarettes can damage your heart and lungs. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Follow up with your doctor as directed:
You may need to come in for ongoing tests or treatment. Your doctor may also refer you to a specialist. The specialist will depend on your symptoms and the affected areas of your body. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
