Enterocele
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is an enterocele?
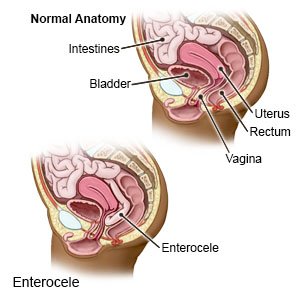
An enterocele happens when part of your small intestine falls down and bulges into your vagina. Weak or stretched muscles in the pelvis allow the intestine to prolapse (fall out of place). An enterocele may also be called a vaginal hernia or a small bowel prolapse.
 |
What increases my risk for an enterocele?
- A hysterectomy or other pelvic surgery
- Pregnancy and childbirth
- Lower estrogen levels from older age or menopause
- Anything that strains your pelvic muscles, such as obesity, chronic constipation, severe coughing, or lifting heavy objects
- Pressure in the pelvic area from a prolapsed bladder, rectum, or uterus
What are the signs and symptoms of an enterocele?
- Low back pain or a pulling feeling in your pelvis that gets better when you lie down
- Fullness, pressure, or pain in your pelvis
- A bulge in your vagina
- Trouble having a bowel movement, chronic constipation, or leaking bowel movement
- Discharge and bleeding from your vagina that is not your monthly period
- Pain or discomfort during sex
How is an enterocele diagnosed?
Your healthcare provider will ask about your medical history and symptoms. You may need any of the following:
- A pelvic exam is used to help find an enterocele. Your provider will examine your vagina and rectum and check your pelvis for any changes. Your provider may ask you to tighten the muscles of your pelvis as if you are trying to stop urinating. This helps find how strong your pelvic muscles are. Your provider may ask you to bear down as if you are having a bowel movement. This will help your provider see where the prolapse is and measure it.
- Defecography shows changes taking place in your rectum and muscles during a bowel movement. A thick paste of barium is placed into your rectum through your anus. X-rays are taken while you push out the barium as if you are having a bowel movement. The barium makes an x-ray outline of your rectum and anus.
How is an enterocele treated?
- Observation may be recommended if the enterocele is not severe. Observation means the enterocele will be checked over time. Treatment may change if the enterocele gets worse or interferes with your quality of life.
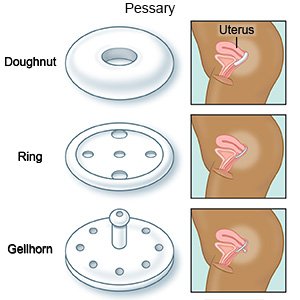
- A pessary can be placed inside the vagina to support the bulging tissues in your vagina. A pessary is a plastic or rubber ring.
- Surgery may be needed to fix the prolapse. You may have surgery to repair stretched or torn vaginal tissues. Your healthcare provider may use a mesh patch or a tissue graft to support or hold the repair.
What can I do to manage or prevent an enterocele?
- Sit with your legs elevated. This can help relieve pain or discomfort. Put pillows or blankets under your lower legs to elevate your entire legs. Do not stand for long periods of time.
- Prevent pressure in your abdomen. Do not strain when you have a bowel movement. Do not lift heavy objects. Talk to your healthcare provider about treatment for a chronic cough. Vaping or smoking can cause or worsen a chronic cough. Ask your provider for information if you currently smoke or vape and need help to quit.
- Do Kegel exercises. These exercises strengthen the muscles that hold your uterus in place. They also tighten the muscles you use when you urinate or have a bowel movement. Tighten muscles in your pelvis (muscles you use to stop urinating). Hold the muscles tight for 5 seconds, then relax for 5 seconds. Gradually work up to holding the muscles contracted for 10 seconds. Do at least 3 sets of 10 repetitions a day.
- Maintain a healthy weight. Ask your healthcare provider for a healthy weight for you. Your provider can help you create a weight loss plan, if needed. Your provider can also help you create a physical activity plan. Physical activity, such as exercise, helps your bowels work better and decreases pressure inside your colon.
- Eat more fiber. High-fiber foods, such as fruits, vegetables, and whole grains, soften bowel movements. This helps bowel movements pass more quickly through your colon. Your provider may also recommend medicines to make it easier to have a bowel movement, or to make them more regular.

- Drink liquids as directed. Ask your provider how much liquid to drink each day and which liquids are best for you. Liquids will help decrease constipation so you will not strain to have a bowel movement.
When should I seek immediate care?
- You have a mass bulging out of your vagina that you cannot push back into place.
- You vomit more than 2 times in a day.
- Your bowel movement is bright red or black.
When should I call my doctor?
- Your pessary falls out.
- You have heavier vaginal bleeding than usual.
- You are not able to have a bowel movement.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
