Cystic Fibrosis in Children
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is cystic fibrosis (CF)?
CF is a lifelong condition that affects your child's lungs, digestive system, and other organs. Mucus, tears, sweat, and saliva become so thick and sticky that they clog the lungs and digestive system. CF typically causes problems with breathing and with breaking down and absorbing food.
What are the signs and symptoms of CF?
The first sign of CF in your newborn is that he or she is not able to have a bowel movement. Your child may often have respiratory infections, such as sinusitis, bronchitis, or pneumonia. He or she may also have any of the following:
- Skin that tastes salty when you kiss him or her
- A cough, wheezing, and shortness of breath that happen often
- Weight loss or failure to gain weight
- Clubbing of fingers or toes (become large, blunt, and rounded)
- Abdominal pain
How is CF diagnosed?
Your child's healthcare provider will ask if anyone in your family has CF. CF is a genetic disorder. The provider will also ask about your child's symptoms. Your child may need any of the following tests:
- A sweat chloride test shows the amount of chloride in your child's sweat. The amount of chloride will be high if he or she has CF.
- Blood tests may be used to find signs of infection and to check kidney function. They may also show the gene that caused your child's CF.
- An x-ray will show inflammation and enlargement of your child's lungs. It will also show plugged airways and any fluid buildup.
- A bronchoscopy is a procedure to look inside your child's lungs to check for damage. A bronchoscope (thin tube with a light) is inserted into the mouth and moved down the throat to the lungs. Tissue and fluid may be collected from your child's lungs to be tested.
How is CF treated?
CF cannot be cured. Treatment may help your child breathe more easily, prevent infections, or absorb nutrients.
- Medicines:
- Antibiotics help fight or prevent an infection caused by bacteria.
- Mucus-thinning medicine is breathed in to help thin lung mucus so it can be coughed up more easily.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Steroids help decrease inflammation.
- Bronchodilators help open the air passages in your child's lungs.
- Pancreatic enzymes help your child's digestive system break down food and absorb nutrients.
- Cystic fibrosis transmembrane regulators (CFTR) may help improve your child's symptoms if the CF is caused by a certain protein mutation. Your child's healthcare provider or CF specialist can give you more information about CFTRs.
- Extra oxygen may be needed if your child's blood oxygen level is lower than it should be. He or she may get oxygen through a mask placed over the nose and mouth or through small tubes placed in the nostrils.
- Surgery may be needed if your child has severe damage to organs, such as his or her liver or lungs. Ask your child's healthcare provider for more information about surgery.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Drugs used to treat this and similar conditions
Pulmozyme
Pulmozyme is used to improve lung function in people with cystic fibrosis. Learn about side ...
Creon
Creon (pancrelipase) contains digestive enzymes and is used to improve food digestion in people who ...
Botox
Botox is used to treat chronic migraines, excessive sweating, bladder conditions, eye muscle ...
Kalydeco
Kalydeco (ivacaftor) is used to treat cystic fibrosis in adults and children who are at least 4 ...
Trikafta
Trikafta is used to treat adults and children aged 2 years and older with cystic fibrosis (CF) with ...
Cayston
Cayston (aztreonam inhalation) is used to improve breathing symptoms in cystic fibrosis patients ...
Zenpep
Zenpep (pancrealipase) is used to replace pancreatic enzymes when the body does not have enough of ...
What can I do to help my child breathe more easily?
- Have your child do airway clearance exercises to help remove mucus. Your child's healthcare provider will show him or her how to do the exercises. These exercises may be used with machines or devices to decrease your child's symptoms and risk for infection.
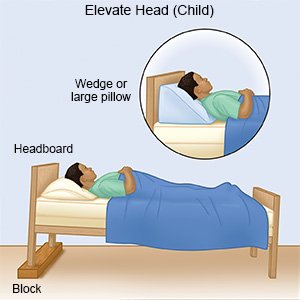
- Elevate your child's head when he or she sleeps. Your child may have trouble breathing when he or she lies flat. Use pillows or foam wedges to elevate his or her head. Do not use pillows with a baby.
- Have your child be physically active, as directed. Ask your child's healthcare provider about the best physical activity plan for your child. Physical activity can help loosen secretions in your child's airways and lungs.

- Do not smoke around your child. Nicotine and other chemicals in cigarettes and cigars can cause lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
What can I do to help my child stay healthy?
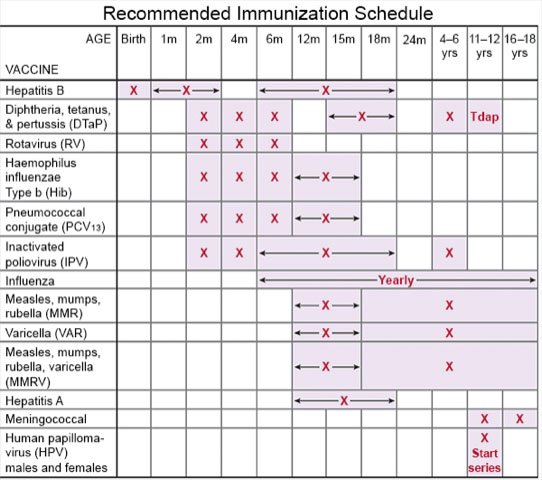
- Ask about vaccines your child may need. Take your child to get a flu vaccine as soon as recommended each year, usually in September or October. Your child should also get a COVID-19 vaccine and recommended boosters. Ask if your child needs other vaccines, and when to get them.
- Prevent the spread of germs. Cover your child's mouth when he or she coughs. Teach him or her to cough into a tissue or the bend of his or her elbow.
- Wash your hands and your child's hands often. Use soap and water. Carry germ-killing gel with you when soap and water are not available. Teach your child to avoid touching his or her eyes, nose, or mouth unless he or she has washed his or her hands first.

- Give your child a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Your child may need to eat foods that have extra calories, fat, vitamins, or calcium. Ask your child's healthcare provider if your child needs to be on a special diet.

- Take your child for screening tests as directed. Screening means your child is checked for complications of CF before he or she shows symptoms. Your child may be screened for CF-related diabetes at least 1 time each year starting at age 10. Your child's provider will tell you which tests your child may need, and how often the tests should be done.
Call your local emergency number (911 in the US) if:
- Your child coughs up blood.
- Your child has trouble breathing.
When should I seek immediate care?
- Your child's lips or fingernails turn blue or white.
- Your child has severe abdominal pain.
When should I call my child's doctor?
- Your child has a fever.
- Your child has chills or feels weak or achy.
- Your child has trouble sleeping.
- Your child urinates less, has a dry mouth or cracked lips, or feels dizzy.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Cystic Fibrosis
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
