Clotting Disorders during Pregnancy
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What do I need to know about clotting disorders during pregnancy?
Pregnancy increases your risk for venous thromboembolism (VTE). A VTE is a blood clot (thrombus) that has formed in a vein. A VTE can form anywhere in your body and block blood flow. A VTE in the deep veins in the calfs, thighs, pelvis, or arms is called a deep venous thrombosis (DVT). A piece of the clot may break loose. This is called an embolus. The embolus can travel to your lungs and cause a life-threatening pulmonary embolism (PE). The 6 weeks after delivery is also a period of increased risk. A condition with abnormal clotting of your blood (thrombophilia) can develop on its own. It can also be inherited. Thrombophilia also increases your risk for VTE. Thrombophilia puts you at risk for problems during pregnancy such as preeclampsia and miscarriage.
What increases my risk for clotting disorders while I am pregnant?
- Past blood clots
- Family history or a condition such as Factor V Leiden mutation
- Older age at pregnancy
- Obesity
- Smoking
- Cesarean section
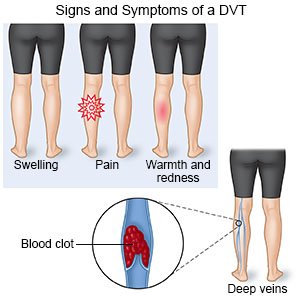
What are the signs and symptoms of a VTE or DVT?
Your symptoms will depend on the location of the clot. You may have any of the following:
- Swelling
- Redness
- Warmth, pain, or tenderness
 |
What are the signs and symptoms of a PE?
- Sudden shortness of breath or fast breathing
- Sudden chest pain that is worse when you take a deep breath
- Fast heartbeat
- Fever and coughing up blood
- Bluish nails
- Cold, pale, clammy skin
- Fainting
How are clotting disorders diagnosed?
Your healthcare provider may recommend screening if your risk for a clotting disorder is high. Screening may include tests to check for a clotting disorder or for a blood clot. Any of the following may be used:
- Blood tests may be used to check how well your blood clots. Genetic tests may also be available. These check for conditions such as Factor V Leiden mutation that increase the risk for clots.
- An ultrasound may show a clot in your vein.
- An MRI may be used if ultrasound pictures did not show a clot but your risk for a DVT continues. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- Contrast venography is an x-ray of a vein. Contrast liquid is used to make the vein easier to see on the x-ray. Tell a healthcare provider if you have ever had an allergic reaction to contrast liquid.
How are clotting disorders treated while I am pregnant?
Anticoagulant medicines such as heparin may be needed throughout your pregnancy. You may also need the medicine for a short time after you give birth.
How can I prevent blood clots?
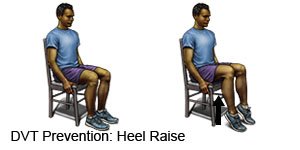
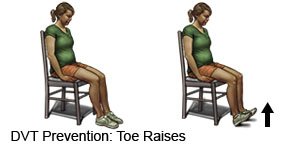
- Change your body position or move around often. Move and stretch in your seat several times each hour if you travel by car or work at a desk. In an airplane, get up and walk every hour. Move your legs by tightening and releasing your leg muscles while sitting. You can move your legs while sitting by raising and lowering your heels. Keep your toes on the floor while you do this. You can also raise and lower your toes while keeping your heels on the floor.
- Maintain a healthy weight. Ask your healthcare provider how much weight you should gain during pregnancy. Ask him or her to help you create a food plan to help you stay within his or her guidelines.
- Drink plenty of liquids. Liquids help keep blood vessels working properly. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you. Do not drink caffeine or alcohol. Blood vessels become narrow with caffeine and alcohol. Narrowed vessels increase your risk for blood clots. Your baby can have problems if you drink alcohol while you are pregnant.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can damage blood vessels and make it more difficult to prevent a blood clot. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Call your local emergency number (911) in the US if:
- You have sudden shortness of breath.
- You have chest pain that gets worse with a deep breath.
- You are lightheaded or you pass out.
- You have bleeding that does not stop after 10 minutes of holding pressure on the area.
When should I seek immediate care?
- You have signs of a miscarriage:
- Vaginal spotting or heavy bleeding
- Pain or cramping in your abdomen or lower back
- Discharge of bloody fluid, tissue, or blood clots from your vagina
- Nausea or vomiting
- Dizziness
When should I call my doctor or obstetrician?
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
