Chronic Wounds
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a chronic wound?
A chronic wound is a wound that does not heal completely in 6 weeks. A wound is an injury that causes a break in the skin. There may also be damage to nearby tissues. Examples of wounds that can become chronic are deep ulcers (open sores), large burns, and infected cuts.
What leads to a chronic wound?
Conditions that slow or stop the healing process may lead to a chronic wound. These may include any of the following:
- Poor blood supply or low oxygen can be caused by low blood pressure, or blocked or narrowed blood vessels. This is more likely if you smoke or have heart or blood vessel disease. Blood, heart, kidney, and lung disease can also decrease the oxygen supply to tissues.
- An infection occurs when bacteria get into your wound. Objects in the wound, such as glass or metal, may bring bacteria into your wound. Dead tissue in your wound may give bacteria a place to grow. Diseases such as diabetes can also increase your risk for infection.
- A weak immune system may lead to a chronic wound. Radiation treatments, poor nutrition, and certain medicines, such as steroids, weaken the immune system. Diseases such as cancer and diabetes can weaken your immune system and make it hard to fight an infection.
- Swelling in the tissues around your wound can cause pressure that decreases blood flow to the area. Tissue swelling may happen with traumatic injuries. It can also happen with conditions that cause decreased blood flow to the area, such as heart failure or blood vessel problems.
What signs and symptoms may happen with a chronic wound?
- Fever
- The area around your wound is red and warm to the touch
- Milky, yellow, green, or brown pus in the wound
- Bleeding, swelling, or pain in the affected area
- Trouble moving the affected area
- Wound has become larger or deeper
- Dark or black skin around the wound
How is a chronic wound diagnosed?
Your healthcare provider will ask about your wound. Your provider will ask about your health, the medicines you take, and any past surgeries. Your provider will examine the wound and the area around it. Your provider will check to see how deep the wound is and look for signs of infection. You may also need any of the following:
- Blood tests are done to see if you have an infection.
- A wound culture is a test of fluid or tissue used to find the cause of your infection.
- An x-ray is a picture of your bones and tissues in the wound area. You may need to have an x-ray if the wound is near a joint or bone. Healthcare providers look for broken bones, or foreign objects such as glass or metal.
How is a chronic wound treated?
Your treatment depends on where your wound is located and how severe it is. If a medical condition such as diabetes is delaying wound healing, it is important to treat the condition. Healthcare providers may change your treatment over time if your wound still does not heal. Your treatment may also change as your wound heals. You may need any of the following:
- Antibiotics may be given to prevent or treat an infection caused by bacteria.
- Wound care:
- Cleansing is done by flushing the wound with sterile fluid. Healthcare providers may use a large syringe with a needle or catheter (tube) tip. They may also use a liquid that kills germs.
- Debridement is done to remove anything from the wound that can delay healing and lead to infection. This includes dead tissue, and objects such as small rocks and dirt. Your healthcare provider may cut out the damaged areas in or around the wound. Your provider may also drain the wound to clean out pus. Moist bandages may be placed inside the wound, or bandages that contain enzymes may be used. Hydrotherapy (whirlpool treatment) uses water to clean wounds. It may be used to clean and debride burn wounds.
- Dressings are used to protect the wound and promote wound healing. Many kinds of dressings can be used for chronic wounds. An elastic bandage may be wrapped around the wound area to put light pressure on it. The light pressure helps to decrease swelling in tissues around the wound area. Dressings may be in the form of bandages, gauze, films, gels, or foams. They may contain substances to help your wound heal faster.
- Negative pressure wound therapy (NPWT) may also be done. This therapy is also called wound vacuum, or wound vac therapy. A vacuum device uses suction to remove fluid and waste from your wound and pull the edges closer together. NPWT may also increase blood flow and new tissue growth in the wound.

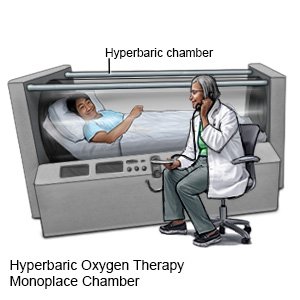
- Hyperbaric oxygen therapy is used to get more oxygen into the area of the wound. The oxygen is given under pressure inside a pressure chamber. You may need to have this therapy more than 1 time.
What do I need to know about wound care?
- Wash your hands before and after you take care of your wound.

- Keep the bandage clean and dry. Do not stop using the bandage on your wound unless your healthcare provider says it is okay.
- Clean the wound and change the dressing as often as directed by your provider.
What can I do to help my wound heal?
- Eat healthy foods and drink liquids as directed. Healthy foods give your body the nutrients it needs to heal your wound. Liquids prevent dehydration that can decrease the blood supply to your wound. Healthy foods include fruits, vegetables, grains (breads and cereals), dairy, and protein foods. Protein foods include meat, fish, nuts, and soy products. Protein, calories, vitamin C, and zinc help wounds heal. Ask your healthcare provider for more information about the foods you should eat to improve healing.
- Do not smoke. If you smoke, it is never too late to quit. Smoking delays wound healing. Smoking also increases your risk for infection after surgery. Ask your provider for information if you need help quitting.
How can I prevent wounds caused by pressure?
Pressure wounds can develop when blood flow to an area is blocked. For example, you sit or lie in the same position without moving and put pressure on your heels. You can prevent pressure wounds by doing any of the following:
- Change your position every 15 minutes while you are sitting.
- Change your position every 2 hours while you lie in bed.
- Prop your legs on pillows to lift your heels while you are lying down.
- Check your skin or have someone else check your skin daily. Check the areas that are common to pressure wounds, such as elbows, heels, and buttocks. Common early signs of pressure wounds are open sores, blisters, or changes in color or temperature.
Drugs used to treat this and similar conditions
Tresiba
Tresiba (insulin degludec) is used to treat diabetes mellitus. Includes Tresiba side effects ...
Humalog
Humalog (insulin lispro) is used to treat type 1 (insulin-dependent) diabetes in adults. Includes ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Crestor
Crestor (rosuvastatin) is used to treat high cholesterol and high triglycerides in the blood ...
Eliquis
Eliquis (apixaban) is used to reduce the risk of stroke and systemic embolism in patients with ...
Lantus
Lantus is a long acting form of insulin used to treat type 1 or type 2 diabetes. Learn about side ...
Sodium bicarbonate
Sodium bicarbonate systemic is used for acidosis, alkylating agent cystitis, asystole, diabetic ...
Rosuvastatin
Rosuvastatin is a prescription medication used to treat high cholesterol and prevent heart disease ...
When should I call my doctor?
- You have a fever.
- You have increased or new pain, swelling, redness, or bleeding in or around your wound.
- You have pus or a foul odor coming from your wound.
- Your skin itches or has a rash.
- You have open sores, blisters, or changes in the color or temperature of your skin.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
