Tiotropium (Monograph)
Brand names: Spiriva Handihaler, Spiriva Respimat
Drug class: Antimuscarinics/Antispasmodics
VA class: RE105
Chemical name: di-2-thienylglycolate-6β,7β-Epoxy-3β-hydroxy-8-methyl-1αH,5αH-tropanium bromide
Molecular formula: C19H22BrNO4S2
CAS number: 139404-48-1
Introduction
Bronchodilator; a synthetic quaternary ammonium antimuscarinic agent.
Uses for Tiotropium
COPD
Tiotropium alone (as oral inhalation powder or solution) or tiotropium/olodaterol fixed-combination therapy (as oral inhalation solution): Long-term maintenance treatment of reversible bronchospasm associated with COPD, including chronic bronchitis and emphysema.
Tiotropium alone (as oral inhalation powder or solution): Reduction of COPD exacerbations in patients with a history of exacerbations.
A long-acting bronchodilator (e.g., orally inhaled salmeterol, formoterol, tiotropium) or an inhaled corticosteroid recommended for maintenance monotherapy in patients with moderate to severe COPD (e.g., FEV1 30 to <80% of predicted or, alternatively, <60% of predicted) who have persistent symptoms not relieved by as-needed therapy with a selective, short-acting inhaled β2-adrenergic agonist. Maintenance therapy with long-acting bronchodilators in such patients more effective and more convenient than regular therapy with short-acting bronchodilators. Insufficient data to favor one maintenance monotherapy over another in patients with moderate to severe COPD. In selected patients with inadequate response, may use a combination of several long-acting bronchodilators, such as tiotropium, and a long-acting β2-adrenergic agonist.
In patients with severe to very severe COPD (e.g., FEV1 <30 to <50% of predicted), some clinicians recommend addition of an inhaled corticosteroid to one or more long-acting bronchodilators, given separately or in fixed combination; however, benefits of combination therapy over monotherapy not consistently established. If inadequate response or limiting adverse effects occur, may consider the addition or substitution of extended-release oral theophylline.
Tiotropium alone (as oral inhalation powder or solution) or tiotropium/olodaterol fixed-combination therapy (as oral inhalation solution): Not indicated for initial treatment of acute episodes of bronchospasm or acute deterioration of COPD; a drug with a more rapid onset of action (e.g., a short-acting β-adrenergic agonist) preferred.
Asthma
Tiotropium alone (as oral inhalation solution): Long-term maintenance treatment of reversible bronchospasm associated with asthma.
Tiotropium oral inhalation solution: Not indicated for treatment of acute episodes of bronchospasm.
Tiotropium/olodaterol fixed-combination therapy: Not indicated for treatment of asthma.
Tiotropium Dosage and Administration
Administration
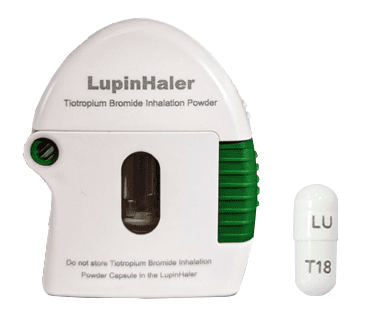
Administer tiotropium powder by oral inhalation only using a special oral inhalation device (HandiHaler) that delivers powdered drug from capsules. Do not take capsules orally, as intended effects on the lungs will not be obtained.
Administer tiotropium solution by oral inhalation only using a specific inhaler (Spiriva Respimat) that delivers a metered-dose spray.
Administer tiotropium/olodaterol in fixed combination by oral inhalation only using a specific inhaler (Stiolto Respimat) that delivers a metered-dose spray.
Spiriva Respimat and Stiolto Respimat inhalers deliver the drugs in an aqueous solution and mechanically produce a fine aerosol mist from the orally inhaled solutions.
Administer tiotropium or tiotropium/olodaterol orally inhaled solutions once daily at the same time every day.
In patients with asthma receiving orally inhaled tiotropium solution, may take 4–8 weeks to achieve maximum clinical benefit.
Oral Inhalation Powder
Open the dust cap by pressing the green piercing button. Pull the dust cap upward on the side opposite the hinge of the Handihaler device to expose the mouthpiece. Open the mouthpiece by pulling the mouthpiece ridge upward on the side opposite the hinge of the inhaler to expose the center chamber. Carefully open the blister card to expose only one capsule immediately before use. Capsule contains only a small amount of powder; do not open. Place capsule into the center chamber of the inhaler, and close the inhaler mouthpiece firmly until it snaps (clicks) into position, leaving the dust cap open (up). (See Stability.) Push down on the mouthpiece ridge to make sure that the mouthpiece is seated in the gray base of the inhaler. Hold the inhaler with the seated mouthpiece upward, depress the green button on the side of the inhaler completely (until the button is flush with the gray base of the inhaler), then release the button. The green button pierces the capsule and disperses the powdered drug upon inspiration. Do not press the green piercing button more than once. Do not shake the Handihaler device. Piercing the capsule may produce small gelatin pieces, which may pass into the mouth or throat; gelatin pieces not expected to cause any harm.
Exhale completely; do not exhale into the HandiHaler device. Hold the inhaler by the gray base; take care not to block the air intake vents near the mouthpiece ridge. With the head kept level, place the mouthpiece of the inhaler between the lips (inhaler is in a horizontal position) and inhale deeply and slowly through the inhaler with a rate sufficient to hear or feel the loaded capsule vibrate (rattle). Pressure from inhalation will disperse the drug from center chamber into air stream created by the patient’s inhalation. Continue breathing until the lungs are full. Remove the inhaler from the mouth and hold the breath for a few seconds, then resume normal breathing. Breathe out completely and inhale once again (from the same capsule) to ensure full delivery of the powder. Do not press the green piercing button again. Upon completion of the second inhalation, open the mouthpiece and tip the device to dispose of the used capsule; close the mouthpiece and dust cap of the inhaler device.
Do not take extra doses despite not being able to hear or feel the capsule vibrate. Tap the inhaler device on a table, holding the gray base in an upright position. Then check to see that the mouthpiece is properly seated in the gray base and attempt to inhale through the device again. If vibration still cannot be felt or heard, throw away the capsule, lift the green piercing button to open the base of the device, and check the center chamber for pieces of the capsule. Turn the device upside down and gently but firmly tap to remove any capsule pieces, then call clinician for instructions. (See Advice to Patients.)
If no improvement in COPD symptoms, make sure patient is inhaling the drug using the oral inhaler rather than swallowing the dry-powder capsules. (See Accidental Oral Ingestion under Cautions.)
Clean the Handihaler device as needed. Open the dust cap and mouthpiece, then open the base by lifting the green piercing button; look in the center chamber for any capsule pieces or powder buildup and tap out if present. Rinse device with warm water (do not use cleaning agents or detergents), pressing the green piercing button a few times so that the center chamber and piercing needle are under the running water; check that remaining powder or capsule pieces are removed. Dry the inhaler well by tipping excess water out on a paper towel; leave dust cap, mouthpiece, and gray base open by fully spreading it out to air dry for 24 hours. Do not use a hair dryer to dry the device. Do not use the inhaler when wet. If needed, clean the outside of the mouthpiece with a clean, damp cloth.
Oral Inhalation Solution
Before first use of either Spiriva Respimat or Stiolto Respimat, place inhaler cartridge into inhaler. Consult the manufacturer's prescribing information for detailed information on inhaler preparation. Write discard date (3 months after cartridge is inserted into inhaler) on inhaler label.
Prime inhaler before first use by turning clear base in direction of black arrows on label until click is heard (one-half turn) with inhaler upright and cap closed. Flip cap until it fully snaps open, then point inhaler away from face, press dose release button, then close cap.
Repeat these steps until spray is visible, then for 3 additional times. Repeat initial actuation step of priming process (without 3 additional repetitions) after periods of nonuse (i.e., for >3 days). If inhaler is not used for >21 days, repeat entire priming process.
To administer a dose, hold inhaler upright with cap closed; turn clear base in direction of black arrows on label until click is heard (one-half turn). Flip cap until it snaps fully open.
Before inhaling dose, exhale slowly and completely. Close lips around end of mouthpiece without covering air vents. Pointing inhaler toward back of throat, press dose release button while taking a slow, deep inhalation through the mouth, continuing to inhale for as long as possible. Hold the breath for 10 seconds (or as long as comfortable). Repeat procedure once more to administer a full dose (2 inhalations), then close cap.
Using only a damp tissue or cloth, clean mouthpiece of the inhaler, including metal part inside, at least once weekly. Outside of inhaler can be wiped with a damp cloth. Inhaler function not affected by minor mouthpiece discoloration.
Dosage
Available as tiotropium bromide monohydrate; dosage expressed in terms of anhydrous tiotropium.
Each capsule of the Spiriva Handihaler contains 18 mcg of tiotropium as an inhalation powder. However, the precise amount of drug delivered to the lungs depends on factors such as the patient’s inspiratory flow.
Each actuation of the Spiriva Respimat inhaler delivers 1.56 or 3.1 mcg of tiotropium bromide monohydrate (equivalent to 1.25 or 2.5 mcg of tiotropium, respectively) per metered spray.
Each actuation of the Stiolto Respimat inhaler delivers 3.1 mcg of tiotropium bromide monohydrate (equivalent to 2.5 mcg of tiotropium) and 2.7 mcg of olodaterol hydrochloride (equivalent to 2.5 mcg of olodaterol) per metered spray.
Precise amount of drug delivered to lungs depends on factors (e.g., patient's coordination between actuation of the inhaler and inspiration through the delivery system). Respimat inhaler mechanically releases dose; delivered dose not dependent on patient's inspiratory effort.
Commercially available inhaler delivers 60 metered sprays equivalent to 30 doses (2 actuations per dose) of the drug.
Pediatric Patients
Asthma
Oral Inhalation
Tiotropium solution in patients ≥6 years of age: 2.5 mcg (2 inhalations of 1.25 mcg per metered spray) once daily.
Adults
COPD
Oral Inhalation
Tiotropium powder: 18 mcg (contents of one capsule) once daily.
Tiotropium solution: 5 mcg (2 inhalations of 2.5 mcg per metered spray) once daily.
Tiotropium/olodaterol fixed-combination therapy: 5 mcg of tiotropium and 5 mcg of olodaterol (2 inhalations) once daily.
Asthma
Oral Inhalation
Tiotropium solution: 2.5 mcg (2 inhalations of 1.25 mcg per metered spray) once daily.
Special Populations
Hepatic Impairment
No dosage adjustments required.
Renal Impairment
No dosage adjustments required.
Geriatric Patients
No dosage adjustments required.
Cautions for Tiotropium
Contraindications
-
Known hypersensitivity to tiotropium bromide, ipratropium, or any ingredient in the formulation.
Warnings/Precautions
Sensitivity Reactions
Immediate hypersensitivity reactions, such as angioedema (e.g., swelling of lips, tongue, throat), urticaria, rash, bronchospasm, anaphylaxis, itching, reported. If such reactions occur, discontinue immediately and consider alternative therapy. Closely monitor patients with history of hypersensitivity reactions to atropine for such reactions. Use tiotropium oral inhalation powder (Spiriva HandiHaler) with caution in patients with severe hypersensitivity to milk proteins.
Use of Fixed Combinations
When used in fixed combination with olodaterol, consider the cautions, precautions, contraindications, and interactions associated with olodaterol.
Acute Bronchospasm
Delayed onset of action; not indicated for initial treatment. Do not use for the treatment of acute episodes of bronchospasm (i.e., as rescue therapy).
Possible Increased Risk of Stroke, Mortality, and/or Cardiovascular Events
Data are conflicting; possible increased risk of stroke identified from ongoing safety monitoring and pooled analysis of placebo-controlled trials. Data on approximately 13,500 patients with COPD suggest an absolute excess risk of 2 strokes per 1000 patient-years with exposure to tiotropium compared with that of placebo. Other observational data involving over 32,000 patients and pooled analyses of almost 15,000 patients suggest an increased risk of mortality and/or cardiovascular events with use of inhaled anticholinergic agents, including tiotropium bromide.
Increased risk of stroke, MI, or death with tiotropium not revealed in a placebo-controlled trial (Understanding Potential Long-term Impacts on Function with Tiotropium [UPLIFT]) in patients with COPD. FDA concluded that available data do not support an association between use of tiotropium inhalation powder and an increased risk of stroke, MI, or cardiovascular death.
All-cause mortality similar in patients with previous cardiac disease receiving tiotropium oral inhalation powder and those receiving tiotropium oral inhalation solution in a long-term, randomized, double-blind, double-dummy, active-controlled trial (Tiotropium Safety and Performance in Respimat [TIOSPIR]).
Increases in corrected QT (QTc) interval reported in patients receiving tiotropium oral inhalation powder.
Paradoxical Bronchospasm
Possible acute paradoxical bronchospasm. Treat immediately with a short-acting inhaled β2-adrenergic agonist; discontinue tiotropium and consider alternative therapy.
Ocular Effects
May worsen angle-closure glaucoma; use with caution in patients with this condition. If signs or symptoms of acute angle-closure glaucoma (e.g., ocular pain/discomfort, blurred vision, visual halos, colored images in association with conjunctival congestion and corneal edema) occur, consult clinician immediately. (See Advice to Patients.) Miotic eye drops alone not considered effective treatment for this condition.
Possible temporary blurred vision or pupillary dilation following inadvertent contact of tiotropium with the eyes. (See Advice to Patients.)
GU Effects
Possible urinary retention, urinary difficulty, or urinary tract infection.
May worsen symptoms and signs of urinary retention, especially in patients with prostatic hyperplasia or bladder neck obstruction. If such signs and/or symptoms occur, immediately consult clinician. Use with caution in patients with urinary retention.
Accidental Oral Ingestion
Acute intoxication unlikely following inadvertent oral ingestion of the dry-powder capsules for oral inhalation since the drug is not well absorbed systemically. Adverse effect reports uncommon following ingestion of dry-powder capsules.
Specific Populations
Pregnancy
Category C.
Limited data on tiotropium use during pregnancy inadequate to inform of drug-associated risk.
Poorly or moderately controlled asthma during pregnancy may increase maternal risk of preeclampsia and infant's risk for prematurity, low birth weight, and small size for gestational age. Closely monitor level of asthma control in pregnant women and adjust therapy as needed to maintain optimal control.
No evidence of structural abnormalities in animal studies. Tiotropium administration resulted in fetal resorption, fetal loss, decreased pup weight and survival in rats receiving higher than the maximum recommended human daily inhalation dosage. In pregnant rabbits, tiotropium administration resulted in increased postimplantation fetal loss at dosages higher than the maximum recommended human daily inhalation dosage.
Lactation
Distributed into milk in rodents; not known whether tiotropium is distributed into human milk. Effects of the drug on breast-fed infants or milk production also not known. Consider benefits of breast-feeding and woman's clinical need for tiotropium along with any potential adverse effects on the breast-fed infant from the drug or from the underlying maternal condition. Use caution.
Pediatric Use
Safety and efficacy of tiotropium oral inhalation powder not established in children <18 years of age.
Safety and efficacy of tiotropium oral inhalation solution for treatment of asthma established in pediatric patients 6–17 years of age in several clinical trials up to 1 year's duration. Safety and efficacy of the drug in these pediatric patients were similar to the effects in patients ≥18 years of age with asthma receiving the drug.
Safety and efficacy of tiotropium oral inhalation solution not established in children <6 years of age.
Geriatric Use
Possible increased incidence of dry mouth, constipation, and urinary tract infection compared with younger adults. However, no overall differences in efficacy relative to younger adults.
Hepatic Impairment
Pharmacokinetics not evaluated.
Renal Impairment
Clearance may be decreased; closely monitor patients with moderate to severe renal impairment (CLcr of <60 mL/minute) for anticholinergic effects during therapy.
Common Adverse Effects
Tiotropium oral inhalation powder: Upper respiratory tract infection, dry mouth, sinusitis, pharyngitis, urinary tract infection, chest pain (nonspecific), rhinitis, dyspepsia, headache, abdominal pain, edema (dependent), arthralgia, constipation, depression, insomnia, vomiting, infection, moniliasis, epistaxis, myalgia, rash.
Tiotropium oral inhalation solution in patients with COPD: Pharyngitis, cough, dry mouth, sinusitis.
Tiotropium oral inhalation solution in patients with asthma: Pharyngitis, headache, bronchitis, sinusitis.
Tiotropium/olodaterol oral inhalation solution (in fixed combination): Nasopharyngitis, cough, back pain.
Drug Interactions
Metabolized by CYP isoenzymes, principally CYP2D6 and CYP3A4.
Does not inhibit CYP1A1, 1A2, 2B6, C29, 2C19, 2D6, 2E1, or 3A4.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β2-Adrenergic agonists |
No adverse drug interactions reported |
|
|
Antihistamines |
No adverse drug interactions reported |
|
|
Anti-IgE monoclonal antibody therapy |
No adverse drug interactions reported |
|
|
Antimuscarinic agents |
Potential increase in anticholinergic effects |
Concomitant use not recommended by manufacturer |
|
Corticosteroids, oral and inhaled |
No adverse drug interactions reported |
|
|
Histamine H2-receptor antagonists |
Increased AUC and decreased renal clearance of IV tiotropium (not currently available in the US) with concomitant cimetidine but not ranitidine |
Pharmacokinetic interactions not considered clinically important |
|
Leukotriene modifiers |
No adverse drug interactions reported |
|
|
Mast-cell stabilizers |
No adverse drug interactions reported. |
|
|
Methylxanthines |
No adverse drug interactions reported |
|
|
Mucolytic agents |
No adverse drug interactions reported |
Tiotropium Pharmacokinetics
Absorption
Bioavailability
Oral inhalation powder: Following inhalation, absolute bioavailability is 19.5%. Most of a dose is swallowed and minimally absorbed into systemic circulation; the fraction reaching the lungs appears to be readily absorbed. Peak plasma concentrations following oral inhalation attained within 7 minutes. Steady state achieved after 7 days of daily administration, with no accumulation thereafter, in patients with COPD.
Oral inhalation solution: Following inhalation, absolute bioavailability is approximately 33%. Peak plasma concentrations following oral inhalation attained within 5–7 minutes. Steady state achieved after 7 days of daily administration, with no accumulation thereafter, in patients with COPD or asthma.
In patients with COPD, once daily administration of oral inhalation powder (18 mcg) or oral inhalation solution (5 mcg) resulted in similar systemic exposure.
Drug exposure similar in pediatric patients (6–17 years of age) and adults with asthma receiving oral inhalation solution.
Onset
Following oral inhalation of tiotropium powder, bronchodilation evident within 30 minutes.
Duration
Bronchodilation generally persists for >24 hours.
Food
Food does not appear to affect absorption from GI tract.
Special Populations
In patients with renal impairment, increased plasma drug concentrations and AUC.
Distribution
Extent
Widely distributed into tissues. Does not penetrate the blood-brain barrier in animals.
Plasma Protein Binding
72%.
Elimination
Metabolism
Metabolized to a limited extent, principally by isoenzymes CYP2D6 and 3A4.
Elimination Route
Oral inhalation powder in healthy individuals: Urinary excretion approximately 14% (principally as unchanged drug).
Oral inhalation powder in patients with COPD: Urinary excretion of unchanged drug 7% over 24 hours.
Oral inhalation solution (5 mcg once daily) in patients with COPD: Urinary excretion of unchanged drug approximately 19% over 24 hours.
Oral inhalation solution (2.5. mcg once daily) in patients with asthma: Urinary excretion of unchanged drug approximately 13% over 24 hours.
Half-life
Terminal elimination half-life following oral inhalation is approximately 25 or 44 hours in patients with COPD or asthma, respectively.
Special Populations
In patients with renal impairment, reduced clearance.
Stability
Storage
Oral Inhalation
Powder
25°C (may be exposed to 15–30°C). Do not expose to extreme temperatures and moisture.
Keep capsules in sealed blisters until immediately before use. Do not store used or unused capsules in the inhaler device. Remove only one capsule immediately before use or effectiveness of the drug may be reduced. Discard additional capsules if opened and exposed to air (i.e., not intended for immediate use).
Solution
Tiotropium: 25°C (may be exposed to 15–30°C); do not freeze. Discard inhaler a maximum of 3 months after first use or when locking mechanism is engaged (no more actuations available), whichever comes first.
Tiotropium/olodaterol in fixed combination: 25°C (may be exposed to 15–30°C); do not freeze. Discard inhaler a maximum of 3 months after first use or when locking mechanism is engaged (no more actuations available), whichever comes first.
Actions
-
Competitively and reversibly inhibits the actions of acetylcholine and other cholinergic stimuli at M3 receptors in the smooth muscle of the respiratory tract, leading to bronchodilation.
Advice to Patients
-
Provide a copy of the manufacturer's patient information (medication guide) and instructions for use to all patients each time drug is dispensed. Importance of instructing patients to read the medication guide prior to initiation of therapy and each time prescription is refilled.
-
Importance of informing a clinician of allergies to any medications prior to initiation of tiotropium bromide therapy.
-
Importance of adequate understanding of proper storage, preparation, and inhalation techniques, including use of the inhalation delivery system (HandiHaler or Respimat).
-
Importance of instructing caregivers to assist children with use of the Respimat inhalation device.
-
Importance of not using the HandiHaleror Respimat device to administer other drugs.
-
Importance of consulting a clinician of faulty inhaler performance (i.e., if capsule vibration is not felt or heard upon inhalation) when certain procedures (i.e., confirming that the mouthpiece is firmly seated in the gray base, tapping the inhaler gently on a table) do not improve inhaler performance.
-
Importance of storing tiotropium dry-powder capsules in sealed blisters and of removing only one capsule immediately before use; discard unused additional capsules that are exposed to air.
-
Importance of avoiding inadvertent contact of the drug with the eyes, as contact may cause blurred vision and pupillary dilation.
-
Importance of not using tiotropium to relieve acute symptoms or exacerbations of asthma or COPD.
-
Importance of advising patients with asthma that maximum benefits may only be apparent after 4–8 weeks of treatment with tiotropium inhalation solution.
-
Risk of immediate hypersensitivity reactions such as anaphylaxis, angioedema (e.g., swelling of the lips, tongue, throat), urticaria, rash, bronchospasm, itching. If such signs and/or symptoms occur, discontinue tiotropium immediately and consult a clinician.
-
Risk of paradoxical bronchospasm. If paradoxical bronchospasm occurs, discontinue tiotropium.
-
Risk of worsening of angle-closure glaucoma. Importance of immediately informing a clinician if eye pain or discomfort, blurred vision, or visual halos or colored images in association with conjunctival congestion or corneal edema occur.
-
Importance of advising patients to use caution when engaging in activities (e.g., driving a vehicle, operating appliances or machinery) since drug may cause dizziness or blurred vision.
-
Risk of worsening of urinary retention. Importance of immediately informing a clinician if symptoms of urinary retention (e.g., dysuria) occur.
-
Importance of keeping drug out of reach of children.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs (e.g., eye drops) and herbal supplements, as well as any concomitant illnesses (e.g., urinary difficulty, enlarged prostate, angle-closure glaucoma).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral Inhalation |
Powder for inhalation (contained in capsules) |
18 mcg (of anhydrous tiotropium) |
Spiriva HandiHaler |
Boehringer Ingelheim (comarketed by Pfizer) |
|
Solution for inhalation |
1.25 mcg (of tiotropium) per metered spray |
Spiriva Respimat |
Boehringer Ingelheim |
|
|
2.5 mcg (of tiotropium) per metered spray |
Spiriva Respimat |
Boehringer Ingelheim |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral Inhalation |
Solution for inhalation |
2.5 mcg (of tiotropium) with Olodaterol Hydrochloride 2.5 mcg (of olodaterol) per metered spray |
Stiolto Respimat |
Boehringer Ingelheim |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 23, 2017. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
More about tiotropium
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (157)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: anticholinergic bronchodilators
- Breastfeeding
Patient resources
- Tiotropium inhalation drug information
- Tiotropium (Advanced Reading)
- Tiotropium Capsules for Inhalation