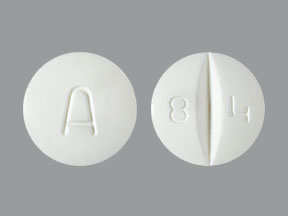
Amiodarone Tablets
Generic name: Amiodarone Tablets [ a-MEE-oh-da-rone ]
Brand names: Cordarone, Pacerone
Drug class: Group III antiarrhythmics
Warning
- This medicine is only used to treat abnormal heartbeats that may be deadly. It may cause severe and sometimes deadly side effects like lung, thyroid, or liver problems. This medicine can also cause the abnormal heartbeats to get worse. If you have questions, talk with the doctor.
- This medicine will be started in a hospital where you will be closely watched. Talk with your doctor.
Uses of Amiodarone Tablets:
- It is used to treat certain types of abnormal heartbeats.
What do I need to tell my doctor BEFORE I take Amiodarone Tablets?
- If you have an allergy to amiodarone, iodine, or any other part of this medicine (amiodarone tablets).
- If you are allergic to this medicine (amiodarone tablets); any part of this medicine (amiodarone tablets); or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had.
- If you have any of these health problems: Certain types of abnormal heartbeats called heart block or sick-sinus syndrome, shock caused by heart problems, or slow heartbeat.
- If you have any of these health problems: Low calcium levels, low magnesium levels, or low potassium levels.
- If you are taking any drugs that can cause a certain type of heartbeat that is not normal (prolonged QT interval). There are many drugs that can do this. Ask your doctor or pharmacist if you are not sure.
- If you take any drugs (prescription or OTC, natural products, vitamins) that must not be taken with this medicine (amiodarone tablets), like certain drugs that are used for hepatitis C, HIV, or infections. There are many drugs that must not be taken with this medicine (amiodarone tablets).
- If you are taking St. John's wort. Do not take St. John's wort with this medicine (amiodarone tablets). This medicine may not work as well.
- If you are breast-feeding. Do not breast-feed while you take this medicine (amiodarone tablets). You may also need to avoid breast-feeding for some time after your last dose. Talk with your doctor to see if you need to avoid breast-feeding after your last dose.
This is not a list of all drugs or health problems that interact with this medicine (amiodarone tablets).
Tell your doctor and pharmacist about all of your drugs (prescription or OTC, natural products, vitamins) and health problems. You must check to make sure that it is safe for you to take this medicine (amiodarone tablets) with all of your drugs and health problems. Do not start, stop, or change the dose of any drug without checking with your doctor.
What are some things I need to know or do while I take Amiodarone Tablets?
- Tell all of your health care providers that you take this medicine (amiodarone tablets). This includes your doctors, nurses, pharmacists, and dentists.
- To lower the chance of feeling dizzy or passing out, rise slowly if you have been sitting or lying down. Be careful going up and down stairs.
- Have blood work checked as you have been told by the doctor. Talk with the doctor.
- Low blood pressure has happened with this medicine (amiodarone tablets). Sometimes this has been deadly. Talk with the doctor.
- Check blood pressure and heart rate as the doctor has told you.
- Have your heart and lung function checked. Talk with your doctor.
- Have an eye exam as you have been told by your doctor.
- Slow heartbeat and the need to get a pacemaker have happened when amiodarone was given with sofosbuvir and certain other hepatitis C drugs. Sometimes, this has been deadly. If you also take drugs for hepatitis C, talk with your doctor.
- If you have a defibrillator or pacemaker, talk with your doctor.
- Avoid grapefruit and grapefruit juice.
- If diarrhea or throwing up happens, talk with the doctor. You will need to make sure to avoid dehydration and electrolyte problems.
- A very bad eye problem has rarely happened with this medicine (amiodarone tablets). This may lead to a change in eyesight and sometimes loss of eyesight, which may not come back. Talk with the doctor.
- You may get sunburned more easily. Avoid sun, sunlamps, and tanning beds. Use sunscreen and wear clothing and eyewear that protects you from the sun.
- This medicine stays in your body for weeks or months even after you stop it. Before you start taking other drugs, be sure to tell your doctor and pharmacist that you have taken this medicine (amiodarone tablets).
- If you are 65 or older, use this medicine (amiodarone tablets) with care. You could have more side effects.
- This medicine may affect fertility. Fertility problems may lead to not being able to get pregnant or father a child.
- This medicine may cause harm to the unborn baby if you take it while you are pregnant. If you are pregnant or you get pregnant while taking this medicine (amiodarone tablets), call your doctor right away.
How is this medicine (Amiodarone Tablets) best taken?
Use this medicine (amiodarone tablets) as ordered by your doctor. Read all information given to you. Follow all instructions closely.
- Take with or without food but take the same way each time. Always take with food or always take on an empty stomach.
- If you take cholestyramine, talk with your pharmacist about how to take it with this medicine (amiodarone tablets).
- Keep taking this medicine (amiodarone tablets) as you have been told by your doctor or other health care provider, even if you feel well.
What do I do if I miss a dose?
- Skip the missed dose and go back to your normal time.
- Do not take 2 doses at the same time or extra doses.
What are some side effects that I need to call my doctor about right away?
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
- Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
- Signs of liver problems like dark urine, feeling tired, not hungry, upset stomach or stomach pain, light-colored stools, throwing up, or yellow skin or eyes.
- Signs of lung or breathing problems like shortness of breath or other trouble breathing, cough, or fever.
- Signs of thyroid problems like change in weight; feeling nervous, excitable, restless, or weak; hair thinning; depression; neck swelling; not able to focus; trouble with heat or cold; menstrual changes; shakiness; or sweating.
- Change in balance.
- Shakiness, trouble moving around, or stiffness.
- Blue or gray skin color.
- Sunburn.
- Coughing up blood.
- Chest pain or pressure.
- A burning, numbness, or tingling feeling that is not normal.
- Fast or slow heartbeat.
- An abnormal heartbeat that is new or worse.
- Change in eyesight, eye pain, or very bad eye irritation.
- If bright lights bother your eyes.
- Dizziness or passing out.
- Trouble controlling body movements.
- Muscle weakness.
- Shortness of breath, a big weight gain, or swelling in the arms or legs.
- Any unexplained bruising or bleeding.
- Lowered interest in sex.
- A very bad skin reaction (Stevens-Johnson syndrome/toxic epidermal necrolysis) may happen. It can cause very bad health problems that may not go away, and sometimes death. Get medical help right away if you have signs like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in your mouth, throat, nose, or eyes.
Related/similar drugs
Cardizem
Cardizem is used to treat hypertension (high blood pressure), angina (chest pain), and heart rhythm ...
Adenocard
Adenocard is used for radionuclide myocardial perfusion study, supraventricular tachycardia ...
Omvoh
Omvoh is used to treat moderate to severe ulcerative colitis or Crohn's disease in adults. This ...
Mexiletine
Mexiletine systemic is used for arrhythmia, diabetic peripheral neuropathy, myotonia congenita ...
Adenosine
Adenosine systemic is used for atrial tachycardia, radionuclide myocardial perfusion study ...
Propafenone
Propafenone systemic is used for atrial fibrillation, atrial flutter, ventricular tachycardia ...
Phenylephrine
Oral and nasal phenylephrine are used as nasal decongestants to temporarily unblock a nose or ...
Verapamil
Verapamil is used to treat hypertension (high blood pressure), angina (chest pain), and certain ...
Flecainide
Flecainide systemic is used for atrial fibrillation, atrial flutter, paroxysmal supraventricular ...
What are some other side effects of Amiodarone Tablets?
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
- Constipation.
- Upset stomach or throwing up.
- Feeling tired or weak.
- Not hungry.
- Stomach pain.
- Headache.
- Trouble sleeping.
- Flushing.
- Change in taste.
- Change in sense of smell.
- More saliva.
These are not all of the side effects that may occur. If you have questions about side effects, call your doctor. Call your doctor for medical advice about side effects.
You may report side effects to the FDA at 1-800-332-1088. You may also report side effects at https://www.fda.gov/medwatch.
If OVERDOSE is suspected:
If you think there has been an overdose, call your poison control center or get medical care right away. Be ready to tell or show what was taken, how much, and when it happened.
How do I store and/or throw out Amiodarone Tablets?
- Store at room temperature.
- Protect from light.
- Keep lid tightly closed.
- Store in a dry place. Do not store in a bathroom.
- Keep all drugs in a safe place. Keep all drugs out of the reach of children and pets.
- Throw away unused or expired drugs. Do not flush down a toilet or pour down a drain unless you are told to do so. Check with your pharmacist if you have questions about the best way to throw out drugs. There may be drug take-back programs in your area.
Consumer Information Use and Disclaimer
- If your symptoms or health problems do not get better or if they become worse, call your doctor.
- Do not share your drugs with others and do not take anyone else's drugs.
- This medicine comes with an extra patient fact sheet called a Medication Guide. Read it with care. Read it again each time this medicine (amiodarone tablets) is refilled. If you have any questions about this medicine (amiodarone tablets), please talk with the doctor, pharmacist, or other health care provider.
- If you think there has been an overdose, call your poison control center or get medical care right away. Be ready to tell or show what was taken, how much, and when it happened.
More about amiodarone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (95)
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
Patient resources
Other brands
Pacerone, Cordarone, Nexterone, Cordarone IV
Professional resources
Other brands
Pacerone, Cordarone, Nexterone
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.