Raynaud's phenomenon
Medically reviewed by Drugs.com. Last updated on Jan 22, 2024.
What is Raynaud's phenomenon?
Raynaud's phenomenon is a blood vessel disorder. The condition is also called Raynaud's disease or Raynaud's syndrome.
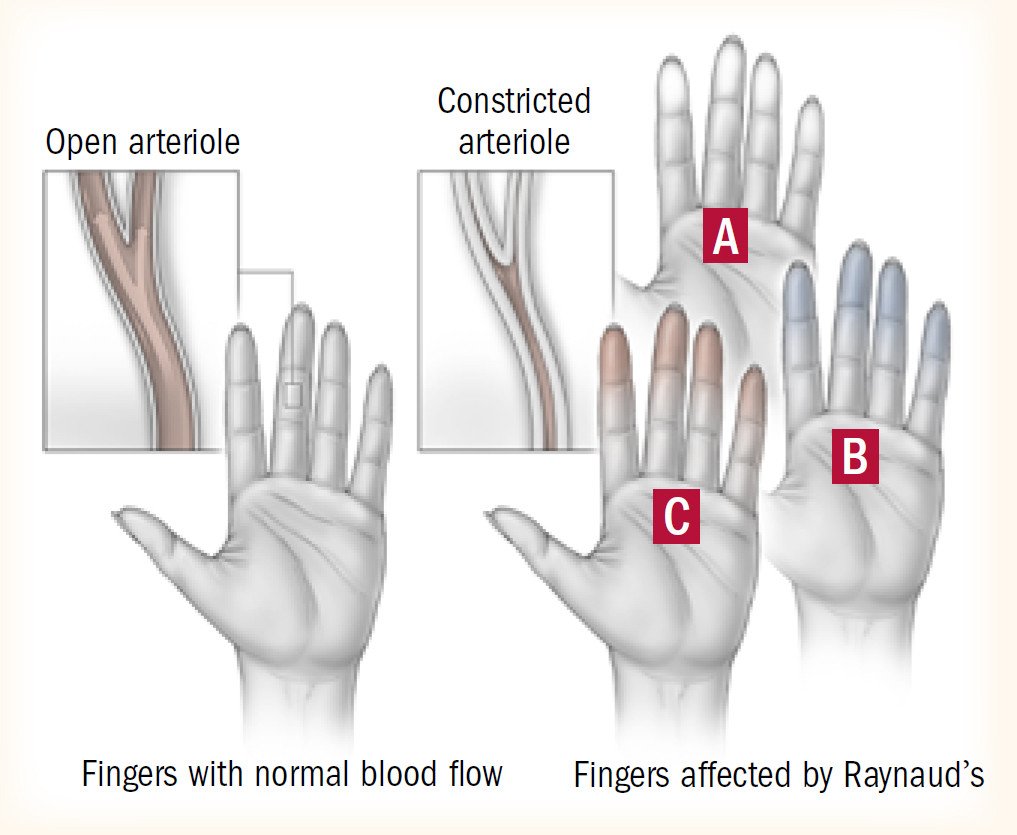
When healthy people are in a cold environment, the tiny blood vessels in their skin constrict, or narrow. This is an effort by the body to conserve heat.
|
In people with Raynaud's phenomenon, that natural response to cold is exaggerated. The tiny blood vessels go into spasm, narrowing and reducing the blood flow to the affected areas. This response, called vasospasm, is seen most often in the fingers and toes. But it also can occur in the ears, cheeks and nose.
In some people, the constriction also can occur in response to emotional stress or a rapid change of temperature from warm to cool. Or, it may occur for no apparent reason.
The effect of this vasospasm can be dramatic and frightening. But it is temporary and rarely dangerous. Once the affected area is warmed, the blood vessels relax and expand. This allows more blood flow.
No one knows what causes Raynaud's phenomenon. People who do not have any other symptoms or disease are said to have primary Raynaud's. People who have Raynaud's as part of another disease are said to have secondary Raynaud's.
Secondary Raynaud's is commonly linked to connective-tissue disorders, such as scleroderma and lupus. It also can result from blood vessel damage due to injury, frostbite or use of jarring machinery, such as jackhammers or chainsaws.
Other causes of secondary Raynaud's include:
- smoking
- medications (especially certain heart and migraine medications) and cocaine
- diseases that affect circulation (such as atherosclerosis).
These factors can also worsen pre-existing Raynaud's.
Symptoms of Raynaud's phenomenon
People with Raynaud's see and feel changes in their fingers and toes when exposed to cold. The skin blanches, or turns white, then blue. Fingers and toes can tingle or feel numb.
When rewarmed, the skin flushes pink or red. And there can be throbbing or soreness as the blood surges back into the tiny blood vessels.
People with secondary Raynaud's often have symptoms related to their underlying rheumatic disease such as
- arthritis
- rash
- a thickening or hardening of the skin.
Diagnosing Raynaud's phenomenon
A physician usually diagnoses Raynaud's based on the patient's description of symptoms.
If other symptoms also are present, blood tests and other procedures may be done to check for other diseases.
More testing also is needed if symptoms are not typical, such as:
- only one finger being affected
- only one hand being affected
- color changes that seem permanent.
These atypical symptoms would be unusual for Raynaud's. They could indicate another problem with circulation.
Careful examination of the nail beds (the skin near the fingernail farthest from the fingertip) may show changes in the blood vessels. These changes may suggest an underlying rheumatic condition such as scleroderma.
Expected duration of Raynaud's phenomenon
Each episode of vasospasm is temporary. However, Raynaud's is considered a chronic (long-lasting) condition.
Preventing Raynaud's phenomenon
There is no way to prevent a person from developing Raynaud's. But once the disorder is present, the number of episodes of vasospasm can be reduced or even eliminated. To do so, avoid situations that can trigger events.
To avoid vasospasm:
- Avoid unnecessary exposure to the cold.
- At home, turn up the thermostat a few degrees.
- In very cold weather, wear a hat and mittens to conserve as much warmth as possible. Mittens protect against cold better than gloves. Use hand warmers and/or foot warmers when in cold environments.
- Bundle up before you head out into the cold, rather than after you are in the cold. This ensures your arms and legs are not shocked by the temperature change.
- Leave your coat, mittens, and hat on while in the freezer or refrigerator section of the grocery store.
- At home, use pot holders, mittens, or a towel to remove items from the refrigerator.
- Use a cup holder when drinking a cold beverage.
- Don't smoke or use cocaine.
- Avoid drugs (if possible) that may worsen vasospasm, such as beta blockers. However, check with your doctor before making any changes to the medicines you take.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Treating Raynaud's phenomenon
Most people with primary Raynaud's disease do not need specific treatment. Their symptoms can be managed by avoiding triggering events as much as possible.
An episode of vasospasm often can be stopped by warming the affected areas. Do this by going indoors or soaking fingers or toes in a bowl of warm (not hot) water.
Biofeedback can help people train the body to warm the extremities. This mind-body method may help you to learn how to gain voluntary control over body processes that are typically involuntary, such as blood flow. It can help some patients to control their symptoms.
For more severe cases (which are more common with secondary Raynaud's), medication may be prescribed to reduce the severity and number of vasospasm episodes. These include:
- calcium channel blockers, such as
- amlodipine (Norvasc)
- diltiazem (Cardizem, Dilacor)
- nifedipine (Procardia, Adalat)
- fluoxetine (Prozac)
- hydralazine (Apresoline)
- losartan (Cozaar)
- nitroglycerin cream or ointment
- prazosin (Minipress)
- sildenafil (Viagra) or tadalafil (Cialis).
In severe cases that do not respond to the above treatments, your doctor may recommend intravenous medications, such as prostacyclin or iloprost. Rarely, your doctor may discuss a surgical procedure to interrupt the nerves that control blood vessel constriction. This procedure is called a sympathectomy.
People with secondary Raynaud's will need to be treated for their underlying disease.
When to call a professional
Call your health care professional if you have symptoms of Raynaud's. Your doctor will tell you more about Raynaud's and will diagnose or rule out associated diseases.
If you have been diagnosed with Raynaud's, see your doctor if you have any unusual symptoms. These include severe redness, inflammation or open sores.
Seek emergency care if you have
- color changes
- numbness or tingling in your arms or legs that does not go away within minutes after the area is warmed.
Prognosis
For most people, primary Raynaud's can be annoying and cause discomfort, but is rarely dangerous. Although it is typically a lifelong condition, it frequently does not get worse. In cases in which the vasospasm is severe, the affected areas may be prone to open sores that are slow to heal.
Raynaud's phenomenon, however, may be the first symptom of a rheumatic disease. So the condition should not be ignored. Patients may need to be examined, tested and monitored to diagnose an associated rheumatic disease at its earliest stage.
Additional info
American College of Rheumatology
http://www.rheumatology.org/
Arthritis Foundation
http://www.arthritis.org/
National Heart, Lung, and Blood Institute (NHLBI)
http://www.nhlbi.nih.gov/
National Institute of Arthritis and Musculoskeletal and Skin Diseases
National Insitutes of Health
http://www.niams.nih.gov/
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
